Plasmacytoma is a plasma cell dyscrasia in which a plasma cell tumour grows within soft tissue or within the axial skeleton.
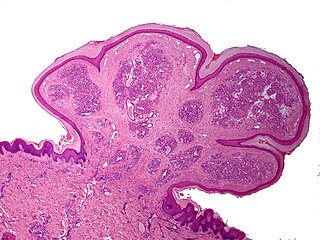
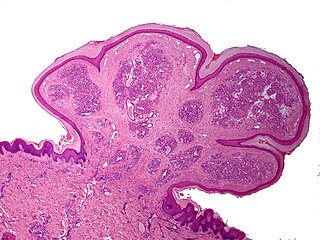
Epulis fissuratum is a benign hyperplasia of fibrous connective tissue which develops as a reactive lesion to chronic mechanical irritation produced by the flange of a poorly fitting denture. More simply, epulis fissuratum is where excess folds of firm tissue form inside the mouth, as a result of rubbing on the edge of dentures that do not fit well. It is a harmless condition and does not represent oral cancer. Treatment is by simple surgical removal of the lesion, and also by adjustment of the denture or provision of a new denture.
A pyogenic granuloma or lobular capillary hemangioma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh.

The immunoglobulin light chain is the small polypeptide subunit of an antibody (immunoglobulin).
A sperm granuloma is a lump of leaked sperm that appears along the vasa deferentia or epididymides in vasectomized individuals. While the majority of sperm granulomas are present along the vas deferens, the rest of them form at the epididymis. Sperm granulomas range in size, from one millimeter to one centimeter. They consist of a central mass of degenerating sperm surrounded by tissue containing blood vessels and immune system cells. Sperm granulomas may also have a yellow, white, or cream colored center when cut open. While some sperm granulomas can be painful, most of them are painless and asymptomatic. Sperm granulomas can appear as a result of surgery, trauma, or an infection. They can appear as early as four days after surgery and fully formed ones can appear as late as 208 days later.
In hematology, plasma cell dyscrasias are a spectrum of progressively more severe monoclonal gammopathies in which a clone or multiple clones of pre-malignant or malignant plasma cells over-produce and secrete into the blood stream a myeloma protein, i.e. an abnormal monoclonal antibody or portion thereof. The exception to this rule is the disorder termed non-secretory multiple myeloma; this disorder is a form of plasma cell dyscrasia in which no myeloma protein is detected in serum or urine of individuals who have clear evidence of an increase in clonal bone marrow plasma cells and/or evidence of clonal plasma cell-mediated tissue injury. Here, a clone of plasma cells refers to group of plasma cells that are abnormal in that they have an identical genetic identity and therefore are descendants of a single genetically distinct ancestor cell.
Fibromatosis colli (FMC), also termed sternocleidomastoid tumor of infancy, pseudotumor of infancy, and infancy sternocleidomastoid pseudotumor, is an uncommon, congenital tumor in one of the two sternocleidomastoid neck muscles although rare cases have presented with a FMC tumor in both sternocleidomastoid muscles. A tumor is here defined as a growth of tissue that is not coordinated with the normal surrounding tissue and persists in growing even if the original trigger for its growth is removed. FMC tumors are benign growths that may cause disfigurements but are not cancers and do not metastasize to distant tissues.
Epulis is any tumor like enlargement situated on the gingival or alveolar mucosa. The word literally means "(growth) on the gingiva", and describes only the location of the mass and has no further implications on the nature of the lesion. There are three types: fibromatous, ossifying and acanthomatous. The related term parulis refers to a mass of inflamed granulation tissue at the opening of a draining sinus on the alveolus over the root of an infected tooth. Another closely related term is gingival enlargement, which tends to be used where the enlargement is more generalized over the whole gingiva rather than a localized mass.

Idiopathic orbital inflammatory (IOI) disease refers to a marginated mass-like enhancing soft tissue involving any area of the orbit. It is the most common painful orbital mass in the adult population, and is associated with proptosis, cranial nerve palsy, uveitis, and retinal detachment. Idiopathic orbital inflammatory syndrome, also known as orbital pseudotumor, was first described by Gleason in 1903 and by Busse and Hochheim. It was then characterized as a distinct entity in 1905 by Birch-Hirschfeld. It is a benign, nongranulomatous orbital inflammatory process characterized by extraocular orbital and adnexal inflammation with no known local or systemic cause. Its diagnosis is of exclusion once neoplasm, primary infection and systemic disorders have been ruled out. Once diagnosed, it is characterized by its chronicity, anatomic location or histologic subtype.

IgG4-related disease (IgG4-RD), formerly known as IgG4-related systemic disease, is a chronic inflammatory condition characterized by tissue infiltration with lymphocytes and IgG4-secreting plasma cells, various degrees of fibrosis (scarring) and a usually prompt response to oral steroids. In approximately 51–70% of people with this disease, serum IgG4 concentrations are elevated during an acute phase.

