Scabies is a contagious human skin infestation by the tiny (0.2–0.45 mm) mite Sarcoptes scabiei, variety hominis. The word is from Latin: scabere, lit. 'to scratch'. The most common symptoms are severe itchiness and a pimple-like rash. Occasionally, tiny burrows may appear on the skin. In a first-ever infection, the infected person usually develops symptoms within two to six weeks. During a second infection, symptoms may begin within 24 hours. These symptoms can be present across most of the body or just certain areas such as the wrists, between fingers, or along the waistline. The head may be affected, but this is typically only in young children. The itch is often worse at night. Scratching may cause skin breakdown and an additional bacterial infection in the skin.

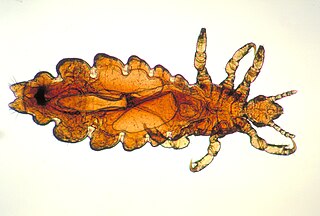
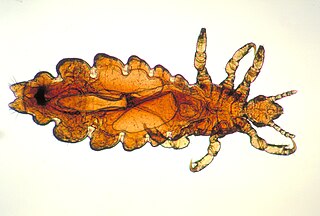
Louse is the common name for any member of the clade Phthiraptera, which contains nearly 5,000 species of wingless parasitic insects. Phthiraptera has variously been recognized as an order, infraorder, or a parvorder, as a result of developments in phylogenetic research.

Sucking lice have around 500 species and represent the smaller of the two traditional superfamilies of lice. As opposed to the paraphyletic chewing lice, which are now divided among three suborders, the sucking lice are monophyletic.

The crab louse or pubic louse is an insect that is an obligate ectoparasite of humans, feeding exclusively on blood. The crab louse usually is found in the person's pubic hair. Although the louse cannot jump, it can also live in other areas of the body that are covered with coarse hair, such as the perianal area, the entire body, and the eyelashes.

Pubic hair is terminal body hair that is found in the genital area of adolescent and adult humans. The hair is located on and around the sex organs and sometimes at the top of the inside of the thighs. In the pubic region around the pubis bone and the mons pubis that covers it, it is known as a pubic patch. Pubic hair is also found on the scrotum and base of the penile shaft in males and on the vulva in females.
Pediculosis is an infestation of lice from the sub-order Anoplura, family Pediculidae. Accordingly, the infestation with head lice is named pediculosis capitis, while this with body lice, pediculosis corporis. Although pediculosis in humans may properly refer to lice infestation of any part of the body, the term is sometimes used loosely to refer to pediculosis capitis, the infestation of the human head with the specific head louse.

The head louse is an obligate ectoparasite of humans. Head lice are wingless insects that spend their entire lives on the human scalp and feed exclusively on human blood. Humans are the only known hosts of this specific parasite, while chimpanzees and bonobos host a closely related species, Pediculus schaeffi. Other species of lice infest most orders of mammals and all orders of birds.

The treatment of human lice is the removal of head lice parasites from human hair. It has been debated and studied for centuries. However, the number of cases of human louse infestations has increased worldwide since the mid-1960s, reaching hundreds of millions annually. There is no product or method that assures 100% destruction of the eggs and hatched lice after a single treatment. However, there are a number of treatment modalities that can be employed with varying degrees of success. These methods include chemical treatments, natural products, combs, shaving, hot air, and silicone-based lotions.

The body louse is a hematophagic ectoparasite louse that infests humans. It is one of three lice which infest humans, the other two being the head louse, and the crab louse or pubic louse.
A louse is a wingless insect.

Head lice infestation, also known as pediculosis capitis, is the infection of the head hair and scalp by the head louse. Itching from lice bites is common. During a person's first infection, the itch may not develop for up to six weeks. If a person is infected again, symptoms may begin much more quickly. The itch may cause problems with sleeping. Generally, however, it is not a serious condition. While head lice appear to spread some other diseases in Africa, they do not appear to do so in Europe or North America.

