Organ donation is the process when a person authorizes an organ of their own to be removed and transplanted to another person, legally, either by consent while the donor is alive, through a legal authorization for deceased donation made prior to death, or for deceased donations through the authorization by the legal next of kin.

Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location. Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.
The Uniform Anatomical Gift Act (UAGA), and its periodic revisions, is one of the Uniform Acts drafted by the National Conference of Commissioners on Uniform State Laws (NCCUSL), also known as the Uniform Law Commission (ULC), in the United States with the intention of harmonizing state laws between the states.
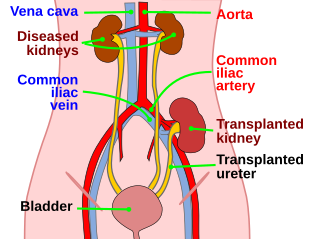
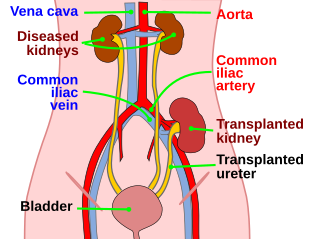
Kidney transplant or renal transplant is the organ transplant of a kidney into a patient with end-stage kidney disease (ESRD). Kidney transplant is typically classified as deceased-donor or living-donor transplantation depending on the source of the donor organ. Living-donor kidney transplants are further characterized as genetically related (living-related) or non-related (living-unrelated) transplants, depending on whether a biological relationship exists between the donor and recipient. The first successful kidney transplant was performed in 1954 by a team including Joseph Murray, the recipient’s surgeon, and Hartwell Harrison, surgeon for the donor. Murray was awarded a Nobel Prize in Physiology or Medicine in 1990 for this and other work. In 2018, an estimated 95,479 kidney transplants were performed worldwide, 36% of which came from living donors.

The Health Resources and Services Administration (HRSA) is an agency of the U.S. Department of Health and Human Services located in North Bethesda, Maryland. It is the primary federal agency for improving access to health care services for people who are uninsured, isolated or medically vulnerable.

The United Network for Organ Sharing (UNOS) is a non-profit scientific and educational organization that administers the only Organ Procurement and Transplantation Network (OPTN) in the United States, established by the U.S. Congress in 1984 by Gene A. Pierce, founder of United Network for Organ Sharing. Located in Richmond, Virginia, the organization's headquarters are situated near the intersection of Interstate 95 and Interstate 64 in the Virginia BioTechnology Research Park.
The National Marrow Donor Program (NMDP) is a nonprofit organization founded in 1986 and based in Minneapolis, Minnesota, that operates the Be The Match Registry of volunteer hematopoietic cell donors and umbilical cord blood units in the United States.
Organ procurement is a surgical procedure that removes organs or tissues for reuse, typically for organ transplantation.
The Healthcare Systems Bureau is part of the Health Resources and Services Administration (HRSA), of the United States Department of Health and Human Services.
Organ trade is the trading of human organs, tissues, or other body products, usually for transplantation. According to the World Health Organization (WHO), organ trade is a commercial transplantation where there is a profit, or transplantations that occur outside of national medical systems. There is a global need or demand for healthy body parts for transplantation, which exceeds the numbers available.
Transplantable organs and tissues may refer to both organs and tissues that are relatively often transplanted, as well as organs and tissues which are relatively seldom transplanted. In addition to this it may also refer to possible-transplants which are still in the experimental stage.

The Gift of Life Marrow Registry is a public bone marrow and blood stem cell registry headquartered in Boca Raton, Florida. Gift of Life facilitates transplants for children and adults suffering from life-threatening illnesses, including leukemia, lymphoma, other cancers and genetic diseases.

