Related Research Articles

An emergency department (ED), also known as an accident & emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance. The emergency department is usually found in a hospital or other primary care center.
In medicine, comorbidity is the presence of one or more additional conditions often co-occurring with a primary condition. Comorbidity describes the effect of all other conditions an individual patient might have other than the primary condition of interest, and can be physiological or psychological. In the context of mental health, comorbidity often refers to disorders that are often coexistent with each other, such as depression and anxiety disorders.
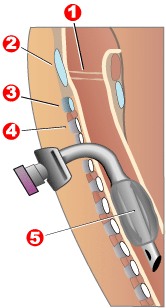
Tracheotomy, or tracheostomy, is a surgical procedure which consists of making an incision (cut) on the anterior aspect (front) of the neck and opening a direct airway through an incision in the trachea (windpipe). The resulting stoma (hole) can serve independently as an airway or as a site for a tracheal tube or tracheostomy tube to be inserted; this tube allows a person to breathe without the use of the nose or mouth.

Maternal death or maternal mortality is defined by the World Health Organization (WHO) as "the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes." These maternal deaths are divided into two categories: direct obstetric deaths and indirect obstetric deaths. The latter are deaths for which there was a preexisting disease that was aggravated by the pregnancy.
A medical error is a preventable adverse effect of care ("iatrogenesis"), whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, syndrome, behavior, infection, or other ailment. Globally, it is estimated that 142,000 people died in 2013 from adverse effects of medical treatment; this is an increase from 94,000 in 1990. However, a 2016 study of the number of deaths that were a result of medical error in the U.S. placed the yearly death rate in the U.S. alone at 251,454 deaths, which suggests that the 2013 global estimation may not be accurate. In line with the high importance of the research area, a 2019 study identified 12,415 scientific publications related to medical errors, and outlined as frequently researched and impactful themes errors related to drugs/medications, applications related to medicinal information technology, errors related to critical/intensive care units, to children, and mental conditions associated with medical errors.
Perioperative mortality has been defined as any death, regardless of cause, occurring within 30 days after surgery in or out of the hospital. Globally, 4.2 million people are estimated to die within 30 days of surgery each year. An important consideration in the decision to perform any surgical procedure is to weigh the benefits against the risks. Anesthesiologists and surgeons employ various methods in assessing whether a patient is in optimal condition from a medical standpoint prior to undertaking surgery, and various statistical tools are available. ASA score is the most well known of these.
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. If it results from an unsuitable or incorrect dosage or procedure, this is called a medical error and not a complication. Adverse effects are sometimes referred to as "iatrogenic" because they are generated by a physician/treatment. Some adverse effects occur only when starting, increasing or discontinuing a treatment. Adverse effects can also be caused by placebo treatments . Using a drug or other medical intervention which is contraindicated may increase the risk of adverse effects. Adverse effects may cause complications of a disease or procedure and negatively affect its prognosis. They may also lead to non-compliance with a treatment regimen. Adverse effects of medical treatment resulted in 142,000 deaths in 2013 up from 94,000 deaths in 1990 globally.
Clinical audit is a process that has been defined as a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change
Patient safety is a discipline that emphasizes safety in health care through the prevention, reduction, reporting, and analysis of error and other types of unnecessary harm that often lead to adverse patient events. The frequency and magnitude of avoidable adverse events, often known as patient safety incidents, experienced by patients was not well known until the 1990s, when multiple countries reported significant numbers of patients harmed and killed by medical errors. Recognizing that healthcare errors impact 1 in every 10 patients around the world, the World Health Organization calls patient safety an endemic concern. Indeed, patient safety has emerged as a distinct healthcare discipline supported by an immature yet developing scientific framework. There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety.
A patient safety organization (PSO) is a group, institution, or association that improves medical care by reducing medical errors. Common functions of patient safety organizations are data collection and analysis, reporting, education, funding, and advocacy.

An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine.

Maternal–fetal medicine (MFM), also known as perinatology, is a branch of medicine that focuses on managing health concerns of the mother and fetus prior to, during, and shortly after pregnancy.

