Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body. MRI does not involve X-rays or the use of ionizing radiation, which distinguishes it from CT and PET scans. MRI is a medical application of nuclear magnetic resonance (NMR). NMR can also be used for imaging in other NMR applications, such as NMR spectroscopy.

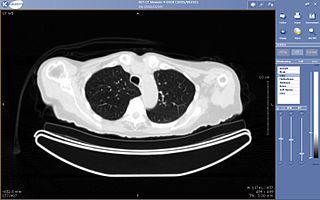
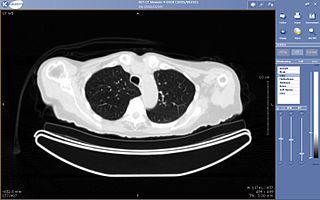
A CT scan, or computed tomography scan is a medical imaging procedure that uses computer-processed combinations of many X-ray measurements taken from different angles to produce cross-sectional (tomographic) images of specific areas of a scanned object, allowing the user to see inside the object without cutting. The 1979 Nobel Prize in Physiology or Medicine was awarded jointly to South African American physicist Allan M. Cormack and British electrical engineer Godfrey N. Hounsfield "for the development of computer assisted tomography."

Radiography is an imaging technique using X-rays, gamma rays, or similar ionizing radiation and non-ionizing radiation to view the internal form of an object. Applications of radiography include medical radiography and industrial radiography. Similar techniques are used in airport security. To create an image in conventional radiography, a beam of X-rays is produced by an X-ray generator and is projected toward the object. A certain amount of the X-rays or other radiation is absorbed by the object, dependent on the object's density and structural composition. The X-rays that pass through the object are captured behind the object by a detector. The generation of flat two dimensional images by this technique is called projectional radiography. In computed tomography an X-ray source and its associated detectors rotate around the subject which itself moves through the conical X-ray beam produced. Any given point within the subject is crossed from many directions by many different beams at different times. Information regarding attenuation of these beams is collated and subjected to computation to generate two dimensional images in three planes which can be further processed to produce a three dimensional image.

Radiology is the medical discipline that uses medical imaging to diagnose and treat diseases within the bodies of animals, including humans.

Medical imaging is the technique and process of creating visual representations of the interior of a body for clinical analysis and medical intervention, as well as visual representation of the function of some organs or tissues (physiology). Medical imaging seeks to reveal internal structures hidden by the skin and bones, as well as to diagnose and treat disease. Medical imaging also establishes a database of normal anatomy and physiology to make it possible to identify abnormalities. Although imaging of removed organs and tissues can be performed for medical reasons, such procedures are usually considered part of pathology instead of medical imaging.

Virtual colonoscopy is a medical imaging procedure which uses x-rays and computers to produce two- and three-dimensional images of the colon from the lowest part, the rectum, all the way to the lower end of the small intestine and display them on a screen. The procedure is used to diagnose colon and bowel disease, including polyps, diverticulosis and colorectal cancer. VC is performed via computed tomography (CT), sometimes called a CAT scan, or with magnetic resonance imaging (MRI). A virtual colonoscopy can provide 3D reconstructed endoluminal views of the bowel. VC provides a secondary benefit of revealing diseases or abnormalities outside the colon.

An arthrogram is a series of images of a joint after injection of a contrast medium, usually done by fluoroscopy or MRI. The injection is normally done under a local anesthetic such as Novocain or lidocaine. The radiologist or radiographer performs the study using fluoroscopy or x-ray to guide the placement of the needle into the joint and then injects around 10 ml of contrast based on age. There is some burning pain from the anesthetic and a painful bubbling feeling in the joint after the contrast is injected. This only lasts 20 - 30 hours until the Contrast is absorbed. During this time, while it is allowed, it is painful to use the limb for around 10 hours. After that the radiologist can more clearly see what is going on under your skin and can get results out within 24 to 48 hours.
Teleradiology is the transmission of radiological patient images, such as x-rays, CTs, and MRIs, from one location to another for the purposes of sharing studies with other radiologists and physicians. Teleradiology is a growth technology given that imaging procedures are growing approximately 15% annually against an increase of only 2% in the radiologist population.
The American College of Radiology (ACR), founded in 1923, is a professional medical society representing nearly 40,000 diagnostic radiologists, radiation oncologists, interventional radiologists, nuclear medicine physicians and medical physicists.
Fee-for-service (FFS) is a payment model where services are unbundled and paid for separately.

