Related Research Articles

Bacterial vaginosis (BV) is an infection of the vagina caused by excessive growth of bacteria. Common symptoms include increased vaginal discharge that often smells like fish. The discharge is usually white or gray in color. Burning with urination may occur. Itching is uncommon. Occasionally, there may be no symptoms. Having BV approximately doubles the risk of infection by a number of sexually transmitted infections, including HIV/AIDS. It also increases the risk of early delivery among pregnant women.

Caesarean section, also known as C-section, cesarean, or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the mother or child at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In the developed countries, most deliveries occur in hospitals, while in the developing countries most are home births.

Maternal death or maternal mortality is defined in slightly different ways by several different health organizations. The World Health Organization (WHO) defines maternal death as the death of a pregnant mother due to complications related to pregnancy, underlying conditions worsened by the pregnancy or management of these conditions. This can occur either while she is pregnant or within six weeks of resolution of the pregnancy. The CDC definition of pregnancy-related deaths extends the period of consideration to include one year from the resolution of the pregnancy. Pregnancy associated death, as defined by the American College of Obstetricians and Gynecologists (ACOG), are all deaths occurring within one year of a pregnancy resolution. Identification of pregnancy associated deaths is important for deciding whether or not the pregnancy was a direct or indirect contributing cause of the death.
Labor induction is the process or treatment that stimulates childbirth and delivery. Inducing (starting) labor can be accomplished with pharmaceutical or non-pharmaceutical methods. In Western countries, it is estimated that one-quarter of pregnant women have their labor medically induced with drug treatment. Inductions are most often performed either with prostaglandin drug treatment alone, or with a combination of prostaglandin and intravenous oxytocin treatment.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.
Maternal health is the health of women during pregnancy, childbirth, and the postpartum period. In most cases, maternal health encompasses the health care dimensions of family planning, preconception, prenatal, and postnatal care in order to ensure a positive and fulfilling experience. In other cases, maternal health can reduce maternal morbidity and mortality. Maternal health revolves around the health and wellness of pregnant women, particularly when they are pregnant, at the time they give birth, and during child-raising. WHO has indicated that even though motherhood has been considered as a fulfilling natural experience that is emotional to the mother, a high percentage of women develop health problems and sometimes even die. Because of this, there is a need to invest in the health of women. The investment can be achieved in different ways, among the main ones being subsidizing the healthcare cost, education on maternal health, encouraging effective family planning, and ensuring progressive check up on the health of women with children. Maternal morbidity and mortality particularly affects women of color and women living in low and lower-middle income countries.
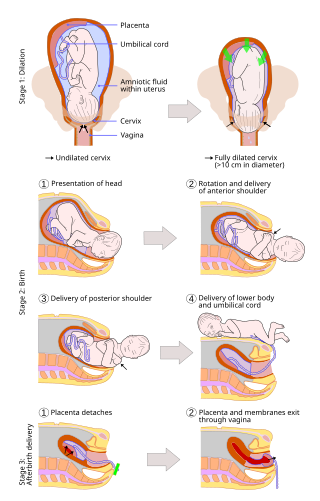
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, as it is correlated with lower morbidity and mortality than caesarean sections (C-sections), though it is not clear whether this is causal.

A high-risk pregnancy is a pregnancy where the mother or the fetus has an increased risk of adverse outcomes compared to uncomplicated pregnancies. No concrete guidelines currently exist for distinguishing “high-risk” pregnancies from “low-risk” pregnancies; however, there are certain studied conditions that have been shown to put the mother or fetus at a higher risk of poor outcomes. These conditions can be classified into three main categories: health problems in the mother that occur before she becomes pregnant, health problems in the mother that occur during pregnancy, and certain health conditions with the fetus.
Antenatal depression, also known as prenatal or perinatal depression, is a form of clinical depression that can affect a woman during pregnancy, and can be a precursor to postpartum depression if not properly treated. It is estimated that 7% to 20% of pregnant women are affected by this condition. Any form of prenatal stress felt by the mother can have negative effects on various aspects of fetal development, which can cause harm to the mother and child. Even after birth, a child born from a depressed or stressed mother feels the affects. The child is less active and can also experience emotional distress. Antenatal depression can be caused by the stress and worry that pregnancy can bring, but at a more severe level. Other triggers include unplanned pregnancy, difficulty becoming pregnant, history of abuse, and economic or family situations.
A pre-existing disease in pregnancy is a disease that is not directly caused by the pregnancy, in contrast to various complications of pregnancy, but which may become worse or be a potential risk to the pregnancy. A major component of this risk can result from necessary use of drugs in pregnancy to manage the disease.
The National Perinatal Epidemiology Unit (NPEU) is a multi-disciplinary research unit within the Nuffield Department of Population Health at Oxford University. It is located in the Richard Doll Building on the Old Road Campus, in Headington, east Oxford, England.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
The vaginal flora in pregnancy, or vaginal microbiota in pregnancy, is different from the vaginal flora before sexual maturity, during reproductive years, and after menopause. A description of the vaginal flora of pregnant women who are immunocompromised is not covered in this article. The composition of the vaginal flora significantly differs in pregnancy. Bacteria or viruses that are infectious most often have no symptoms.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.

