Related Research Articles

Antidepressants are a class of medications used to treat major depressive disorder, anxiety disorders, chronic pain, and addiction.
An anxiolytic is a medication or other intervention that reduces anxiety. This effect is in contrast to anxiogenic agents which increase anxiety. Anxiolytic medications are used for the treatment of anxiety disorders and their related psychological and physical symptoms.

Psychopharmacology is the scientific study of the effects drugs have on mood, sensation, thinking, behavior, judgment and evaluation, and memory. It is distinguished from neuropsychopharmacology, which emphasizes the correlation between drug-induced changes in the functioning of cells in the nervous system and changes in consciousness and behavior.

Monoamine transporters (MATs) are proteins that function as integral plasma-membrane transporters to regulate concentrations of extracellular monoamine neurotransmitters. The three major classes are serotonin transporters (SERTs), dopamine transporters (DATs), and norepinephrine transporters (NETs) and are responsible for the reuptake of their associated amine neurotransmitters. MATs are located just outside the synaptic cleft (peri-synaptically), transporting monoamine transmitter overflow from the synaptic cleft back to the cytoplasm of the pre-synaptic neuron. MAT regulation generally occurs through protein phosphorylation and post-translational modification. Due to their significance in neuronal signaling, MATs are commonly associated with drugs used to treat mental disorders as well as recreational drugs. Compounds targeting MATs range from medications such as the wide variety of tricyclic antidepressants, selective serotonin reuptake inhibitors such as fluoxetine (Prozac) to stimulant medications such as methylphenidate (Ritalin) and amphetamine in its many forms and derivatives methamphetamine (Desoxyn) and lisdexamfetamine (Vyvanse). Furthermore, drugs such as MDMA and natural alkaloids such as cocaine exert their effects in part by their interaction with MATs, by blocking the transporters from mopping up dopamine, serotonin, and other neurotransmitters from the synapse.

Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of antidepressant medications used to treat major depressive disorder (MDD), anxiety disorders, social phobia, chronic neuropathic pain, fibromyalgia syndrome (FMS), and menopausal symptoms. Off-label uses include treatments for attention-deficit hyperactivity disorder (ADHD), obsessive–compulsive disorder (OCD), and migraine prevention. SNRIs are monoamine reuptake inhibitors; specifically, they inhibit the reuptake of serotonin and norepinephrine. These neurotransmitters are thought to play an important role in mood regulation. SNRIs can be contrasted with the selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), which act upon single neurotransmitters.
Biological psychiatry or biopsychiatry is an approach to psychiatry that aims to understand mental disorder in terms of the biological function of the nervous system. It is interdisciplinary in its approach and draws on sciences such as neuroscience, psychopharmacology, biochemistry, genetics, epigenetics and physiology to investigate the biological bases of behavior and psychopathology. Biopsychiatry is the branch of medicine which deals with the study of the biological function of the nervous system in mental disorders.
Antidepressant discontinuation syndrome, also called antidepressant withdrawal syndrome, is a condition that can occur following the interruption, reduction, or discontinuation of antidepressant medication following its continuous use of at least a month. The symptoms may include flu-like symptoms, trouble sleeping, nausea, poor balance, sensory changes, akathisia, intrusive thoughts, depersonalization and derealization, mania, anxiety, and depression. The problem usually begins within three days and may last for several weeks or months. Rarely psychosis may occur.
Neuromodulation is the physiological process by which a given neuron uses one or more chemicals to regulate diverse populations of neurons. Neuromodulators typically bind to metabotropic, G-protein coupled receptors (GPCRs) to initiate a second messenger signaling cascade that induces a broad, long-lasting signal. This modulation can last for hundreds of milliseconds to several minutes. Some of the effects of neuromodulators include: altering intrinsic firing activity, increasing or decreasing voltage-dependent currents, altering synaptic efficacy, increasing bursting activity and reconfigurating synaptic connectivity.

Olanzapine/fluoxetine is a fixed-dose combination medication containing olanzapine (Zyprexa), an atypical antipsychotic, and fluoxetine (Prozac), a selective serotonin reuptake inhibitor (SSRI). Olanzapine/fluoxetine is primarily used to treat the depressive episodes of bipolar I disorder as well as treatment-resistant depression.
Fluoxetine, sold under the brand name Prozac, among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. It is used for the treatment of major depressive disorder, obsessive–compulsive disorder (OCD), anxiety, bulimia nervosa, panic disorder, and premenstrual dysphoric disorder. It is also approved for treatment of major depressive disorder in adolescents and children 8 years of age and over. It has also been used to treat premature ejaculation. Fluoxetine is taken by mouth.
A serotonin–norepinephrine–dopamine reuptake inhibitor (SNDRI), also known as a triple reuptake inhibitor (TRI), is a type of drug that acts as a combined reuptake inhibitor of the monoamine neurotransmitters serotonin, norepinephrine, and dopamine. It does this by concomitantly inhibiting the serotonin transporter (SERT), norepinephrine transporter (NET), and dopamine transporter (DAT), respectively. Inhibition of the reuptake of these neurotransmitters increases their extracellular concentrations and, therefore, results in an increase in serotonergic, adrenergic, and dopaminergic neurotransmission. The naturally-occurring and potent SNDRI cocaine is widely used recreationally and often illegally for the euphoric effects it produces.

A serotonin reuptake inhibitor (SRI) is a type of drug which acts as a reuptake inhibitor of the neurotransmitter serotonin by blocking the action of the serotonin transporter (SERT). This in turn leads to increased extracellular concentrations of serotonin and, therefore, an increase in serotonergic neurotransmission. It is a type of monoamine reuptake inhibitor (MRI); other types of MRIs include dopamine reuptake inhibitors and norepinephrine reuptake inhibitors.

