Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types: acute pancreatitis, and chronic pancreatitis. Signs and symptoms of pancreatitis include pain in the upper abdomen, nausea and vomiting. The pain often goes into the back and is usually severe. In acute pancreatitis, a fever may occur, and symptoms typically resolve in a few days. In chronic pancreatitis weight loss, fatty stool, and diarrhea may occur. Complications may include infection, bleeding, diabetes mellitus, or problems with other organs.
Cholecystitis is inflammation of the gallbladder. Symptoms include right upper abdominal pain, pain in the right shoulder, nausea, vomiting, and occasionally fever. Often gallbladder attacks precede acute cholecystitis. The pain lasts longer in cholecystitis than in a typical gallbladder attack. Without appropriate treatment, recurrent episodes of cholecystitis are common. Complications of acute cholecystitis include gallstone pancreatitis, common bile duct stones, or inflammation of the common bile duct.

Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of pancreatic cancer are known.
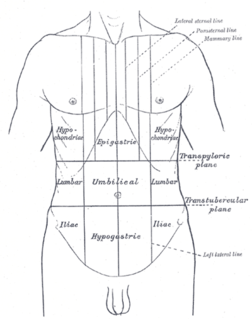
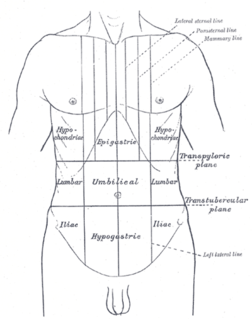
Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes in order of frequency include: 1) a gallstone impacted in the common bile duct beyond the point where the pancreatic duct joins it; 2) heavy alcohol use; 3) systemic disease; 4) trauma; 5) and, in minors, mumps. Acute pancreatitis may be a single event; it may be recurrent; or it may progress to chronic pancreatitis.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.

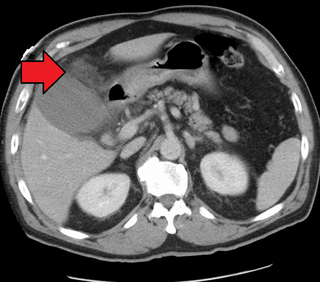
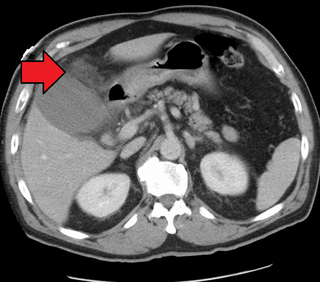
A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

A pancreatic fistula is an abnormal communication between the pancreas and other organs due to leakage of pancreatic secretions from damaged pancreatic ducts. An external pancreatic fistula is one that communicates with the skin, and is also known as a pancreaticocutaneous fistula, whereas an internal pancreatic fistula communicates with other internal organs or spaces. Pancreatic fistulas can be caused by pancreatic disease, trauma, or surgery.
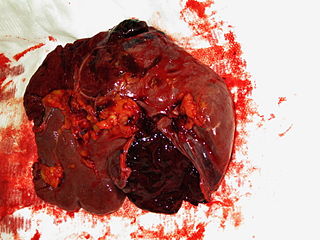
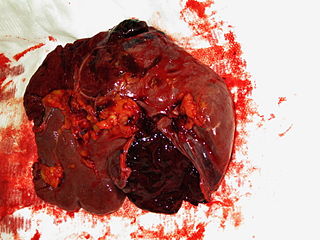
A splenic injury, which includes a ruptured spleen, is any injury to the spleen. The rupture of a normal spleen can be caused by trauma, such as a traffic collision.
Pancreatic divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts. Most individuals with pancreas divisum remain without symptoms or complications. A minority of people with pancreatic divisum may develop episodes of abdominal pain, nausea or vomiting due to acute or chronic pancreatitis. The presence of pancreas divisum is usually identified with cross sectional diagnostic imaging, such as MRI or computed tomography (CT) imaging. In some cases, endoscopic retrograde cholangiopancreatography (ERCP) is performed, revealing the diagnosis of pancreas divisum. If no symptoms or complications are present, then treatment is not necessary. However, if there is recurrent pancreatitis, then a sphincterotomy of the minor papilla may be indicated.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, is physical trauma or impactful force to a body part, often occurring with road traffic collisions, direct blows, assaults, injuries during sports, and particularly in the elderly who fall. It is contrasted with penetrating trauma which occurs when an object pierces the skin and enters a tissue of the body, creating an open wound and bruise.
Hemoperitoneum is the presence of blood in the peritoneal cavity. The blood accumulates in the space between the inner lining of the abdominal wall and the internal abdominal organs. Hemoperitoneum is generally classified as a surgical emergency; in most cases, urgent laparotomy is needed to identify and control the source of the bleeding. In selected cases, careful observation may be permissible. The abdominal cavity is highly distensible and may easily hold greater than five liters of blood, or more than the entire circulating blood volume for an average-sized individual. Therefore, large-scale or rapid blood loss into the abdomen will reliably induce hemorrhagic shock and, if untreated, may rapidly lead to death.

