Related Research Articles
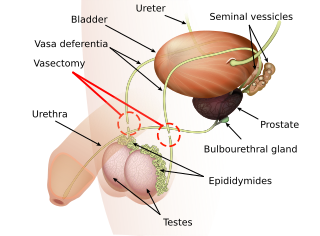
Vasectomy, is an elective surgical procedure for male sterilization or permanent contraception. During the procedure, the male vasa deferentia are cut and tied or sealed so as to prevent sperm from entering into the urethra and thereby prevent fertilization of a female through sexual intercourse. Vasectomies are usually performed in a physician's office, medical clinic, or, when performed on an animal, in a veterinary clinic. Hospitalization is not normally required as the procedure is not complicated, the incisions are small, and the necessary equipment routine.
Sterilization is any of a number of medical methods of birth control that intentionally leaves a person unable to reproduce. Sterilization methods include both surgical and non-surgical, and exist for both males and females. Sterilization procedures are intended to be permanent; reversal is generally difficult or impossible.

Tubal ligation is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked, clipped or removed. This prevents the fertilization of eggs by sperm and thus the implantation of a fertilized egg. Tubal ligation is considered a permanent method of sterilization and birth control.
Cauterization is a medical practice or technique of burning a part of a body to remove or close off a part of it. It destroys some tissue in an attempt to mitigate bleeding and damage, remove an undesired growth, or minimize other potential medical harm, such as infections when antibiotics are unavailable.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

A surgical instrument is a medical device for performing specific actions or carrying out desired effects during a surgery or operation, such as modifying biological tissue, or to provide access for viewing it. Over time, many different kinds of surgical instruments and tools have been invented. Some surgical instruments are designed for general use in all sorts of surgeries, while others are designed for only certain specialties or specific procedures.

Vas-occlusive contraception is a form of male contraception that blocks sperm transport in the vas deferens, the tubes that carry sperm from the epididymis to the ejaculatory ducts.
Vasovasostomy is a surgery by which vasectomies are partially reversed. Another surgery for vasectomy reversal is vasoepididymostomy.

There are many different surgical specialties, some of which require very specific kinds of surgical instruments to perform.
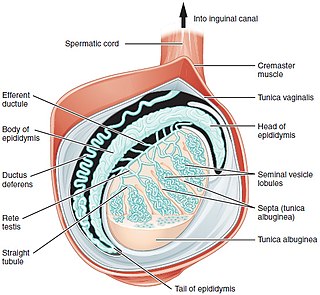
Testicular sperm extraction (TESE) is a surgical procedure in which a small portion of tissue is removed from the testicle and any viable sperm cells from that tissue are extracted for use in further procedures, most commonly intracytoplasmic sperm injection (ICSI) as part of in vitro fertilisation (IVF). TESE is often recommended to patients who cannot produce sperm by ejaculation due to azoospermia.
Ambulatory phlebectomy is a minisurgical treatment for superficial varicose veins and so-called side branches.
Post-vasectomy pain syndrome (PVPS) is a chronic and sometimes debilitating genital pain condition that may develop immediately or several years after vasectomy. Because this condition is a syndrome, there is no single treatment method, therefore efforts focus on mitigating/relieving the individual patient's specific pain. When pain in the epididymides is the primary symptom, post-vasectomy pain syndrome is often described as congestive epididymitis.
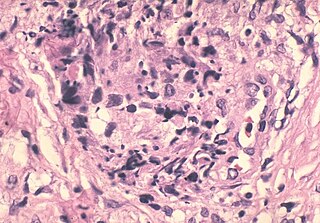
A sperm granuloma is a lump of leaked sperm that appears along the vasa deferentia or epididymides in vasectomized individuals. While the majority of sperm granulomas are present along the vas deferens, the rest of them form at the epididymis. Sperm granulomas range in size, from one millimeter to one centimeter. They consist of a central mass of degenerating sperm surrounded by tissue containing blood vessels and immune system cells. Sperm granulomas may also have a yellow, white, or cream colored center when cut open. While some sperm granulomas can be painful, most of them are painless and asymptomatic. Sperm granulomas can appear as a result of surgery, trauma, or an infection. They can appear as early as four days after surgery and fully formed ones can appear as late as 208 days later.
Urethroplasty is the surgical repair of an injury or defect within the walls of the urethra. Trauma, iatrogenic injury and infections are the most common causes of urethral injury/defect requiring repair. Urethroplasty is regarded as the gold standard treatment for urethral strictures and offers better outcomes in terms of recurrence rates than dilatations and urethrotomies. It is probably the only useful modality of treatment for long and complex strictures though recurrence rates are higher for this difficult treatment group.
Vasectomy reversal is a term used for surgical procedures that reconnect the male reproductive tract after interruption by a vasectomy. Two procedures are possible at the time of vasectomy reversal: vasovasostomy and vasoepididymostomy. Although vasectomy is considered a permanent form of contraception, advances in microsurgery have improved the success of vasectomy reversal procedures. The procedures remain technically demanding and may not restore the pre-vasectomy condition.
Reproductive surgery is surgery in the field of reproductive medicine. It can be used for contraception, e.g. in vasectomy, wherein the vasa deferentia of a male are severed, but is also used plentifully in assisted reproductive technology. Reproductive surgery is generally divided into three categories: surgery for infertility, in vitro fertilization, and fertility preservation.
Vasoepididymostomy or epididymovasostomy is a surgery by which vasectomies are reversed. It involves connection of the severed vas deferens to the epididymis and is more technically demanding than the vasovasostomy.
In surgery, a surgical incision is a cut made through the skin and soft tissue to facilitate an operation or procedure. Often, multiple incisions are possible for an operation. In general, a surgical incision is made as small and unobtrusive as possible to facilitate safe and timely operating conditions.
Circumcision surgical procedure in males involves either a conventional "cut and stitch" surgical procedure or use of a circumcision instrument or device. In the newborn period, almost all circumcisions are done by generalist physicians using one of three surgical instruments. In the US, the Gomco clamp is the most utilized instrument, followed by the Mogen clamp and the Plastibell. They are also used worldwide.