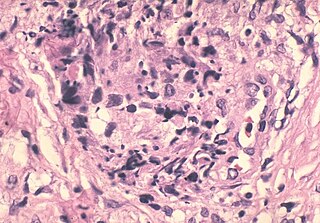
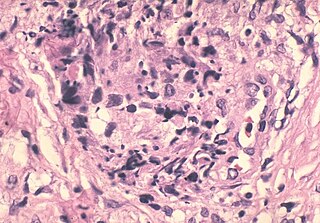
Inflammatory myofibroblastic tumor (IMT) is a rare neoplasm of the mesodermal cells that form the connective tissues which support virtually all of the organs and tissues of the body. IMT was formerly termed inflammatory pseudotumor. Currently, however, inflammatory pseudotumor designates a large and heterogeneous group of soft tissue tumors that includes inflammatory myofibroblastic tumor, plasma cell granuloma, xanthomatous pseudotumor, solitary mast cell granuloma, inflammatory fibrosarcoma, pseudosarcomatous myofibroblastic proliferation, myofibroblastoma, inflammatory myofibrohistiocytic proliferation, and other tumors that develop from connective tissue cells. Inflammatory pseudotumour is a generic term applied to various neoplastic and non-neoplastic tissue lesions which share a common microscopic appearance consisting of spindle cells and a prominent presence of the white blood cells that populate chronic or, less commonly, acute inflamed tissues.
According to the WHO classification, three lesional patterns can be observed

Inflammatory fibroid polyp (IFP) is a benign abnormal growth of tissue projecting into the lumen of the gastrointestinal tract.
The xanthogranulomatous process (XP), is a form of acute and chronic inflammation characterized by an exuberant clustering of foamy macrophages among other inflammatory cells. Localization in the kidney and renal pelvis has been the most frequent and better known occurrence followed by that in the gallbladder but many others have been subsequently recorded. The pathological findings of the process and etiopathogenetic and clinical observations have been reviewed by Cozzutto and Carbone.

An otic polyp is a benign proliferation of chronic inflammatory cells associated with granulation tissue, in response to a longstanding inflammatory process of the middle ear.
Chronic sclerosing sialadenitis is a chronic (long-lasting) inflammatory condition affecting the salivary gland. Relatively rare in occurrence, this condition is benign, but presents as hard, indurated and enlarged masses that are clinically indistinguishable from salivary gland neoplasms or tumors. It is now regarded as a manifestation of IgG4-related disease.
Acral myxoinflammatory fibroblastic sarcoma (AMSF), also termed myxoinflammatory fibroblastic sarcoma (MSF), is a rare, low-grade, soft tissue tumor that the World Health Organization (2020) classified as in the category of rarely metastasizing fibroblastic and myofibroblastic tumors. It is a locally aggressive neoplasm that often recurs at the site of its surgical removal. However, it usually grows slowly and in only 1–2% of cases spreads to distant tissues.

Proliferative fasciitis and proliferative myositis (PF/PM) are rare benign soft tissue lesions that increase in size over several weeks and often regress over the ensuing 1–3 months. The lesions in PF/PM are typically obvious tumors or swellings. Historically, many studies had grouped the two descriptive forms of PF/PM as similar disorders with the exception that proliferative fasciitis occurs in subcutaneous tissues while proliferative myositis occurs in muscle tissues. In 2020, the World Health Organization agreed with this view and defined these lesions as virtually identical disorders termed proliferative fasciitis/proliferative myositis or proliferative fasciitis and proliferative myositis. The Organization also classified them as one of the various forms of the fibroblastic and myofibroblastic tumors.
Fibroblastic and myofibroblastic tumors (FMTs) develop from the mesenchymal stem cells which differentiate into fibroblasts and/or the myocytes/myoblasts that differentiate into muscle cells. FMTs are a heterogeneous group of soft tissue neoplasms. The World Health Organization (2020) defined tumors as being FMTs based on their morphology and, more importantly, newly discovered abnormalities in the expression levels of key gene products made by these tumors' neoplastic cells. Histopathologically, FMTs consist of neoplastic connective tissue cells which have differented into cells that have microscopic appearances resembling fibroblasts and/or myofibroblasts. The fibroblastic cells are characterized as spindle-shaped cells with inconspicuous nucleoli that express vimentin, an intracellular protein typically found in mesenchymal cells, and CD34, a cell surface membrane glycoprotein. Myofibroblastic cells are plumper with more abundant cytoplasm and more prominent nucleoli; they express smooth muscle marker proteins such as smooth muscle actins, desmin, and caldesmon. The World Health Organization further classified FMTs into four tumor forms based on their varying levels of aggressiveness: benign, intermediate, intermediate, and malignant.
Cellular angiofibroma (CAF) is a rare, benign tumor of superficial soft tissues that was first described by M. R. Nucci et al. in 1997. These tumors occur predominantly in the distal parts of the female and male reproductive systems, i.e. in the vulva-vaginal and inguinal-scrotal areas, respectively, or, less commonly, in various other superficial soft tissue areas throughout the body. CAF tumors develop exclusively in adults who typically are more than 30 years old.