Related Research Articles
Palliative care is an interdisciplinary medical caregiving approach aimed at optimizing quality of life and mitigating suffering among people with serious, complex, and often terminal illnesses. Within the published literature, many definitions of palliative care exist. The World Health Organization (WHO) describes palliative care as "an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain, illnesses including other problems whether physical, psychosocial, and spiritual". In the past, palliative care was a disease specific approach, but today the WHO takes a broader patient-centered approach that suggests that the principles of palliative care should be applied as early as possible to any chronic and ultimately fatal illness. This shift was important because if a disease-oriented approach is followed, the needs and preferences of the patient are not fully met and aspects of care, such as pain, quality of life, and social support, as well as spiritual and emotional needs, fail to be addressed. Rather, a patient-centered model prioritizes relief of suffering and tailors care to increase the quality of life for terminally ill patients.

Torticollis, also known as wry neck, is a painful, dystonic condition defined by an abnormal, asymmetrical head or neck position, which may be due to a variety of causes. The term torticollis is derived from Latin tortus 'twisted' and collum 'neck'.

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a specific medical specialty devoted to pain, which is called pain medicine.
Premedication is using medication before some other therapy to prepare for that forthcoming therapy. Typical examples include premedicating with a sedative or analgesic before surgery; using prophylactic (preventive) antibiotics before surgery; and using antiemetics or antihistamines before chemotherapy.
Manual therapy, or manipulative therapy, is a part of Physiotherapy, it is a physical treatment primarily used by physical therapists, occupational therapists to treat musculoskeletal pain and disability; it mostly includes kneading and manipulation of muscles, joint mobilization and joint manipulation. It is also used by Rolfers, massage therapists, athletic trainers, osteopaths, and physicians.
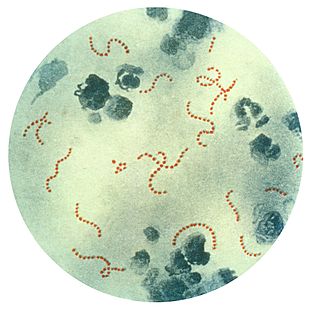
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) is a controversial hypothetical diagnosis for a subset of children with rapid onset of obsessive-compulsive disorder (OCD) or tic disorders. Symptoms are proposed to be caused by group A streptococcal (GAS), and more specifically, group A beta-hemolytic streptococcal (GABHS) infections. OCD and tic disorders are hypothesized to arise in a subset of children as a result of a post-streptococcal autoimmune process. The proposed link between infection and these disorders is that an autoimmune reaction to infection produces antibodies that interfere with basal ganglia function, causing symptom exacerbations, and this autoimmune response results in a broad range of neuropsychiatric symptoms.
Idiopathic pulmonary haemosiderosis (IPH) is a lung disease of unknown cause that is characterized by alveolar capillary bleeding and accumulation of haemosiderin in the lungs. It is rare, with an incidence between 0.24 and 1.23 cases per million people.
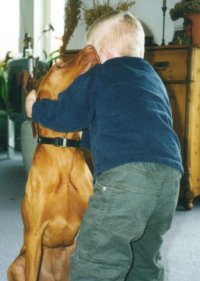
Animal-assisted therapy (AAT) is an alternative or complementary type of therapy that includes the use of animals in a treatment. The goal of this animal-assisted intervention is to improve a patient's social, emotional, or cognitive functioning. Studies have documented some positive effects of the therapy on subjective self-rating scales and on objective physiological measures such as blood pressure and hormone levels.

Alternative cancer treatment describes any cancer treatment or practice that is not part of the conventional standard of cancer care. These include special diets and exercises, chemicals, herbs, devices, and manual procedures. Most alternative cancer treatments do not have high-quality evidence supporting their use and many have been described as fundamentally pseudoscientific. Concerns have been raised about the safety of some purported treatments and some have been found unsafe in clinical trials. Despite this, many untested and disproven treatments are used around the world.