Abdominal ultrasonography is a form of medical ultrasonography to visualise abdominal anatomical structures. It uses transmission and reflection of ultrasound waves to visualise internal organs through the abdominal wall. For this reason, the procedure is also called a transabdominal ultrasound, in contrast to endoscopic ultrasound, the latter combining ultrasound with endoscopy through visualize internal structures from within hollow organs.
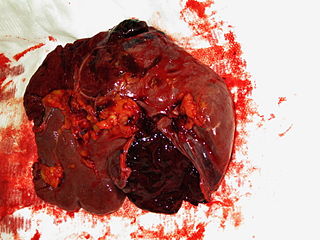
Blunt splenic trauma occurs when a significant impact to the spleen from some outside source damages or ruptures the spleen. Treatment varies depending on severity, but often consists of embolism or splenectomy.

Superior mesenteric artery (SMA) syndrome is a gastro-vascular disorder in which the third and final portion of the duodenum is compressed between the abdominal aorta (AA) and the overlying superior mesenteric artery. This rare, potentially life-threatening syndrome is typically caused by an angle of 6°–25° between the AA and the SMA, in comparison to the normal range of 38°–56°, due to a lack of retroperitoneal and visceral fat. In addition, the aortomesenteric distance is 2–8 millimeters, as opposed to the typical 10–20. However, a narrow SMA angle alone is not enough to make a diagnosis, because patients with a low BMI, most notably children, have been known to have a narrow SMA angle with no symptoms of SMA syndrome.

Abdominal trauma is an injury to the abdomen. Signs and symptoms include abdominal pain, tenderness, rigidity, and bruising of the external abdomen. Complications may include blood loss and infection.

Diaphragmatic rupture is a tear of the diaphragm, the muscle across the bottom of the ribcage that plays a crucial role in breathing. Most commonly, acquired diaphragmatic tears result from physical trauma. Diaphragmatic rupture can result from blunt or penetrating trauma and occurs in about 0.5% of all people with trauma.
An exploratory laparotomy is a general surgical operation where the abdomen is opened and the abdominal organs are examined for injury or disease. It is the standard of care in various blunt and penetrating trauma situations in which there may be life-threatening internal injuries. It is also used in certain diagnostic situations, in which the operation is undertaken in search of a unifying cause for multiple signs and symptoms of disease, and in the staging of some cancers.

A stab wound is a specific form of penetrating trauma to the skin that results from a knife or a similar pointed object. While stab wounds are typically known to be caused by knives, they can also occur from a variety of implements, including broken bottles and ice picks. Most stabbings occur because of intentional violence or through self-infliction. The treatment is dependent on many different variables such as the anatomical location and the severity of the injury. Even though stab wounds are inflicted at a much greater rate than gunshot wounds, they account for less than 10% of all penetrating trauma deaths.

A liver injury, also known as liver laceration, is some form of trauma sustained to the liver. This can occur through either a blunt force such as a car accident, or a penetrating foreign object such as a knife. Liver injuries constitute 5% of all traumas, making it the most common abdominal injury. Generally nonoperative management and observation is all that is required for a full recovery.