Ancient Roman surgical practices developed from Greek techniques. Roman surgeons and doctors usually learned through apprenticeships or studying. Ancient Roman doctors such as Galen and Celsus described Roman surgical techniques in their medical literature, such as De Medicina. These methods encompassed modern oral surgery, cosmetic surgery, sutures, ligatures, amputations, tonsillectomies, mastectomies, cataract surgeries, lithotomies, hernia repair, gynecology, neurosurgery, and others. Surgery was a rare practice, as it was dangerous and often had fatal results. To perform these procedures, they used tools such as specula, catheters, enemas, bone levers, osteotomes, phlebotomes, probes, curettes, bone drills, bone forceps, cupping vessels, knives, scalpels, scissors, and spathas.
References
- 1 2 3 4 5 Cook, Lynley A.; Pun, Asha; Gallo, Maria F.; Lopez, Laureen M.; Van Vliet, Huib A. A. M. (30 March 2014). "Scalpel versus no-scalpel incision for vasectomy". The Cochrane Database of Systematic Reviews. 2014 (3): CD004112. doi:10.1002/14651858.CD004112.pub4. ISSN 1469-493X. PMC 6464377 . PMID 24683021.
- ↑ Shattuck, Dominick; Perry, Brian; Packer, Catherine; Chin Quee, Dawn (23 December 2016). "A Review of 10 Years of Vasectomy Programming and Research in Low-Resource Settings". Global Health: Science and Practice. 4 (4): 647–660. doi:10.9745/GHSP-D-16-00235. ISSN 2169-575X. PMC 5199180 . PMID 28031302.
- 1 2 3 4 No-Scalpel Vasectomy: An Illustrated Guide for Surgeons (PDF). New York: Engender Health. 1997. Retrieved 17 November 2016.
- ↑ "World Vasectomy Day" (PDF).
- 1 2 "A Urologist Answers Questions About the No-Needle, No-Scalpel Vasectomy". UNC School of Medicine . 1 June 2019. Retrieved 22 April 2022.
- 1 2 Sharlip, Ira D.; Belker, Arnold M.; Honig, Stanton; Labrecque, Michel; Marmar, Joel L.; Ross, Lawrence S.; Sandlow, Jay I.; Sokal, David C. (December 2012). "Vasectomy: AUA Guideline". Journal of Urology. 188 (6S): 2482–2491. doi:10.1016/j.juro.2012.09.080. ISSN 0022-5347. PMID 23098786.
- ↑ "Complications of No-scalpel vasectomy". drvijayantgovinda.com. 25 September 2016.