Liver tumors are abnormal growth of liver cells on or in the liver. Several distinct types of tumors can develop in the liver because the liver is made up of various cell types. Liver tumors can be classified as benign (non-cancerous) or malignant (cancerous) growths. They may be discovered on medical imaging, and the diagnosis is often confirmed with liver biopsy. Signs and symptoms of liver masses vary from being asymptomatic to patients presenting with an abdominal mass, hepatomegaly, abdominal pain, jaundice, or some other liver dysfunction. Treatment varies and is highly specific to the type of liver tumor.

A teratoma is a tumor made up of several different types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the tailbone, ovary, or testicle.

An ovarian cyst is a fluid-filled sac within the ovary. Often they cause no symptoms. Occasionally they may produce bloating, lower abdominal pain, or lower back pain. The majority of cysts are harmless. If the cyst either breaks open or causes twisting of the ovary, it may cause severe pain. This may result in vomiting or feeling faint, and even cause head aches.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

A dermoid cyst is a teratoma of a cystic nature that contains an array of developmentally mature, solid tissues. It frequently consists of skin, hair follicles, and sweat glands, while other commonly found components include clumps of long hair, pockets of sebum, blood, fat, bone, nail, teeth, eyes, cartilage, and thyroid tissue.

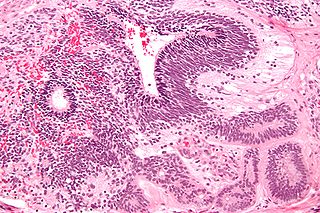
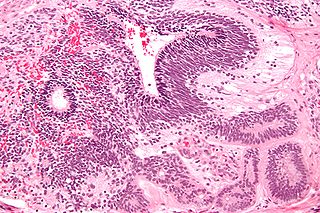
A serous tumour is a neoplasm that typically has papillary to solid formations of tumor cells with crowded nuclei, and which typically arises on the modified Müllerian-derived serous membranes that surround the ovaries in females. Such ovarian tumors are part of the surface epithelial-stromal tumour group of ovarian tumors. They are common neoplasms with a strong tendency to occur bilaterally, and they account for approximately a quarter of all ovarian tumors.

Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in this group are thought to be derived from the ovarian surface epithelium or from ectopic endometrial or fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This group of tumors accounts for 90% to 95% of all cases of ovarian cancer; however is mainly only found in postmenopausal women with the exception of the United States where 7% of cases occur in women under the age of 40. Serum CA-125 is often elevated but is only 50% accurate so it is not a useful tumor marker to assess the progress of treatment. 75% of women with epithelial ovarian cancer are found within the advanced-stages; however younger patients are more likely to have better prognoses than older patients.

Sex cord–gonadal stromal tumour is a group of tumours derived from the stromal component of the ovary and testis, which comprises the granulosa, thecal cells and fibrocytes. In contrast, the epithelial cells originate from the outer epithelial lining surrounding the gonad while the germ cell tumors arise from the precursor cells of the gametes, hence the name germ cell. In humans, this group accounts for 8% of ovarian cancers and under 5% of testicular cancers. Their diagnosis is histological: only a biopsy of the tumour can make an exact diagnosis. They are often suspected of being malignant prior to operation, being solid ovarian tumours that tend to occur most commonly in post menopausal women.

Germ cell tumor (GCT) is a neoplasm derived from the primordial germ cells. Germ-cell tumors can be cancerous or benign. Germ cells normally occur inside the gonads. GCTs that originate outside the gonads may be birth defects resulting from errors during development of the embryo.

Ovarian tumors, or ovarian neoplasms, are tumors arising from the ovary. They can be benign or malignant. They consist of mainly solid tissue, while ovarian cysts contain fluid.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
An immature teratoma is a teratoma that contains anaplastic immature elements, and is often synonymous with malignant teratoma. A teratoma is a tumor of germ cell origin, containing tissues from more than one germ cell line, It can be ovarian or testicular in its origin. and are almost always benign. An immature teratoma is thus a very rare tumor, representing 1% of all teratomas, 1% of all ovarian cancers, and 35.6% of malignant ovarian germ cell tumors. It displays a specific age of incidence, occurring most frequently in the first two decades of life and almost never after menopause. Unlike a mature cystic teratoma, an immature teratoma contains immature or embryonic structures. It can coexist with mature cystic teratomas and can constitute of a combination of both adult and embryonic tissue. The most common symptoms noted are abdominal distension and masses. Prognosis and treatment options vary and largely depend on grade, stage and karyotype of the tumor itself.
Primary fallopian tube cancer (PFTC), often just tubal cancer, is a malignant neoplasm that originates from the fallopian tube.
A borderline tumor, sometimes called low malignant potential (LMP) tumor, is a distinct but yet heterogeneous group of tumors defined by their histopathology as atypical epithelial proliferation without stromal invasion. It generally refers to such tumors in the ovary but borderline tumors may rarely occur at other locations as well.

Endodermal sinus tumor (EST) is a member of the germ cell tumor group of cancers. It is the most common testicular tumor in children under three, and is also known as infantile embryonal carcinoma. This age group has a very good prognosis. In contrast to the pure form typical of infants, adult endodermal sinus tumors are often found in combination with other kinds of germ cell tumor, particularly teratoma and embryonal carcinoma. While pure teratoma is usually benign, endodermal sinus tumor is malignant.

The ovarian fibroma, also fibroma, is a benign sex cord-stromal tumour.
Hyperthermic intrathoracic chemotherapy (HITOC) is part of a surgical strategy employed in the treatment of various pleural malignancies. The pleura in this situation could be considered to include the surface linings of the chest wall, lungs, mediastinum, and diaphragm. HITOC is the chest counterpart of HIPEC. Traditionally used in the treatment of malignant mesothelioma, a primary malignancy of the pleura, this modality has recently been evaluated in the treatment of secondary pleural malignancies.
Vulvar tumors are those neoplasms of the vulva. Vulvar and vaginal neoplasms make up a small percentage (3%) of female genital cancers. They can be benign or malignant. Vulvar neoplasms are divided into cystic or solid lesions and other mixed types. Vulvar cancers are those malignant neoplasms that originate from vulvar epithelium, while vulvar sarcomas develop from non-epithelial cells such as bone, cartilage, fat, muscle, blood vessels, or other connective or supportive tissue. Epithelial and mesenchymal tissue are the origin of vulvar tumors.
Ovarian germ cell tumors (OGCTs) are heterogeneous tumors that are derived from the primitive germ cells of the embryonic gonad, which accounts for about 2.6% of all ovarian malignancies. There are four main types of OGCTs, namely dysgerminomas, yolk sac tumor, teratoma, and choriocarcinoma.