A sexually transmitted infection (STI), also referred to as a sexually transmitted disease (STD) and the older term venereal disease (VD), is an infection that is spread by sexual activity, especially vaginal intercourse, anal sex, oral sex, or sometimes manual sex. STIs often do not initially cause symptoms, which results in a risk of passing the infection on to others. Symptoms and signs of STIs may include vaginal discharge, penile discharge, ulcers on or around the genitals, and pelvic pain. Some STIs can cause infertility.

No nit policy is a public health policy implemented by some education authorities to prevent the transmission of head lice infestation. The "no nit" policy requires the sending home and barring of all children who have nits on their hair from controlled settings such as school, summer camp or day care facilities. The CDC, American Academy of Pediatrics (AAP) and the National Association of School Nurses (NASN) advocate that "no-nit" policies should be discontinued, due in part because nits, the eggs or empty egg shells, are not transmissible and the burden of unnecessary absenteeism to the students, families and communities far outweighs the risks associated with head lice. Proponents of the no-nit policy counter that only a consistently nit-free child can be reliably shown to be infestation-free. That is, the presence of nits serves as a proxy for infestation status. Proponents argue that such a proxy is necessary because lice screening is prone to false negative conclusions.
An ectoparasitic infestation is a parasitic disease caused by organisms that live primarily on the surface of the host.

Pediculosis corporis or Vagabond's disease is a cutaneous condition caused by body lice that lay their eggs on clothing and to a lesser extent on human hairs.

Pthirus gorillae or gorilla louse is a species of parasitic sucking louse that afflicts gorillas. It is found in the African continent, specifically in Rwanda and Democratic Republic of the Congo. P. gorillae and P. pubis are the only known species that belong to the genus Pthirus, often incorrectly spelled as Phthirus. It is suggested that it is transmitted among its hosts by social grooming, shared bedding and sexual contact.

Pthirus is a genus of lice. There are only two extant species, and they are the sole known members of the family Pthiridae. Pthirus gorillae infests gorillas, and Pthirus pubis afflicts humans, and is commonly known as the crab louse or pubic louse. The two species diverged some 3.3 million years ago.

Trichodectes canis, also known as canine chewing louse, is a chewing louse found on domesticated dogs and wild canids throughout the world. T. canis is a well-known vector for the dog tapeworm, Dipylidium caninum. T. canis usually does not present any major problems to the host, however, can be very irritating in heavy infestations. In North America and most developed countries, T. canis infestation of domesticated dogs is very uncommon as long as they are properly cared for and healthy. Poorly taken care of dogs are more prone to getting a lice infestation.

Haematopinus suis, the hog louse, is one of the largest members of the louse suborder Anoplura, which consists of sucking lice that commonly afflict a number of mammals. H. suis is found almost solely on the skin surface of swine, and takes several blood meals a day from its host. H. suis has large claws that enable it to grasp a hog's hair and move around its body. It is easily seen without magnification, being 5–6 millimetres (0.20–0.24 in) long. H. suis has a long, narrow head and long mouthparts adapted for sucking blood. It is the only louse found on swine. H. suis infestation is relatively rare in the US; a 2004 study found that about 14% of German swine farms had H. suis infestations. Due to the frequency of feeding, infected swine become severely irritated, often rubbing themselves to the point of injuring their skin and displacing body hair. Particularly afflicted hogs may become almost completely bald and, in young hogs, the resulting stress can arrest growth, a cause of concern for farmers.
Mutual monogamy is a form of monogamy that exists when two partners agree to be sexually active with only one another. Being in a long-term mutually monogamous relationship reduces the risk of acquiring a sexually transmitted infection (STI). It is one of the most reliable ways to avoid STIs. Those who choose mutual monogamy can be tested before the sexual relationship to be certain they are not infected. This strategy for the prevention of acquiring a sexually transmitted infection requires that each partner remain faithful and does not engage in sexual activity with another partner.