X-ray radiation, or, much less commonly, X-radiation, is a penetrating form of high-energy electromagnetic radiation. Most X-rays have a wavelength ranging from 10 nanometers to 10 picometers, corresponding to frequencies in the range 30 petahertz to 30 exahertz (3×1016 Hz to 3×1019 Hz) and energies in the range 124 keV to 145 eV, respectively. X-ray wavelengths are shorter than those of UV rays and typically longer than those of gamma rays. In many languages, X-radiation is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it on November 8, 1895. He named it X-radiation to signify an unknown type of radiation. Spellings of X-ray(s) in English include the variants x-ray(s), xray(s), and X ray(s).

A computed tomography scan is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers or radiology technologists.

Radiography is an imaging technique using X-rays, gamma rays, or similar ionizing radiation and non-ionizing radiation to view the internal form of an object. Applications of radiography include medical radiography and industrial radiography. Similar techniques are used in airport security. To create an image in conventional radiography, a beam of X-rays is produced by an X-ray generator and is projected toward the object. A certain amount of the X-rays or other radiation is absorbed by the object, dependent on the object's density and structural composition. The X-rays that pass through the object are captured behind the object by a detector. The generation of flat two dimensional images by this technique is called projectional radiography. In computed tomography an X-ray source and its associated detectors rotate around the subject which itself moves through the conical X-ray beam produced. Any given point within the subject is crossed from many directions by many different beams at different times. Information regarding attenuation of these beams is collated and subjected to computation to generate two dimensional images in three planes which can be further processed to produce a three dimensional image.

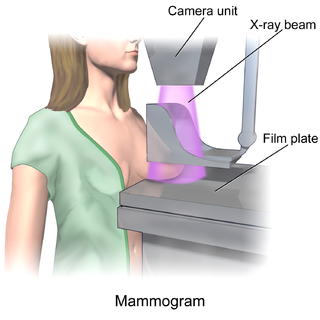
Mammography is the process of using low-energy X-rays to examine the human breast for diagnosis and screening. The goal of mammography is the early detection of breast cancer, typically through detection of characteristic masses or microcalcifications.

A gamma camera (γ-camera), also called a scintillation camera or Anger camera, is a device used to image gamma radiation emitting radioisotopes, a technique known as scintigraphy. The applications of scintigraphy include early drug development and nuclear medical imaging to view and analyse images of the human body or the distribution of medically injected, inhaled, or ingested radionuclides emitting gamma rays.

Technetium (99mTc) sestamibi (INN) is a pharmaceutical agent used in nuclear medicine imaging. The drug is a coordination complex consisting of the radioisotope technetium-99m bound to six (sesta=6) methoxyisobutylisonitrile (MIBI) ligands. The anion is not defined. The generic drug became available late September 2008. A scan of a patient using MIBI is commonly known as a "MIBI scan".
Charge sharing is an effect of signal degradation through transfer of charges from one electronic domain to another.
X-ray optics is the branch of optics that manipulates X-rays instead of visible light. It deals with focusing and other ways of manipulating the X-ray beams for research techniques such as X-ray crystallography, X-ray fluorescence, small-angle X-ray scattering, X-ray microscopy, X-ray phase-contrast imaging, and X-ray astronomy.

Tomosynthesis, also digital tomosynthesis (DTS), is a method for performing high-resolution limited-angle tomography at radiation dose levels comparable with projectional radiography. It has been studied for a variety of clinical applications, including vascular imaging, dental imaging, orthopedic imaging, mammographic imaging, musculoskeletal imaging, and chest imaging.
A Compound refractive lens (CRL) is a series of individual lenses arranged in a linear array in order to achieve focusing of X-rays in the energy range of 5-40 keV. They are an alternative to the KB mirror.

Flat-panel detectors are a class of solid-state x-ray digital radiography devices similar in principle to the image sensors used in digital photography and video. They are used in both projectional radiography and as an alternative to x-ray image intensifiers (IIs) in fluoroscopy equipment.

Positron emission mammography (PEM) is a nuclear medicine imaging modality used to detect or characterise breast cancer. Mammography typically refers to x-ray imaging of the breast, while PEM uses an injected positron emitting isotope and a dedicated scanner to locate breast tumors. Scintimammography is another nuclear medicine breast imaging technique, however it is performed using a gamma camera. Breasts can be imaged on standard whole-body PET scanners, however dedicated PEM scanners offer advantages including improved resolution.

