Major depressive disorder (MDD), also known as clinical depression, is a mental disorder characterized by at least two weeks of pervasive low mood, low self-esteem, and loss of interest or pleasure in normally enjoyable activities. Introduced by a group of US clinicians in the mid-1970s, the term was adopted by the American Psychiatric Association for this symptom cluster under mood disorders in the 1980 version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), and has become widely used since.
A mental disorder, also referred to as a mental illness, a mental health condition, or a psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. A mental disorder is also characterized by a clinically significant disturbance in an individual's cognition, emotional regulation, or behavior, often in a social context. Such disturbances may occur as single episodes, may be persistent, or may be relapsing–remitting. There are many different types of mental disorders, with signs and symptoms that vary widely between specific disorders. A mental disorder is one aspect of mental health.
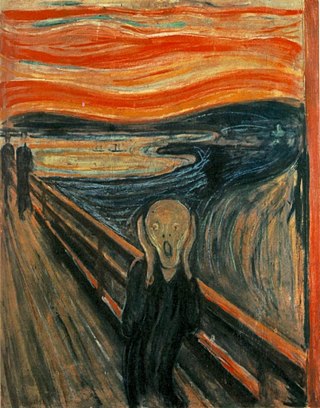
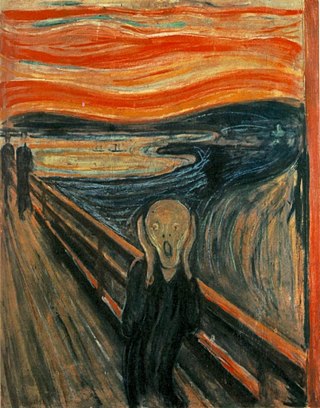
Anxiety disorders are a cluster of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal functions are significantly impaired. Anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, easy fatigue, difficulty concentrating, increased heart rate, chest pain, abdominal pain, and a variety of other symptoms that may vary based on the individual.
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that develops from experiencing a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life or well-being. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress, but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.

Hypochondriasis or hypochondria also known as syndrome is a condition in which a person is excessively and unduly worried about having a serious illness. Hypochondria is an old concept whose meaning has repeatedly changed over its lifespan. It has been claimed that this debilitating condition results from an inaccurate perception of the condition of body or mind despite the absence of an actual medical diagnosis. An individual with hypochondriasis is known as a hypochondriac. Hypochondriacs become unduly alarmed about any physical or psychological symptoms they detect, no matter how minor the symptom may be, and are convinced that they have, or are about to be diagnosed with, a serious illness.

Postpartum depression (PPD), also called postnatal depression, is a type of mood disorder experienced after childbirth, which can affect both sexes. Symptoms may include extreme sadness, low energy, anxiety, crying episodes, irritability, and changes in sleeping or eating patterns. PPD can also negatively affect the newborn child.
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis requires symptoms of both schizophrenia and a mood disorder: either bipolar disorder or depression. The main criterion is the presence of psychotic symptoms for at least two weeks without any mood symptoms. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar I disorder, schizophreniform disorder, or schizophrenia. This is a problem as treatment and prognosis differ greatly for most of these diagnoses.
Self-medication, sometime called do-it-yourself (DIY) medicine, is a human behavior in which an individual uses a substance or any exogenous influence to self-administer treatment for physical or psychological conditions, for example headaches or fatigue.
Generalized anxiety disorder (GAD) is a mental and behavioral disorder, specifically an anxiety disorder characterized by excessive, uncontrollable and often irrational worry about events or activities. Worry often interferes with daily functioning, and individuals with GAD are often overly concerned about everyday matters such as health, finances, death, family, relationship concerns, or work difficulties. Symptoms may include excessive worry, restlessness, trouble sleeping, exhaustion, irritability, sweating, and trembling.