Child psychotherapy, or mental health interventions for children refers to the psychological treatment of various mental disorders diagnosed in children and adolescents. The therapeutic techniques developed for younger age ranges specialize in prioritizing the relationship between the child and the therapist. The goal of maintaining positive therapist-client relationships is typically achieved using therapeutic conversations and can take place with the client alone, or through engagement with family members.

Major depressive disorder, often simply referred to as depression, is a mental disorder characterized by prolonged unhappiness or irritability. It is accompanied by a constellation of somatic and cognitive signs and symptoms such as fatigue, apathy, sleep problems, loss of appetite, loss of engagement, low self-regard/worthlessness, difficulty concentrating or indecisiveness, or recurrent thoughts of death or suicide.
Game addiction problems can induce repetitive strain injuries, skin disorders or other health issues. Other problems include video game-provoked seizures in patients with epilepsy. In rare and extreme cases, deaths have resulted from excessive video game playing.
Pain in babies, and whether babies feel pain, has been a large subject of debate within the medical profession for centuries. Prior to the late nineteenth century it was generally considered that babies hurt more easily than adults. It was only in the last quarter of the 20th century that scientific techniques finally established babies definitely do experience pain – probably more than adults – and developed reliable means of assessing and of treating it. As recently as 1999, it was widely believed by medical professionals that babies could not feel pain until they were a year old, but today it is believed newborns and likely even fetuses beyond a certain age can experience pain.

Trauma in children, also known as pediatric trauma, refers to a traumatic injury that happens to an infant, child or adolescent. Because of anatomical and physiological differences between children and adults the care and management of this population differs.
Pediatric psychology is a multidisciplinary field of both scientific research and clinical practice which attempts to address the psychological aspects of illness, injury, and the promotion of health behaviors in children, adolescents, and families in a pediatric health setting. Psychological issues are addressed in a developmental framework and emphasize the dynamic relationships which exist between children, their families, and the health delivery system as a whole.
Childhood chronic illness refers to conditions in pediatric patients that are usually prolonged in duration, do not resolve on their own, and are associated with impairment or disability. The duration required for an illness to be defined as chronic is generally greater than 12 months, but this can vary, and some organizations define it by limitation of function rather than a length of time. Regardless of the exact length of duration, these types of conditions are different than acute, or short-lived, illnesses which resolve or can be cured. There are many definitions for what counts as a chronic condition. However, children with chronic illnesses will typically experience at least one of the following: limitation of functions relative to their age, disfigurement, dependency on medical technologies or medications, increased medical attention, and a need for modified educational arrangements.

Chest pain in children is the pain felt in the chest by infants, children and adolescents. In most cases the pain is not associated with the heart. It is primarily identified by the observance or report of pain by the infant, child or adolescent by reports of distress by parents or caregivers. Chest pain is not uncommon in children. Many children are seen in ambulatory clinics, emergency departments and hospitals and cardiology clinics. Most often there is a benign cause for the pain for most children. Some have conditions that are serious and possibly life-threatening. Chest pain in pediatric patients requires careful physical examination and a detailed history that would indicate the possibility of a serious cause. Studies of pediatric chest pain are sparse. It has been difficult to create evidence-based guidelines for evaluation.

Childhood chronic pain affects at least 5% of the population under the age of 18, according to conservative epidemiological studies. Rates of pediatric chronic pain have also increased in the past 20 years. While chronic pain conditions vary significantly in severity, they often affect children's mental health, academic performance, activities of daily living, social participation, and general quality of life. The outcomes of childhood chronic pain are affected by a number of factors, including demographic factors, genetics, access to rehabilitation services, and school and family support.

Pain management in children is the assessment and treatment of pain in infants and children.
Tiffany Martini Field is professor in the departments of pediatrics, psychology, and psychiatry at the University of Miami School of Medicine and director of the Touch Research Institute. She specializes in infant development, especially with regard to the impact of maternal postpartum depression on mother-infant interaction and the efficacy of massage and touch therapy in promoting growth and emotional well-being in premature and low birth weight infants.