Radiographers, also known as radiologic technologists, diagnostic radiographers and medical radiation technologists are healthcare professionals who specialise in the imaging of human anatomy for the diagnosis and treatment of pathology. Radiographers are infrequently, and almost always erroneously, known as x-ray technicians. In countries that use the title radiologic technologist they are often informally referred to as techs in the clinical environment; this phrase has emerged in popular culture such as television programmes. The term radiographer can also refer to a therapeutic radiographer, also known as a radiation therapist.
A full-body scan is a scan of the patient's entire body as part of the diagnosis or treatment of illnesses. If computed tomography (CAT) scan technology is used, it is known as a full-body CT scan, though many medical imaging technologies can perform full-body scans.

CT pulmonary angiogram (CTPA) is a medical diagnostic test that employs computed tomography (CT) angiography to obtain an image of the pulmonary arteries. Its main use is to diagnose pulmonary embolism (PE). It is a preferred choice of imaging in the diagnosis of PE due to its minimally invasive nature for the patient, whose only requirement for the scan is an intravenous line.
In economics, supplier induced demand (SID) may occur when asymmetry of information exists between supplier and consumer. The supplier can use superior information to encourage an individual to demand a greater quantity of the good or service they supply than the Pareto efficient level, should asymmetric information not exist. The result of this is a welfare loss.
Nuclear medicine physicians are medical specialists that use tracers, usually radiopharmaceuticals, for diagnosis and therapy. Nuclear medicine procedures are the major clinical applications of molecular imaging and molecular therapy. In the United States, nuclear medicine physicians are certified by the American Board of Nuclear Medicine and the American Osteopathic Board of Nuclear Medicine.
Paediatric radiology is a subspecialty of radiology involving the imaging of fetuses, infants, children adolescents and young adults. Many paediatric radiologists practice at children's hospitals.
Unnecessary health care is health care provided with a higher volume or cost than is appropriate. In the United States, where health care costs are the highest as a percentage of GDP, overuse was the predominant factor in its expense, accounting for about a third of its health care spending in 2012.
Clinical physiology is both an academic discipline within the medical sciences and a clinical medical specialty for physicians in the health care systems of Sweden, Denmark and Finland. Clinical Physiology can also be more broadly defined as the application of the knowledge of human physiology to patients in a health care setting. As a specialty for medical doctors, Clinical Physiology is a diagnostic specialty to which patients are referred to undergo specialized tests of functions of the heart, blood vessels, lungs, kidneys and gastrointestinal tract, and other organs. Testing methods include evaluation of electrical activity, blood pressure, and air flow. In addition, Clinical Physiologists measure movements, velocities, and metabolic processes through imaging techniques such as ultrasound, echocardiography, magnetic resonance imaging (MRI), x-ray computed tomography (CT), and nuclear medicine scanners.
Global radiology, a subspecialty of diagnostic radiology, comprises the study and practice of improving access to radiology resources in poor and developing countries, and addressing global health inequities through the application of radiology. Similar to the fields of public health and global health, global radiology draws on and encourages collaboration with nonmedical specialties relevant to disease patterns and the provision of medical services, including economic development, biomedical technology, engineering and social sciences.

Magnetic resonance imaging (MRI) is in general a safe technique, although injuries may occur as a result of failed safety procedures or human error. During the last 150 years, thousands of papers focusing on the effects or side effects of magnetic or radiofrequency fields have been published. They can be categorized as incidental and physiological. Contraindications to MRI include most cochlear implants and cardiac pacemakers, shrapnel and metallic foreign bodies in the eyes. The safety of MRI during the first trimester of pregnancy is uncertain, but it may be preferable to other options. Since MRI does not use any ionizing radiation, its use generally is favored in preference to CT when either modality could yield the same information..