Depression is a mental state of low mood and aversion to activity. It affects more than 280 million people of all ages. Depression affects a person's thoughts, behavior, feelings, and sense of well-being. Depressed people often experience loss of motivation or interest in, or reduced pleasure or joy from, experiences that would normally bring them pleasure or joy.
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usual, causing marked distress, preoccupation with the stressor and its consequences, and functional impairment.
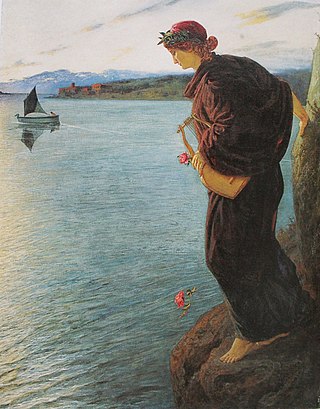
Suicidal ideation, or suicidal thoughts, is the thought process of having ideas, or ruminations about the possibility of completing suicide. It is not a diagnosis but is a symptom of some mental disorders, use of certain psychoactive drugs, and can also occur in response to adverse life events without the presence of a mental disorder.
Mental disorders are classified as a psychological condition marked primarily by sufficient disorganization of personality, mind, and emotions to seriously impair the normal psychological and often social functioning of the individual. Individuals diagnosed with certain mental disorders can be unable to function normally in society. Mental disorders may consist of several affective, behavioral, cognitive and perceptual components. The acknowledgement and understanding of mental health conditions has changed over time and across cultures. There are still variations in the definition, classification, and treatment of mental disorders.

Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions. These include various matters related to mood, behaviour, cognition, perceptions, and emotions.

Social anxiety disorder (SAD), also known as social phobia, is an anxiety disorder characterized by sentiments of fear and anxiety in social situations, causing considerable distress and impairing ability to function in at least some aspects of daily life. These fears can be triggered by perceived or actual scrutiny from others. Individuals with social anxiety disorder fear negative evaluations from other people.
Somatic symptom disorder, also known as somatoform disorder, is defined by one or more chronic physical symptoms that coincide with excessive and maladaptive thoughts, emotions, and behaviors connected to those symptoms. The symptoms are not deliberately produced or feigned, and they may or may not coexist with a known medical ailment.
Antenatal depression, also known as prenatal or perinatal depression, is a form of clinical depression that can affect a woman during pregnancy, and can be a precursor to postpartum depression if not properly treated. It is estimated that 7% to 20% of pregnant women are affected by this condition. Any form of prenatal stress felt by the mother can have negative effects on various aspects of fetal development, which can cause harm to the mother and child. Even after birth, a child born from a depressed or stressed mother feels the affects. The child is less active and can also experience emotional distress. Antenatal depression can be caused by the stress and worry that pregnancy can bring, but at a more severe level. Other triggers include unplanned pregnancy, difficulty becoming pregnant, history of abuse, and economic or family situations.
The relationships between digital media use and mental health have been investigated by various researchers—predominantly psychologists, sociologists, anthropologists, and medical experts—especially since the mid-1990s, after the growth of the World Wide Web. A significant body of research has explored "overuse" phenomena, commonly known as "digital addictions", or "digital dependencies." These phenomena manifest differently in many societies and cultures. Some experts have investigated the benefits of moderate digital media use in various domains, including in mental health, and the treatment of mental health problems with novel technological solutions.

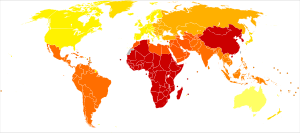
The COVID-19 pandemic has impacted the mental health of people across the globe. The pandemic has caused widespread anxiety, depression, and post-traumatic stress disorder symptoms. According to the UN health agency WHO, in the first year of the COVID-19 pandemic, prevalence of common mental health conditions, such as depression and anxiety, went up by more than 25 percent. The pandemic has damaged social relationships, trust in institutions and in other people, has caused changes in work and income, and has imposed a substantial burden of anxiety and worry on the population. Women and young people face the greatest risk of depression and anxiety.

There is increasing evidence suggesting that COVID-19 causes both acute and chronic neurologicalor psychological symptoms. Caregivers of COVID-19 patients also show a higher than average prevalence of mental health concerns. These symptoms result from multiple different factors.