Phase-contrast X-ray imaging or phase-sensitive X-ray imaging is a general term for different technical methods that use information concerning changes in the phase of an X-ray beam that passes through an object in order to create its images. Standard X-ray imaging techniques like radiography or computed tomography (CT) rely on a decrease of the X-ray beam's intensity (attenuation) when traversing the sample, which can be measured directly with the assistance of an X-ray detector. However, in phase contrast X-ray imaging, the beam's phase shift caused by the sample is not measured directly, but is transformed into variations in intensity, which then can be recorded by the detector.

X-ray detectors are devices used to measure the flux, spatial distribution, spectrum, and/or other properties of X-rays.

Photon counting is a technique in which individual photons are counted using a single-photon detector (SPD). A single-photon detector emits a pulse of signal for each detected photon. The counting efficiency is determined by the quantum efficiency and the system's electronic losses.
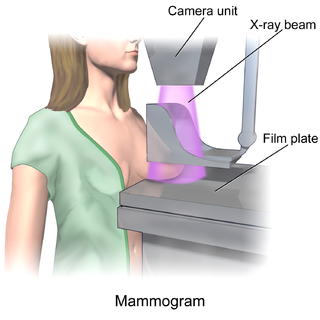
In medicine, breast imaging is a sub-speciality of diagnostic radiology that involves imaging of the breasts for screening or diagnostic purposes. There are various methods of breast imaging using a variety of technologies as described in detail below. Traditional screening and diagnostic mammography uses x-ray technology and has been the mainstay of breast imaging for many decades. Breast tomosynthesis is a relatively new digital x-ray mammography technique that produces multiple image slices of the breast similar to, but distinct from, computed tomography (CT). Xeromammography and galactography are somewhat outdated technologies that also use x-ray technology and are now used infrequently in the detection of breast cancer. Breast ultrasound is another technology employed in diagnosis and screening that can help differentiate between fluid filled and solid lesions, an important factor to determine if a lesion may be cancerous. Breast MRI is a technology typically reserved for high-risk patients and patients recently diagnosed with breast cancer. Lastly, scintimammography is used in a subgroup of patients who have abnormal mammograms or whose screening is not reliable on the basis of using traditional mammography or ultrasound.
Jeffrey Harold Siewerdsen is an American physicist and biomedical engineer who is a Professor of Biomedical Engineering, Computer Science, Radiology, and Neurosurgery at Johns Hopkins University. He is Co-Director of the Carnegie Center for Surgical Innovation at Johns Hopkins School of Medicine and is a member of the Malone Center for Engineering in Healthcare. He is among the original inventors of cone-beam CT-guided radiotherapy as well as weight-bearing cone-beam CT for musculoskeletal radiology and orthopedic surgery. His work also includes the early development of flat-panel detectors on mobile C-arms for intraoperative cone-beam CT in image-guided surgery. He developed early models for the signal and noise performance of flat-panel detectors and later extended such analysis to dual-energy imaging and 3D imaging performance in cone-beam CT. His core laboratory at Johns Hopkins University is the ISTAR Lab in the Department of Biomedical Engineering at the Johns Hopkins Hospital.
Photon-counting computed tomography (PCCT) is a form of X-ray computed tomography (CT) in which X-rays are detected using a photon-counting detector (PCD) which registers the interactions of individual photons. By keeping track of the deposited energy in each interaction, the detector pixels of a PCD each record an approximate energy spectrum, making it a spectral or energy-resolved CT technique. In contrast, more conventional CT scanners use energy-integrating detectors (EIDs), where the total energy deposited in a pixel during a fixed period of time is registered. These EIDs thus register only photon intensity, comparable to black-and-white photography, whereas PCDs register also spectral information, similar to color photography.
Spectral imaging is an umbrella term for energy-resolved X-ray imaging in medicine. The technique makes use of the energy dependence of X-ray attenuation to either increase the contrast-to-noise ratio, or to provide quantitative image data and reduce image artefacts by so-called material decomposition. Dual-energy imaging, i.e. imaging at two energy levels, is a special case of spectral imaging and is still the most widely used terminology, but the terms "spectral imaging" and "spectral CT" have been coined to acknowledge the fact that photon-counting detectors have the potential for measurements at a larger number of energy levels.
Diffuse optical mammography, or simply optical mammography, is an emerging imaging technique that enables the investigation of the breast composition through spectral analysis. It combines in a single non-invasive tool the capability to implement breast cancer risk assessment, lesion characterization, therapy monitoring and prediction of therapy outcome. It is an application of diffuse optics, which studies light propagation in strongly diffusive media, such as biological tissues, working in the red and near-infrared spectral range, between 600 and 1100 nm.