Ernest Amory Codman, M.D., was a pioneering Boston surgeon who made contributions to anaesthesiology, radiology, duodenal ulcer surgery, orthopaedic oncology, shoulder surgery, and the study of medical outcomes.
Surgical Outcomes Analysis & Research, SOAR, is a research laboratory of the Department of Surgery at Boston University School of Medicine and Boston Medical Center with expertise in outcomes research. SOAR investigates surgical diseases and perioperative outcomes. The group focuses on pancreatic cancer, other gastrointestinal and hepatobiliary malignancies, vascular disease, and transplant surgery. SOAR's goal is to examine quality, delivery, and financing of care in order to have an immediate impact on patient care and system improvements. The group members utilize national health services and administrative databases, as well as institutional databases, to investigate and to address factors contributing to disease outcomes and healthcare disparities.
Outcomes research is a branch of public health research, which studies the end results of the structure and processes of the health care system on the health and well-being of patients and populations. According to one medical outcomes and guidelines source book - 1996, Outcomes research includes health services research that focuses on identifying variations in medical procedures and associated health outcomes. Though listed as a synonym for the National Library of Medicine MeSH term "Outcome Assessment ", outcomes research may refer to both health services research and healthcare outcomes assessment, which aims at Health technology assessment, decision making, and policy analysis through systematic evaluation of quality of care, access, and effectiveness.

Iatrogenesis is the causation of a disease, a harmful complication, or other ill effect by any medical activity, including diagnosis, intervention, error, or negligence. First used in this sense in 1924, the term was introduced to sociology in 1976 by Ivan Illich, alleging that industrialized societies impair quality of life by overmedicalizing life. Iatrogenesis may thus include mental suffering via medical beliefs or a practitioner's statements. Some iatrogenic events are obvious, like amputation of the wrong limb, whereas others, like drug interactions, can evade recognition. In a 2013 estimate, about 20 million negative effects from treatment had occurred globally. In 2013, an estimated 142,000 persons died from adverse effects of medical treatment, up from an estimated 94,000 in 1990.
The July effect, sometimes referred to as the July phenomenon, is a perceived increase in the risk of medical errors and surgical complications that occurs in association with the time of year in which United States medical school graduates begin residencies. A similar period in the United Kingdom is known as the killing season or, more specifically, Black Wednesday, referring to the first Wednesday in August when postgraduate trainees commence their rotations.
Health care quality is a level of value provided by any health care resource, as determined by some measurement. As with quality in other fields, it is an assessment of whether something is good enough and whether it is suitable for its purpose. The goal of health care is to provide medical resources of high quality to all who need them; that is, to ensure good quality of life, cure illnesses when possible, to extend life expectancy, and so on. Researchers use a variety of quality measures to attempt to determine health care quality, including counts of a therapy's reduction or lessening of diseases identified by medical diagnosis, a decrease in the number of risk factors which people have following preventive care, or a survey of health indicators in a population who are accessing certain kinds of care.
The Trauma Quality Improvement Program (TQIP) was initiated in 2008 by the American College of Surgeons Committee on Trauma. Its aim is to provide risk-adjusted data for the purpose of reducing variability in adult trauma outcomes and offering best practice guidelines to improve trauma care. TQIP makes use of national data to allows hospitals to objectively evaluate their trauma centers' performance relative to other hospitals. TQIP's administrative costs are less than those of other programs, making it an accessible tool for assessing performance and enhancing quality of trauma care.
References
- ↑ Holland, J. (2007). "A role for morbidity and mortality conferences in psychiatry". Australasian Psychiatry. 15 (4): 338–342. doi:10.1080/10398560701351803. PMID 17612890. S2CID 72647543.
- 1 2 Campbell, W. (1988). "Surgical morbidity and mortality meetings". Annals of the Royal College of Surgeons of England. 70 (6): 363–365. PMC 2498614 . PMID 3207327.
- ↑ Gawande, Atul (2002). Complications: A Surgeon's Notes on an Imperfect Science. Macmillan. pp. 47–74. ISBN 0-8050-6319-6.
- ↑ Orlander, J.; Barber, T.; Fincke, B. (2002). "The morbidity and mortality conference: the delicate nature of learning from error". Academic Medicine. 77 (10): 1001–1006. doi: 10.1097/00001888-200210000-00011 . PMID 12377674.
- ↑ Orlander, Jay D, and B Graeme Fincke. “Morbidity and Mortality Conference: A Survey of Academic Internal Medicine Departments.” Journal of General Internal Medicine 18.8 (2003): 656–658. PMC. Web. 19 Feb. 2017.
- ↑ Cicero, MD, Mark X.; Whitfill, MPH, Travis; Munjal, MD, Kevin; Madhok, MD, MPH, Manu; Diaz, MD, Maria Carmen G.; Scherzer, MD, Daniel J.; Walsh, MD, Barbara M.; Bowen, RN, BSN, CPEN, NREMT-P, Angela; Redlener, MD, Michael; Goldberg, MD, MPH, Scott A.; Symons, MD, Nadine (2017-04-01). "60 seconds to survival: A pilot study of a disaster triage video game for prehospital providers". American Journal of Disaster Medicine. 12 (2): 75–83. doi:10.5055/ajdm.2017.0263. ISSN 1932-149X. PMID 29136270.CS1 maint: multiple names: authors list (link)