Related Research Articles

Leprosy, also known as Hansen's disease (HD), is a long-term infection by the bacteria Mycobacterium leprae or Mycobacterium lepromatosis. Infection can lead to damage of the nerves, respiratory tract, skin, and eyes. This nerve damage may result in a lack of ability to feel pain, which can lead to the loss of parts of a person's extremities from repeated injuries or infection through unnoticed wounds. An infected person may also experience muscle weakness and poor eyesight. Leprosy symptoms may begin within one year, but, for some people, symptoms may take 20 years or more to occur.

A leper colony, also known by many other names, is an isolated community for the quarantining and treatment of lepers, people suffering from leprosy. M. leprae, the bacterium responsible for leprosy, is believed to have spread from East Africa through the Middle East, Europe, and Asia by the 5th century before reaching the rest of the world more recently. Historically, leprosy was believed to be extremely contagious and divinely ordained, leading to enormous stigma against its sufferers. Other severe skin diseases were frequently conflated with leprosy and all such sufferers were kept away from the general public, although some religious orders provided medical care and treatment. Recent research has shown M. leprae has maintained a similarly virulent genome over at least the last thousand years, leaving it unclear which precise factors led to leprosy's near elimination in Europe by 1700. A growing number of cases following the first wave of European colonization, however, led to increased attention towards leprosy during the New Imperialism of the late 19th century. Following G.A. Hansen's discovery of the role of M. leprae in the disease, the First International Leprosy Conference held in Berlin in 1897 renewed interest and investment in the isolation of lepers throughout the European colonial empires. Although Western countries now generally treat cases of leprosy individually on an outpatient basis, traditional isolated colonies continue to exist in India, China, and some other countries.

Nummular dermatitis is one of the many forms of dermatitis. It is characterized by round or oval-shaped itchy lesions. The name comes from the Latin word "nummus," which means "coin."
Lepra (Leprosy Relief Association) is a UK-based international charity established in 1924, working to diagnose, treat, and rehabilitate people with leprosy. Lepra currently works in India, Bangladesh, and Zimbabwe.
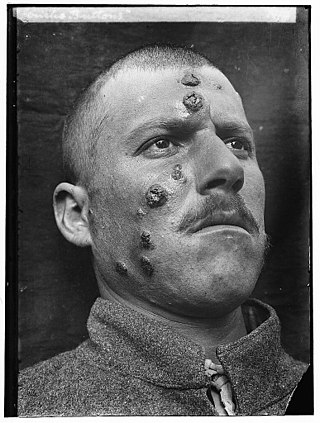
Cutaneous leishmaniasis is the most common form of leishmaniasis affecting humans. It is a skin infection caused by a single-celled parasite that is transmitted by the bite of a phlebotomine sand fly. There are about thirty species of Leishmania that may cause cutaneous leishmaniasis.

Podoconiosis, also known as nonfilarial elephantiasis, is a disease of the lymphatic vessels of the lower extremities that is caused by chronic exposure to irritant soils. It is the second most common cause of tropical lymphedema after lymphatic filariasis, and it is characterized by prominent swelling of the lower extremities, which leads to disfigurement and disability. Methods of prevention include wearing shoes and using floor coverings. Mainstays of treatment include daily foot hygiene, compression bandaging, and when warranted, surgery of overlying nodules.

