Dentistry, also known as dental medicine and oral medicine, is the branch of medicine focused on the teeth, gums, and mouth. It consists of the study, diagnosis, prevention, management, and treatment of diseases, disorders, and conditions of the mouth, most commonly focused on dentition as well as the oral mucosa. Dentistry may also encompass other aspects of the craniofacial complex including the temporomandibular joint. The practitioner is called a dentist.

A dental dam or rubber dam is a thin, 6-inch (150 mm) square sheet, usually latex or nitrile, used in dentistry to isolate the operative site from the rest of the mouth. Sometimes termed "Kofferdam", it was designed in the United States in 1864 by Sanford Christie Barnum. It is used mainly in endodontic, fixed prosthodontic and general restorative treatments. Its purpose is both to prevent saliva interfering with the dental work, and to prevent instruments and materials from being inhaled, swallowed or damaging the mouth. In dentistry, use of a rubber dam is sometimes referred to as isolation or moisture control.

A dentist, also known as a dental surgeon, is a health care professional who specializes in dentistry, the branch of medicine focused on the teeth, gums, and mouth. The dentist's supporting team aids in providing oral health services. The dental team includes dental assistants, dental hygienists, dental technicians, and sometimes dental therapists.
Teeth cleaning is part of oral hygiene and involves the removal of dental plaque from teeth with the intention of preventing cavities, gingivitis, and periodontal disease. People routinely clean their own teeth by brushing and interdental cleaning, and dental hygienists can remove hardened deposits (tartar) not removed by routine cleaning. Those with dentures and natural teeth may supplement their cleaning with a denture cleaner.

An occupational injury is bodily damage resulting from working. The most common organs involved are the spine, hands, the head, lungs, eyes, skeleton, and skin. Occupational injuries can result from exposure to occupational hazards, such as temperature, noise, insect or animal bites, blood-borne pathogens, aerosols, hazardous chemicals, radiation, and occupational burnout.

This discussion of the dental amalgam controversy outlines the debate over whether dental amalgam should be used. Supporters claim that it is safe, effective and long-lasting, while critics argue that amalgam is unsafe because it may cause mercury poisoning and other toxicity.
Tooth whitening or tooth bleaching is the process of lightening the color of human teeth. Whitening is often desirable when teeth become yellowed over time for a number of reasons, and can be achieved by changing the intrinsic or extrinsic color of the tooth enamel. The chemical degradation of the chromogens within or on the tooth is termed as bleaching.

A herpetic whitlow is a herpes lesion (whitlow), typically on a finger or thumb, caused by the herpes simplex virus (HSV). Occasionally infection occurs on the toes or on the nail cuticle. Herpes whitlow can be caused by infection by HSV-1 or HSV-2. HSV-1 whitlow is often contracted by health care workers that come in contact with the virus; it is most commonly contracted by dental workers and medical workers exposed to oral secretions. It is also often observed in thumb-sucking children with primary HSV-1 oral infection (autoinoculation) prior to seroconversion, and in adults aged 20 to 30 following contact with HSV-2-infected genitals.

Dental assistants are members of the dental team. They support a dental operator in providing more efficient dental treatment. Dental assistants are distinguished from other groups of dental auxiliaries by differing training, roles and patient scopes.
A health professional, healthcare professional, or healthcare worker is a provider of health care treatment and advice based on formal training and experience. The field includes those who work as a nurse, physician, physician assistant, registered dietitian, veterinarian, veterinary technician, optometrist, pharmacist, pharmacy technician, medical assistant, physical therapist, occupational therapist, dentist, midwife, psychologist, audiologist, or healthcare scientist, or who perform services in allied health professions. Experts in public health and community health are also health professionals.
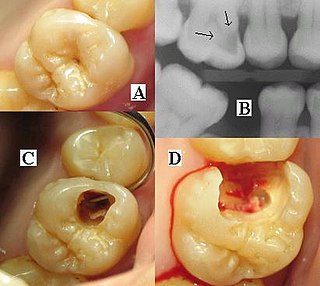
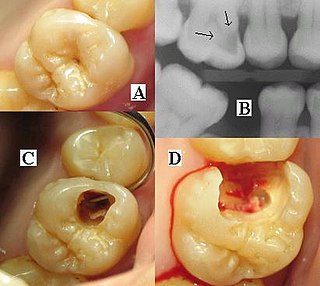
Dental radiographs, commonly known as X-rays, are radiographs used to diagnose hidden dental structures, malignant or benign masses, bone loss, and cavities.