References
- ↑ Beider S, Mahrer NE, Gold JI (December 2007). "Pediatric massage therapy: an overview for clinicians". Pediatr. Clin. North Am. 54 (6): 1025–41, xii–xiii. doi:10.1016/j.pcl.2007.10.001. PMID 18061789.
- ↑ Bennett, Cathy; Underdown, Angela; Barlow, Jane (2013-04-30). "Massage for promoting mental and physical health in typically developing infants under the age of six months". The Cochrane Database of Systematic Reviews (4): CD005038. doi:10.1002/14651858.CD005038.pub3. ISSN 1469-493X. PMC 8078453 . PMID 23633323.
- ↑ Vickers A, Ohlsson A, Lacy JB, Horsley A (2004). "Massage for promoting growth and development of preterm and/or low birth-weight infants". Cochrane Database Syst Rev (2): CD000390. doi:10.1002/14651858.CD000390.pub2. PMC 6956667 . PMID 15106151.
- ↑ Field T.; Morrow C.; Valdeon C.; Larson S.; Kuhn C.; Schanberg S. (1992). "Massage reduces depression and anxiety in child and adolescent psychiatric patients". Journal of the American Academy of Child & Adolescent Psychiatry. 31 (1): 125–131. doi: 10.1097/00004583-199201000-00019 . PMID 1537763.
- ↑ Field T.; Grizzle N.; Scafidi F.; Schanberg S. (1996). "Massage and relaxation therapies' effects on depressed adolescent mothers". Adolescence. 31 (124): 903–911. PMID 8970662.
- 1 2 Oz Mehmet C.; Whitworth Gerard C.; Liu Eric H. (1998). "Complementary Medicine in the Surgical Wards". JAMA. 279 (9): 710–711. doi:10.1001/jama.279.9.710-jms0304-5-1. PMID 9496995.
- 1 2 Haun JN, Graham-Pole J, Shortley B (Jun 2009). "Children with cancer and blood diseases experience positive physical and psychological effects from massage therapy". Int J Ther Massage Bodywork. 2 (2): 7–14. doi:10.3822/ijtmb.v2i2.12. PMC 3091462 . PMID 21589728.
- ↑ Hernandez-Reif M, Shor-Posner G, Baez J, Soto S, Mendoza R, Castillo R, Quintero N, Perez E, Zhang G (Sep 2008). "Dominican Children with HIV not Receiving Antiretrovirals: Massage Therapy Influences their Behavior and Development". Evid Based Complement Alternat Med. 5 (3): 345–354. doi:10.1093/ecam/nem032. PMC 2529379 . PMID 18830444.
- 1 2 3 Hughes D, Ladas E, Rooney D, Kelly K (May 2008). "Massage therapy as a supportive care intervention for children with cancer". Oncol Nurs Forum. 35 (3): 431–42. doi:10.1188/08.onf.431-442. PMID 18467292. S2CID 6266704.
- ↑ Pediatric massage therapy: an overview for clinicians. Beider S, Mahrer NE, Gold JI" Pediatr Clin North Am. 2007 Dec;54(6):1025-41.
- ↑ Mencía SB, López-Herce JC, Freddi N. "Analgesia and sedation in children: practical approach for the most frequent situations. J Pediatr (Rio J). 2007 May;83(2 Suppl):S71-82.
- ↑ Evelyn, Haly. "부산출장" . Retrieved 16 October 2023.
- ↑ Ali S, Drendel AL, Kircher J, Beno S (Jul 2010). "Pain management of musculoskeletal injuries in children: current state and future directions". Pediatr Emerg Care. 26 (7): 518–24. doi:10.1097/pec.0b013e3181e5c02b. PMID 20622635. S2CID 28302486.
