Rhinoplasty, commonly called nose job, medically called nasal reconstruction is a plastic surgery procedure for altering and reconstructing the nose. There are two types of plastic surgery used – reconstructive surgery that restores the form and functions of the nose and cosmetic surgery that changes the appearance of the nose. Reconstructive surgery seeks to resolve nasal injuries caused by various traumas including blunt, and penetrating trauma and trauma caused by blast injury. Reconstructive surgery can also treat birth defects, breathing problems, and failed primary rhinoplasties. Rhinoplasty may remove a bump, narrow nostril width, change the angle between the nose and the mouth, or address injuries, birth defects, or other problems that affect breathing, such as a deviated nasal septum or a sinus condition. Surgery only on the septum is called a septoplasty.
Facial feminization surgery (FFS) is a set of reconstructive surgical procedures that alter typically male facial features to bring them closer in shape and size to typical female facial features. FFS can include various bony and soft tissue procedures such as brow lift, rhinoplasty, cheek implantation, and lip augmentation.
Grafting refers to a surgical procedure to move tissue from one site to another on the body, or from another creature, without bringing its own blood supply with it. Instead, a new blood supply grows in after it is placed. A similar technique where tissue is transferred with the blood supply intact is called a flap. In some instances, a graft can be an artificially manufactured device. Examples of this are a tube to carry blood flow across a defect or from an artery to a vein for use in hemodialysis.

A facelift, technically known as a rhytidectomy, is a type of cosmetic surgery procedure used to give a more youthful facial appearance. There are multiple surgical techniques and exercise routines. Surgery usually involves the removal of excess facial skin, with or without the tightening of underlying tissues, and the redraping of the skin on the patient's face and neck. Exercise routines tone underlying facial muscles without surgery. Surgical facelifts are effectively combined with eyelid surgery (blepharoplasty) and other facial procedures and are typically performed under general anesthesia or deep twilight sleep.

Hypertelorism is an abnormally increased distance between two organs or bodily parts, usually referring to an increased distance between the orbits (eyes), or orbital hypertelorism. In this condition the distance between the inner eye corners as well as the distance between the pupils is greater than normal. Hypertelorism should not be confused with telecanthus, in which the distance between the inner eye corners is increased but the distances between the outer eye corners and the pupils remain unchanged.
The terms free flap, free autologous tissue transfer and microvascular free tissue transfer are synonymous terms used to describe the "transplantation" of tissue from one site of the body to another, in order to reconstruct an existing defect. "Free" implies that the tissue is completely detached from its blood supply at the original location and then transferred to another location and the circulation in the tissue re-established by anastomosis of artery(s) and vein(s). This is in contrast to a "pedicled" flap in which the tissue is left partly attached to the donor site ("pedicle") and simply transposed to a new location; keeping the "pedicle" intact as a conduit to supply the tissue with blood.
Velopharyngeal insufficiency is a disorder of structure that causes a failure of the velum to close against the posterior pharyngeal wall during speech in order to close off the nose during oral speech production. This is important because speech requires sound and airflow to be directed into the oral cavity (mouth) for the production of all speech sound with the exception of nasal sounds. If complete closure does not occur during speech, this can cause hypernasality and/or audible nasal emission during speech. In addition, there may be inadequate airflow to produce most consonants, making them sound weak or omitted.
A forehead lift, also known as a browlift or browplasty, is a cosmetic surgery procedure used to elevate a drooping eyebrow that may obstruct vision and/or to remove the deep “worry” lines that run across the forehead.
A DIEP flap is type of breast reconstruction where blood vessels, fat, and skin from the lower belly are relocated to the chest to rebuild breasts after mastectomy. DIEP stands for the deep inferior epigastric perforator artery, which runs through the abdomen. This is a type of autologous reconstruction, meaning one's own tissue is used.
David Ralph Millard, Jr. was a plastic surgeon who developed several techniques used in cleft lip and palate surgeries. He also popularized the double eyelid surgery or "Asian blepharoplasty" to “deorientalize” patients’ faces while stationed in South Korea during the Korean War. He was chief of the Division of Plastic Surgery at University of Miami's Miller School of Medicine for 28 years, and maintained a private practice in Miami.