In dentistry, amalgam is an alloy of mercury used to fill teeth cavities. It is made by mixing a combination of liquid mercury and particles of solid metals such a silver, copper or tin. The amalgam is mixed by the dentist just before use. It remains soft for a short while after mixing, which facilitates it being snugly packed into the cavity and shaped before it sets hard.

Dental fear, or dentophobia, is a normal emotional reaction to one or more specific threatening stimuli in the dental situation. However, dental anxiety is indicative of a state of apprehension that something dreadful is going to happen in relation to dental treatment, and it is usually coupled with a sense of losing control. Similarly, dental phobia denotes a severe type of dental anxiety, and is characterised by marked and persistent anxiety in relation to either clearly discernible situations or objects or to the dental setting in general. The term ‘dental fear and anxiety’ (DFA) is often used to refer to strong negative feelings associated with dental treatment among children, adolescents and adults, whether or not the criteria for a diagnosis of dental phobia are met. Dental phobia can include fear of dental procedures, dental environment or setting, fear of dental instruments or fear of the dentist as a person. People with dental phobia often avoid the dentist and neglect oral health, which may lead to painful dental problems and ultimately force a visit to the dentist. The emergency nature of this appointment may serve to worsen the phobia. This phenomenon may also be called the cycle of dental fear. Dental anxiety typically starts in childhood. There is the potential for this to place strains on relationships and negatively impact on employment.

Reproductive toxicity refers to the potential risk from a given chemical, physical or biologic agent to adversely affect both male and female fertility as well as offspring development. Reproductive toxicants may adversely affect sexual function, ovarian failure, fertility as well as causing developmental toxicity in the offspring. Lowered effective fertility related to reproductive toxicity relates to both male and female effects alike and is reflected in decreased sperm counts, semen quality and ovarian failure.

In occupational safety and health, hand arm vibrations (HAVs) are a specific type of occupational hazard which can lead to hand arm vibration syndrome.
Oral sedation dentistry is a medical procedure involving the administration of sedative drugs via an oral route, generally to facilitate a dental procedure and reduce patients anxiety related to the experience. Oral sedation is one of the available methods of conscious sedation dentistry, along with inhalation sedation and conscious intravenous sedation. Benzodiazepines are commonly used, specifically triazolam. Triazolam is commonly selected for its rapid onset and limited duration of effect. An initial dose is usually taken approximately one hour before the dental appointment. Treatment may include additional dosing on the night proceeding the procedure, to mitigate anxiety-related insomnia. The procedure is generally recognized as safe, with the effective dosages being below levels sufficient to impair breathing.
Eco-friendly dentistry aims at reducing the detrimental impact of dental services on the environment while still being able to adhere to the regulations and standards of the dental industries in their respective countries.

Inhalation sedation is a form of conscious sedation where an inhaled drug should:
- Depress the central nervous system (CNS) to an extent that surgeons can operate with minimal physiological and psychological stress to the patient
- Modify the patient's state of mind such that communication is maintained and the patient can respond to verbal command
- Carry a margin of safety wide enough to render the unintended loss of consciousness and loss of protective reflexes unlikely.

A dental aerosol is an aerosol that is produced from dental instrument, dental handpieces, three-way syringes, and other high-speed instruments. These aerosols may remain suspended in the clinical environment. Dental aerosols can pose risks to the clinician, staff, and other patients. The heavier particles contained within the aerosols are likely to remain suspended in the air for relatively short period and settle quickly onto surfaces, however, the lighter particles may remain suspended for longer periods and may travel some distance from the source. These smaller particles are capable of becoming deposited in the lungs when inhaled and provide a route of diseases transmission. Different dental instruments produce varying quantities of aerosol, and therefore are likely to pose differing risks of dispersing microbes from the mouth. Air turbine dental handpieces generally produce more aerosol, with electric micromotor handpieces producing less, although this depends on the configuration of water coolant used by the handpiece.

Hazard controls for COVID-19 in workplaces are the application of occupational safety and health methodologies for hazard controls to the prevention of COVID-19. Vaccination is the most effective way to protect against severe illness or death from COVID-19. Multiple layers of controls are recommended, including measures such as remote work and flextime, increased ventilation, personal protective equipment (PPE) and face coverings, social distancing, and enhanced cleaning programs.