- ↑ Parlak Gürol A, Polat S, Akçay MN (May 2010). "Itching, pain, and anxiety levels are reduced with massage therapy in burned adolescents". J Burn Care Res. 31 (3): 429–32. doi:10.1097/bcr.0b013e3181db522c. PMID 20453734. S2CID 3679959.
- ↑ Von Stülpnagel C, Reilich P, Straube A, Schäfer J, Blaschek A, Lee SH, Müller-Felber W, Henschel V, Mansmann U, Heinen F (Apr 2009). "Myofascial trigger points in children with tension-type headache: a new diagnostic and therapeutic option. J" (PDF). Child Neurol. 24 (4): 406–9. doi:10.1177/0883073808324540. PMID 19339283. S2CID 11461767.
- ↑ Diego MA, Field T, Hernandez-Reif M (Apr 2009). "Procedural pain heart rate responses in massaged preterm infants". Infant Behav. Dev. 32 (2): 226–9. doi:10.1016/j.infbeh.2008.12.001. PMC 2694508 . PMID 19185352.
- ↑ Evans S, Tsao JC, Zeltzer LK (Sep 2008). "Complementary and alternative medicine for acute procedural pain in children". Altern Ther Health Med. 14 (5): 52–6. PMID 18780584.
- 1 2 Suresh S, Wang S, Porfyris S, Kamasinski-Sol R, Steinhorn DM (Sep 2008). "Massage therapy in outpatient pediatric chronic pain patients: do they facilitate significant reductions in levels of distress, pain, tension, discomfort, and mood alterations?". Paediatr Anaesth. 18 (9): 884–7. doi:10.1111/j.1460-9592.2008.02638.x. PMID 18768049.
- ↑ Lowe RM, Hashkes PJ (Oct 2008). "Growing pains: a noninflammatory pain syndrome of early childhood". Nat Clin Pract Rheumatol. 4 (10): 542–9. doi:10.1038/ncprheum0903. PMID 18762787. S2CID 8894456.
- ↑ Procianoy RS, Mendes EW, Silveira RC (Jan 2010). "Massage therapy improves neurodevelopment outcome at two years corrected age for very low birth weight infants". Early Human Development. 86 (1): 7–11. doi:10.1016/j.earlhumdev.2009.12.001. PMID 20022717.
- ↑ Kemper KJ, Shannon S (Dec 2007). "Complementary and alternative medicine therapies to promote healthy moods". Pediatr Clin North Am. 54 (6): 901–26. doi:10.1016/j.pcl.2007.09.002. PMC 2329575 . PMID 18061783.
- ↑ Zebracki K, Holzman K, Bitter KJ, Feehan K, Miller ML (Sep 2007). "Brief report: use of complementary and alternative medicine and psychological functioning in Latino children with juvenile idiopathic arthritis or arthralgia". J Pediatr Psychol. 32 (8): 1006–10. doi: 10.1093/jpepsy/jsm033 . PMID 17626068.
- ↑ Diego M.A.; Hernandez-Reif M.; Field T.; Friedman L.; Shaw K. (2001). "HIV adolescents show improved immune function following massage therapy". International Journal of Neuroscience. 106 (1–2): 35–45. doi:10.3109/00207450109149736. PMID 11264907. S2CID 32089766.
- 1 2 Field T.; Cullen C.; Diego M.; Hernandez-Reif M.; Sprinz P.; Beebe K.; Kissel B.; Bango-Sanchez V. (2001). "Leukemia immune changes following massage therapy". Journal of Bodywork and Movement Therapies. 3 (4): 1–5. doi:10.1054/jbmt.2001.0228.
- ↑ Pediatric massage therapy: an overview for clinicians. Beider S, Mahrer NE, Gold JI" Pediatr Clin North Am. 2007 Dec;54(6) 1025-41; xii-xiii. Review.
- ↑ Green AD, Alioto A, Mousa H, Di Lorenzo C (Apr 2011). "Severe pediatric rumination syndrome: successful interdisciplinary inpatient management". J Pediatr Gastroenterol Nutr. 52 (4): 414–8. doi: 10.1097/mpg.0b013e3181fa06f3 . PMID 21407115. S2CID 8299506.