Serpiginous, first known to be used in the 15th century, is a term from Latin serpere to creep, usually referring to a creeping, snakelike or slowly progressive skin disease.
Pityriasis alba is a skin condition, a type of dermatitis, commonly seen in children and young adults as dry, fine-scaled, pale patches on the face. It is self-limiting and usually only requires use of moisturizer creams.
Leprosy was said to be first recognized in the ancient civilizations of China, Egypt, and India, according to the World Health Organization (WHO). Leprosy, also known as Hansen's disease, was officially eliminated at the national level in China by 1982, meaning prevalence is lower than 1 in 100,000. There are 3,510 active cases today. Though leprosy has been brought under control in general, the situation in some areas is worsening, according to China's Ministry of Health. In the past, leprosy sufferers were ostracized by their communities as the disease was incurable, disfiguring, and wrongly thought to be highly infectious.
Venereology is a branch of medicine that is concerned with the study and treatment of sexually transmitted diseases (STDs). The name derives from Roman goddess Venus, associated with love, beauty and fertility. A physician specializing in venereology is called a venereologist. In many areas of the world, the specialty is usually combined with dermatology.
Granuloma multiforme is a cutaneous condition most commonly seen in central Africa, and rarely elsewhere, characterized by skin lesions that are on the upper trunk and arms in sun-exposed areas. It may be confused with tuberculoid leprosy, with which it has clinical similarities. The condition was first noted by Gosset in the 1940s, but it was not until 1964 that Leiker coined the term to describe "a disease resembling leprosy" in his study in Nigeria.
Leprosy stigma is a type of social stigma, a strong negative feeling towards a person with leprosy relating to their moral status in society. It is also referred to as leprosy-related stigma, leprostigma, and stigma of leprosy. Since ancient times, leprosy instilled the practice of fear and avoidance in many societies because of the associated physical disfigurement and lack of understanding behind its cause. Because of the historical trauma the word "leprosy" invokes, the disease is now referred to as Hansen's disease, named after Gerhard Armauer Hansen who discovered Mycobacterium leprae, the bacterial agent that causes Hansen's disease. Those who have suffered from Hansen's disease describe the impact of social stigma as far worse than the physical manifestations despite it being only mildly contagious and pharmacologically curable. This sentiment is echoed by Weis and Ramakrishna, who noted that "the impact of the meaning of the disease may be a greater source of suffering than symptoms of the disease".

Worldwide, two to three million people are estimated to be permanently disabled because of leprosy. India has the greatest number of cases, with Brazil second and Indonesia third.
Vasant Ramji Khanolkar, better known as V. R. Khanolkar, was an Indian pathologist. He made major contributions to the epidemiology and understanding of cancer, blood groups, and leprosy. He has been called the "Father of Pathology and Medical Research in India."
There has, historically, been fear around leprosy and people with the disease have suffered stigma, isolation and social exclusion. Expulsion of individuals infected with leprosy to quarantined areas or special institutions has been the general protocol since ancient times and was the recommended course of action by the Leprosy Conference of Berlin 1897. As a result, the exclusion and quarantining of people infected with leprosy became law, hence leprosy colonies were formed. The inhabitants of these colonies had very little legal recourse in preventing their exclusion and, even after they were treated and cured, many had trouble reintegrating into society. Even by the 1960s, when leprosy was highly treatable and curable, it still resulted in repulsion, and the exclusion of sufferers, by the general populace. As leprosy became curable, the focus of study shifted towards investigating the social aspects of the disease. This has become relevant due to the fact that the disease is making a resurgence and is proving resistant to previous remedies.
Indira Nath was an Indian immunologist. Her major contribution in medical science deals with mechanisms underlying immune unresponsiveness in man, reactions and nerve damage in leprosy and a search for markers for viability of the Leprosy bacillus. Prof. Nath's fields of specialisations are Immunology, Pathology, Medical biotechnology, and communicable diseases.

The history of leprosy was traced to its origins by an international team of 22 geneticists using comparative genomics of the worldwide distribution of Mycobacterium leprae. Monot et al. (2005) determined that leprosy originated in East Africa or the Near East and traveled with humans along their migration routes, including those of trade in goods and slaves. The four strains of M. leprae are based in specific geographic regions where each predominantly occurs:

Dr AJ Kanwar is an Indian Dermatologist. He has been Senior Professor and Head, Department of Dermatology, Venereology & Leprology, PGI Chandigarh and currently practices in his hometown, New Delhi, India. Dr AJ Kanwar is the son of Late Shri Inder Singh and Smt Shanti Devi and was born on 29 June 1948. He attended school in New Delhi and graduated from the prestigious institute AIIMS, New Delhi in MBBS (Dermatology) in 1969. He continued in AIIMS, New Delhi to obtain his post graduate degree (M.D.) in Dermatology and Venereology in 1975. After his senior residency in AIIMS, Dr Kanwar went on a foreign assignment in Benghazi, Libya. He also served a year in St John's Institute of Dermatology, London during a Commonwealth Medical Fellowship. He received a special training in Pediatric Dermatology during this year. To his credit are also time in National Institute of Health, Washington USA in 2006 for a Fellowship in AIDS, and a month in Kurume, Japan in 2010 for special training in Pemphigus. Dr Kanwar's foreign assignment in Libya, ended in 1987 when he returned to join PGI Chandigarh.