Francis L. Delmonico, MD, FACS is a surgeon, clinical professor and health expert in the field of transplantation. He serves on numerous committees and is affiliated with various leading organizations and institutions. He is the chief medical officer of the New England Organ Bank (NEOB) and Professor of Surgery, Part-Time at Harvard Medical School in Boston, Massachusetts, where he is emeritus director of renal transplantation. He served as president of The Transplantation Society (TTS) from 2012 to 2014, an international non-profit organization based in Montreal, Canada that works with international transplantation physicians and researchers. He also served as the president of the United Network of Organ Sharing (UNOS) in 2005, which overseas the practice of organ donation and transplantation in the United States. He was appointed and still serves as an advisor to the World Health Organization in matters of organ donation and transplantation. He was appointed by Pope Francis to the Pontifical Academy of Science in 2016. In 2020, he became the recipient of the Medawar Prize of The Transplantation Society.
In the United States, an organ procurement organization (OPO) is a non-profit organization that is responsible for the evaluation and procurement of deceased-donor organs for organ transplantation. There are 57 such organizations in the United States, each responsible for organ procurement in a specific region, and each a member of the Organ Procurement and Transplantation Network (OPTN), a federally-mandated network managed by the United Network for Organ Sharing (UNOS) under federal contract. The individual OPOs represent the front line of organ procurement, having direct contact with the donor's hospital and the family of the recently deceased donor. Once the OPO receives authorization for donation from the decedent's family or through first-person authorization, it works with UNOS to identify the best candidates for the available organs, and coordinates with the surgical team for each organ recipient.

MOHAN Foundation is a not-for-profit, registered non-government charity organisation in India that works in the field of deceased organ donation and transplantation. MOHAN is an acronym for Multi Organ Harvesting Aid Network. It has offices in Chennai, Hyderabad, Bengaluru, Delhi, Mumbai, Chandigarh, Nagpur, Jaipur and information centers at Kerala and Imphal.

The HIV Organ Policy Equity Act is a law that modifies rules regarding organ donation between HIV-positive individuals. The law authorizes clinical research and the revision of rules about organ donation and transportation as a result of the research. Organs from HIV donors would only be going to individuals who are already HIV positive, but could lead to 600 additional organ transplants a year. The use of HIV-positive organs was previously a federal crime. This bill passed the United States Senate during the 113th United States Congress, and also passed the United States House of Representatives. It was signed into law as PL 113-51 by President Barack Obama on November 21, 2013.
Transplant coordinator is a healthcare professional – doctor, nurse, or allied health science graduate – who coordinates activities related to organ donation and transplantation. Transplant coordinators can either be Donor Coordinators or Recipient Coordinators.
Organ donation is when a person gives their organs after they die to someone in need of new organs. Transplantation is the process of transplanting the organs donated into another person. This process extends the life expectancy of a person suffering from organ failure. The number of patients requiring organ transplants outweighs the number of donor organs available.
Kidney paired donation (KPD), or paired exchange, is an approach to living donor kidney transplantation where patients with incompatible donors swap kidneys to receive a compatible kidney. KPD is used in situations where a potential donor is incompatible. Because better donor HLA and age matching are correlated with lower lifetime mortality and longer lasting kidney transplants, many compatible pairs are also participating in swaps to find better matched kidneys. In the United States, the National Kidney Registry organizes the majority of U.S. KPD transplants, including the largest swaps. The first large swap was a 60 participant chain in 2012 that appeared on the front page of the New York Times and the second, even larger swap, included 70 participants and was completed in 2014. Other KPD programs in the U.S. include the UNOS program, which was launched in 2010 and completed its 100th KPD transplant in 2014, and the Alliance for Paired Donation.
Organ transplantation in the Indian state of Tamil Nadu is regulated by India's Transplantation of Human Organs Act, 1994 and is facilitated by the Transplant Authority of Tamil Nadu (TRANSTAN) of the Government of Tamil Nadu and several NGOs. Tamil Nadu ranks first in India in deceased organ donation rate at 1.8 per million population, which is seven times higher than the national average.