- ↑ Field T.; Morrow C.; Valdeon C.; Larson S.; Kuhn C.; Schanberg S. (1992). "Massage therapy reduces anxiety in child and adolescent psychiatric patients". Journal of the American Academy of Child and Adolescent Psychiatry. 31 (1): 125–130. doi: 10.1097/00004583-199201000-00019 . PMID 1537763.
- ↑ Field T.; Kilmer T.; Hernandez-Reif M.; Burman I. (1996). "Preschool Children's Sleep and Wake Behavior: Effects of massage therapy". Early Child Development and Care. 120: 39–44. doi:10.1080/0300443961200104.
- ↑ Cullen C.; Field T.; Escalona A.; Hartshorn K. (2000). "Father-infants interactions are enhanced by massage therapy". Early Child Development and Care. 164: 41–47. doi:10.1080/0300443001640104. S2CID 145180279.
- 1 2 Miller Laura J (2002). "Postpartum Depression". JAMA. 287 (6): 762–765. doi:10.1001/jama.287.6.762. PMID 11851544.
- ↑ Hart S.; Field T.; Hernandez-Reif M.; Lundy B. (1998). "Preschoolers' cognitive performance improves following massage". Early Child Development & Care. 143: 59–64. doi:10.1080/0300443981430105.
- ↑ Knapp Miland E (1960). "Physical Medicine in Rehabilitation for Arthritis in Children". JAMA. 174 (15): 1951–1953. doi:10.1001/jama.1960.03030150039010. PMID 13757053.
- ↑ Field T.; Lasko D.; Mundy P.; Henteleff T.; Talpins S.; Dowling M. (1986). "Autistic children's attentiveness and responsitivity improved after touch therapy". Journal of Autism and Developmental Disorders. 27 (3): 329–334. doi:10.1023/A:1025858600220. PMID 9229263. S2CID 12306795.
- ↑ Escalona A.; Field T.; Singer-Strunck R.; Cullen C.; Hartshorn K. (2001). "Brief report: improvements in the behavior of children with autism following massage therapy". Journal of Autism and Developmental Disorders. 31 (5): 513–516. doi:10.1023/a:1012273110194. PMID 11794416. S2CID 13400410.
- ↑ Hartshorn K.; Olds L.; Field T.; Delage J.; Cullen C.; Escalona A. (2001). "Creative movement therapy benefits children with autism". Early Child and Development and Care. 166: 1–5. doi:10.1080/0300443011660101. S2CID 143486019.
- ↑ Hernandez-Reif M.; Field T.; Krasnegor J.; Martinez E. (1999). "Cystic fibrosis symptoms are reduced with massage therapy intervention". Journal of Pediatric Psychology. 24 (2): 183–189. doi:10.1093/jpepsy/24.2.175. PMID 10361400.
- ↑ Anbar RD, Murthy VV (Sep 2010). "Reestablishment of hope as an intervention for a patient with cystic fibrosis awaiting lung transplantation". J Altern Complement Med. 16 (9): 1007–10. doi:10.1089/acm.2010.0107. PMID 20799891.
- ↑ Field T.; Seligman S.; Scafidi F.; Schanberg S. (1996). "Alleviating posttraumatic stress in children following Hurricane Andrew". Journal of Applied Developmental Psychology. 17: 37–50. doi: 10.1016/s0193-3973(96)90004-0 .
- ↑ April KT, Walji R (Feb 2011). "The state of research on complementary and alternative medicine in pediatric rheumatology". Rheum Dis Clin North Am. 37 (1): 85–94. doi:10.1016/j.rdc.2010.11.011. PMID 21220088.
- ↑ Beider S, Mahrer NE, Gold JI. "Pediatric massage therapy: an overview for clinicians" Pediatr Clin North Am. 2007 Dec;54(6):1025-41; xii-xiii. Review.