Venkataram Mysore is a dermatologist, dermatopathologist, and hair transplant surgeon from Bangalore, India. He has over 30 years experience as a dermatologist, 18 years as a teacher and is currently the director of the Venkat Center for Advanced Dermatology and Post-Graduate Training.
Neglected tropical diseases in India are a group of bacterial, parasitic, viral, and fungal infections that are common in low income countries but receive little funding to address them. Neglected tropical diseases are common in India.
References
- ↑ WHO (September 2011). "Leprosy update, 2011". Weekly Epidemiological Record. 36: 389–400. Archived from the original on 2014-02-16. Retrieved 2014-02-16.
- 1 2 3 4 Sengupta, Utpal (Spring 2018). "Elimination of Leprosy in India: An Analysis". Indian Journal of Dermatology, Venereology and Leprology. 84 (2): 131–136. doi: 10.4103/ijdvl.IJDVL_1070_16 . PMID 29451189.
- 1 2 World Health Organization (2009): Leprosy. http://www.who.int/mediacentre/factsheets/fs101/en/index.html
- 1 2 Seshadri, Divya; Khaitan, Binod K.; Khanna, Neena; Sagar, Rajesh (1 March 2015). "Dehabilitation in the era of elimination and rehabilitation: a study of 100 leprosy patients from a tertiary care hospital in India". Leprosy Review. 86 (1): 62–74. doi: 10.47276/lr.86.1.62 . PMID 26065148.
- 1 2 3 4 Muthuvel, Thirumugam; Govindarajulu, Srinivas; Isaakidis, Petros; Shewade, Hemant; Rokade, Vasudev; Singh, Rajbir; Kamble, Sanjeev (January 2017). ""I Wasted 3 Years, Thinking It's Not a Problem": Patient and Health System Delays in Diagnosis of Leprosy in India: A Mixed-Methods Study". PLOS Neglected Tropical Diseases. 11 (1): e0005192. doi: 10.1371/journal.pntd.0005192 . PMC 5230757 . PMID 28081131.
- ↑ Bhattacharya S., Sehgal Virendra N. (1999). "Leprosy in India". Clinics in Dermatology. 17 (2): 159–170. doi:10.1016/s0738-081x(99)00009-7. PMID 10330599.
- ↑ Barrett, Ron. "Medical Anthropology: Leprosy on the Ganges." Conformity and Conflict: Readings in Cultural Anthropology, edited by James Spradley and David W. McCurdy, 14th ed., Pearson, 2012, pp. 351-358.
- ↑ Poestges, Heide (June 2011). "Leprosy, the key to another kingdom". Leprosy Review. 82 (2): 155–167. doi: 10.47276/lr.82.2.155 . PMID 21888140. Gale A317779757.
- ↑ Kathju, Junaid (6 October 2021). "Abandoned by Families, Adopted by Strangers: Lives of Leprosy Patients in Kashmir". The Wire.
- ↑ "Indian lepers whose dreams are shattered by stigma". 30 January 2017.
- ↑ Robbins G.; et al. (2009). "Ancient Skeletal Evidence for Leprosy in India (2000 B.C.)". PLOS ONE. 4 (5): e5669. Bibcode:2009PLoSO...4.5669R. doi: 10.1371/journal.pone.0005669 . PMC 2682583 . PMID 19479078.
- ↑ Jacob J., Franco-Paredes Carlos (2008). "The Stigmatization and Control". PLOS Neglected Tropical Diseases. 2 (1): 1–3.
- ↑ "Text of the Act from the Indian Lawyer".
- ↑ Report of the Global Forum on Elimination of Leprosy as a Public Health Problem. World Health Organization. 26 May 2006.[ dead link ]
- ↑ Lipy K, Shukla; et al. (2015). "Evaluation of the Effect of Block Level Awareness Campaign on Performance Indicators of National Leprosy Elimination Program in Vadodara District, Gujarat, India". Indian Journal of Dermatology, Venereology and Leprology. 81 (3): 257–262. doi: 10.4103/0378-6323.154793 . PMID 25851761.
- 1 2 Putul, A. (2008): Laws in India Criminalise Leprosy.OneWorld South Asia. http://southasia.oneworld.net/Article/laws-in-india-criminalise-leprosy
- ↑ "Supreme Court notice on petition to repeal 144 laws against leprosy patients". Economic Times. 5 December 2017. Gale A517345944.
- ↑ "Discrimination against leprosy patients: SC seeks govt response on plea". Times of India. 5 December 2017. Gale A517346348.
- ↑ "Leprosy's 'return' rattles docs after 'elimination'". The Times of India. ISSN 0971-8257 . Retrieved 2023-07-28.