Seproxetine, also known as (S)-norfluoxetine, is a selective serotonin reuptake inhibitor (SSRI). It is the S enantiomer of norfluoxetine, the main active metabolite of the widely used antidepressant fluoxetine; it is nearly 4 times more selective for stimulating neurosteroid synthesis relative to serotonin reuptake inhibition than fluoxetine. It is formed through the demethylation, or removal of a methyl group, of norfluoxetine. Seproxetine is both an inhibitor of serotonin and dopamine transporters, 5-HT2A and 5-HT2C receptors. It was being investigated by Eli Lilly and Company as an antidepressant; however, it inhibited the KvLQT1 protein, which is responsible for the management of the QT interval. This is the time it takes for the heart to contract and recover. Due to the inhibition, the QT interval was prolonged, which could lead to significant cardiac side complications. Due to this, development of the medication was discontinued. Tests on its efficacy found that it was equivalent to fluoxetine, but sixteen times more powerful than the R enantiomer of norfluoxetine.

Nisoxetine, originally synthesized in the Lilly research laboratories during the early 1970s, is a potent and selective inhibitor for the reuptake of norepinephrine (noradrenaline) into synapses. It currently has no clinical applications in humans, although it was originally researched as an antidepressant. Nisoxetine is now widely used in scientific research as a standard selective norepinephrine reuptake inhibitor. It has been used to research obesity and energy balance, and exerts some local analgesia effects.

Selective serotonin reuptake inhibitors (SSRIs) are a class of drugs that are typically used as antidepressants in the treatment of major depressive disorder, anxiety disorders, and other psychological conditions.
Selective serotonin reuptake inhibitors, or serotonin-specific re-uptake inhibitor (SSRIs), are a class of chemical compounds that have application as antidepressants and in the treatment of depression and other psychiatric disorders. SSRIs are therapeutically useful in the treatment of panic disorder (PD), posttraumatic stress disorder (PTSD), social anxiety disorder, obsessive-compulsive disorder (OCD), premenstrual dysphoric disorder (PMDD), and anorexia. There is also clinical evidence of the value of SSRIs in the treatment of the symptoms of schizophrenia and their ability to prevent cardiovascular diseases.
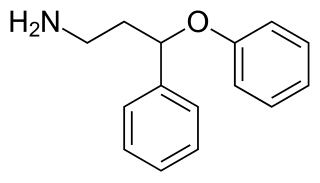
PPPA, or 3-phenoxy-3-phenylpropan-1-amine, is a drug which is described as an antidepressant. It was derived by Eli Lilly from the antihistamine diphenhydramine, a diphenylmethane derivative with additional properties as a selective serotonin reuptake inhibitor (SSRI), and has been the basis for the subsequent discovery of a number of other antidepressant drugs.
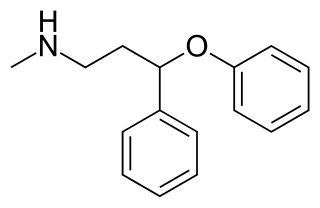
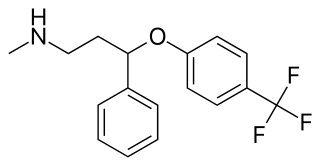
N-Methyl-PPPA, or N-methyl-3-phenoxy-3-phenylpropan-1-amine, is a serotonin-norepinephrine reuptake inhibitor (SNRI) which was developed by Eli Lilly from diphenhydramine in the early 1970s while in search of new antidepressants, but was never marketed. It is closely related structurally to fluoxetine, atomoxetine, and nisoxetine.
Bryan Barnet Molloy was a Scottish chemist, known notably for helping to invent the antidepressant Prozac, a name for fluoxetine. Prozac was introduced in 1988, and has been the world's leading antidepressant.
Selective norepinephrine reuptake inhibitors (sNRIs) are a class of drugs that have been marketed as antidepressants and are used for various mental disorders, mainly depression and attention-deficit hyperactivity disorder (ADHD). The norepinephrine transporter (NET) serves as the fundamental mechanism for the inactivation of noradrenergic signaling because of the NET termination in the reuptake of norepinephrine (NE). The selectivity and mechanism of action for the NRI drugs remain mostly unresolved and, to date, only a limited number of NRI-selective inhibitors are available. The first commercially available selective NRI was the drug reboxetine (Edronax), developed as a first-line therapy for major depressive disorder. Atomoxetine (Strattera) is another potent and selective NRI which is also effective and well tolerated for the treatment of ADHD in adults; it may also be a new treatment option for adults with ADHD, particularly for those patients at risk of substance abuse.
References
- ↑ "Klaus Schmiegel | Lemelson". lemelson.mit.edu. Retrieved 2023-07-06.
- ↑ "Chemical & Engineering News: Top Pharmaceuticals: Prozac". pubsapp.acs.org. Retrieved 2023-07-06.
- ↑ Moore, Anna (2007-05-13). "Eternal sunshine". The Observer. ISSN 0029-7712 . Retrieved 2023-07-06.
- ↑ "Klaus K. Schmiegel Inventions, Patents and Patent Applications - Justia Patents Search". patents.justia.com. Retrieved 2023-07-06.
- ↑ "NIHF Inductee Klaus Schmiegel Invented Prozac Medication". www.invent.org. 2023-07-06. Retrieved 2023-07-06.
- ↑ "United States Patent and Trademark Office 1999 Annual Report" (PDF). Retrieved July 6, 2023.