Frontonasal dysplasia (FND) is a congenital malformation of the midface. For the diagnosis of FND, a patient should present at least two of the following characteristics: hypertelorism, a wide nasal root, vertical midline cleft of the nose and/or upper lip, cleft of the wings of the nose, malformed nasal tip, encephalocele or V-shaped hair pattern on the forehead. The cause of FND remains unknown. FND seems to be sporadic (random) and multiple environmental factors are suggested as possible causes for the syndrome. However, in some families multiple cases of FND were reported, which suggests a genetic cause of FND.
A facial cleft is an opening or gap in the face, or a malformation of a part of the face. Facial clefts is a collective term for all sorts of clefts. All structures like bone, soft tissue, skin etc. can be affected. Facial clefts are extremely rare congenital anomalies. There are many variations of a type of clefting and classifications are needed to describe and classify all types of clefting. Facial clefts hardly ever occur isolated; most of the time there is an overlap of adjacent facial clefts.
Flap surgery is a technique in plastic and reconstructive surgery where any type of tissue is lifted from a donor site and moved to a recipient site with an intact blood supply. This is distinct from a graft, which does not have an intact blood supply and therefore relies on growth of new blood vessels. This is done to fill a defect such as a wound resulting from injury or surgery when the remaining tissue is unable to support a graft, or to rebuild more complex anatomic structures such as breast or jaw.
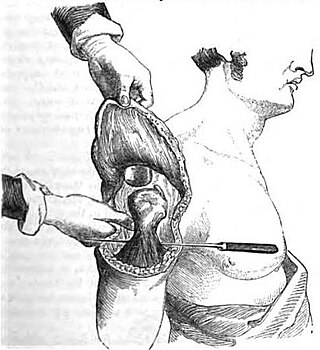
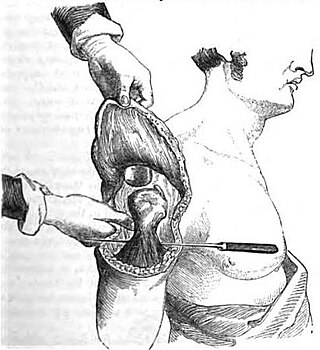
Scalp reconstruction is a surgical procedure for people with scalp defects. Scalp defects may be partial or full thickness and can be congenital or acquired. Because not all layers of the scalp are elastic and the scalp has a convex shape, the use of primary closure is limited. Sometimes the easiest way of closing the wound may not be the ideal or best way. The choice for a reconstruction depends on multiple factors, such as the defect itself, the patient characteristics and surgeon preference.
Andrew A. Jacono, M.D., FACS is an American facial surgeon and creator of the minimal access deep-plane extended facelift, a minimally invasive hybrid facelift. Jacono starred in the Discovery Fit & Health television program Facing Trauma as the volunteer surgeon who reconstructed faces disfigured in abusive relationships and other violent circumstances.
The cheek constitutes the facial periphery, plays a key role in the maintenance of oral competence and mastication, is involved in the facial manifestation of human emotion, and supports neighboring primary structures.
Non-surgical rhinoplasty is a medical aesthetic procedure in which injectable fillers, most commonly hyaluronic acid ones like Restylane and Juvederm or calcium hydroxyapatite (Radiesse), are used to alter and shape a person's nose without a surgery. The procedure fills in depressed areas on the nose, lifting the angle of the tip or smoothing the appearance of bumps on the bridge. Non surgical rhinoplasty is an augmentation procedure, so it cannot reduce the size of someone's nose. The cosmetic procedure carries the risk of causing serious skin damage or distant complications like blindness. If the filler product is injected into an artery, filler can travel in the arteries and blocks smaller size arteries like ophthalmic artery and cause blindness. If blood vessels of the skin is blocked, skin necrosis can develop. Hyaluronic acid based fillers can be reversed even if injected into a blood vessel with an enzyme called hyaluronidase, which can be also injected like fillers.
Perforator flap surgery is a technique used in reconstructive surgery where skin and/or subcutaneous fat are removed from a distant or adjacent part of the body to reconstruct the excised part. The vessels that supply blood to the flap are isolated perforator(s) derived from a deep vascular system through the underlying muscle or intermuscular septa. Some perforators can have a mixed septal and intramuscular course before reaching the skin. The name of the particular flap is retrieved from its perforator and not from the underlying muscle. If there is a potential to harvest multiple perforator flaps from one vessel, the name of each flap is based on its anatomical region or muscle. For example, a perforator that only traverses through the septum to supply the underlying skin is called a septal perforator. Whereas a flap that is vascularised by a perforator traversing only through muscle to supply the underlying skin is called a muscle perforator. According to the distinct origin of their vascular supply, perforators can be classified into direct and indirect perforators. Direct perforators only pierce the deep fascia, they don't traverse any other structural tissue. Indirect perforators first run through other structures before piercing the deep fascia.
Free-flap breast reconstruction is a type of autologous-tissue breast reconstruction applied after mastectomy for breast cancer, without the emplacement of a breast implant prosthesis. As a type of plastic surgery, the free-flap procedure for breast reconstruction employs tissues, harvested from another part of the woman's body, to create a vascularised flap, which is equipped with its own blood vessels. Breast-reconstruction mammoplasty can sometimes be realised with the application of a pedicled flap of tissue that has been harvested from the latissimus dorsi muscle, which is the broadest muscle of the back, to which the pedicle (“foot”) of the tissue flap remains attached until it successfully grafts to the recipient site, the mastectomy wound. Moreover, if the volume of breast-tissue excised was of relatively small mass, breast augmentation procedures, such as autologous-fat grafting, also can be applied to reconstruct the breast lost to mastectomy.

David A. Hidalgo is an American reconstructive and aesthetic plastic surgeon, author, and visual artist. He holds the academic title of Clinical Professor of Surgery at Weill Cornell Medical College in New York City.