Emergency childbirth is the precipitous birth of an infant in an unexpected setting. In planned childbirth, mothers choose the location and obstetric team ahead of time. Options range from delivering at home, at a hospital, a medical facility or a birthing center. Sometimes, birth can occur on the way to these facilities, without a healthcare team. The rates of unplanned childbirth are low. If the birth is imminent, emergency measures may be needed. Emergency services can be contacted for help in some countries.

COVID-19 infection in pregnancy is associated with several pregnancy complications. However, pregnancy does not appear to increase the susceptibility of becoming infected by COVID-19. Recommendations for the prevention of COVID-19 include the same measures as non-pregnant people.
Jennifer J. Kurinczuk is a British physician who is a Professor of Perinatal Epidemiology and Director of the National Perinatal Epidemiology Unit at the University of Oxford. In 2019 she was named an Honorary Fellow of the Royal College of Obstetricians and Gynaecologists. During the COVID-19 pandemic, Kurinczuk investigated the neonatal complications of coronavirus disease.

Lucy Chappell is a British professor of obstetrics at King’s College London and the Chief Scientific Adviser (CSA) for the UK Department of Health and Social Care. As part of her CSA role, she oversees the National Institute for Health and Care Research (NIHR) as Chief Executive Officer. Her research areas include medical problems during pregnancy such as pre-eclampsia, and the safety of medicines in pregnancy.
References
- 1 2 3 "Directory | NIHR". www.nihr.ac.uk. Retrieved 2020-07-06.
- ↑ Knight, Marian (1997). Syncytiotrophoblast microvillous membrane deportation in the pathogenesis of pre-eclampsia (Thesis). OCLC 43180655.
- ↑ "Marian Knight". BMFMS Conference. Retrieved 2020-07-06.
- ↑ "UK Obstetric Surveillance System (UKOSS) | NPEU". www.npeu.ox.ac.uk. Retrieved 2020-07-06.
- ↑ "People | NPEU". www.npeu.ox.ac.uk. Retrieved 2020-07-06.
- ↑ "Professor Marian Knight | Baby Lifeline" . Retrieved 2020-07-06.
- 1 2 "Half of perinatal suicides by women 'could be prevented by better care'". the Guardian. 2015-12-08. Retrieved 2020-07-06.
- ↑ Agency (2015-12-08). "Basic checks on expectant mothers' mental health can prevent deaths, experts say". The Daily Telegraph. ISSN 0307-1235 . Retrieved 2020-07-06.
- 1 2 Knight, Marian; Chiocchia, Virginia; Partlett, Christopher; Rivero-Arias, Oliver; Hua, Xinyang; Hinshaw, Kim; Tuffnell, Derek; Linsell, Louise; Juszczak, Edmund; Knight, Marian; Enderby, Helen (2019-06-15). "Prophylactic antibiotics in the prevention of infection after operative vaginal delivery (ANODE): a multicentre randomised controlled trial". The Lancet. 393 (10189): 2395–2403. doi: 10.1016/S0140-6736(19)30773-1 . ISSN 0140-6736. PMC 6584562 . PMID 31097213. S2CID 153310605.
- ↑ Bonet, Mercedes; Brizuela, Vanessa; Abalos, Edgardo; Cuesta, Cristina; Baguiya, Adama; Chamillard, Mónica; Fawole, Bukola; Knight, Marian; Kouanda, Seni; Lumbiganon, Pisake; Nabhan, Ashraf (2020-05-01). "Frequency and management of maternal infection in health facilities in 52 countries (GLOSS): a 1-week inception cohort study". The Lancet Global Health. 8 (5): e661–e671. doi: 10.1016/S2214-109X(20)30109-1 . ISSN 2214-109X. PMC 7196885 . PMID 32353314.
- ↑ "Pregnant women are not at greater risk of severe COVID-19 than other women". www.nihr.ac.uk. Retrieved 2020-07-06.
- 1 2 Knight, Marian; Bunch, Kathryn; Vousden, Nicola; Morris, Edward; Simpson, Nigel; Gale, Chris; O’Brien, Patrick; Quigley, Maria; Brocklehurst, Peter; Kurinczuk, Jennifer J. (2020-06-08). "Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study". BMJ. 369: m2107. doi: 10.1136/bmj.m2107 . ISSN 1756-1833. PMC 7277610 . PMID 32513659. S2CID 219540353.
- ↑ Roxby, Philippa (2020-06-08). "Higher coronavirus risk for pregnant BAME women". BBC News. Retrieved 2020-07-06.
- ↑ Miller, Anna Medaris. "Pregnant women may be more likely to suffer severe coronavirus infections, according to the largest study of its kind". Business Insider. Retrieved 2020-07-06.
- ↑ "No. 63918". The London Gazette (Supplement). 31 December 2022. p. N20.