A central venous catheter (CVC), also known as a central line (c-line), central venous line, or central venous access catheter, is a catheter placed into a large vein. It is a form of venous access. Placement of larger catheters in more centrally located veins is often needed in critically ill patients, or in those requiring prolonged intravenous therapies, for more reliable vascular access. These catheters are commonly placed in veins in the neck, chest, groin, or through veins in the arms.

Intravenous therapy is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutrients for those who cannot, or will not—due to reduced mental states or otherwise—consume food or water by mouth. It may also be used to administer medications or other medical therapy such as blood products or electrolytes to correct electrolyte imbalances. Attempts at providing intravenous therapy have been recorded as early as the 1400s, but the practice did not become widespread until the 1900s after the development of techniques for safe, effective use.
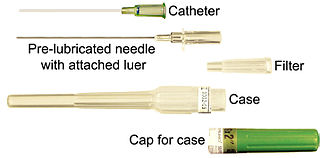
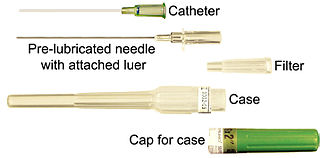
In medicine, a catheter (/ˈkæθətər/) is a thin tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgical procedure. Catheters are manufactured for specific applications, such as cardiovascular, urological, gastrointestinal, neurovascular and ophthalmic procedures. The process of inserting a catheter is called catheterization.
In surgery, a percutaneous procedure is any medical procedure or method where access to inner organs or other tissue is done via needle-puncture of the skin, rather than by using an "open" approach where inner organs or tissue are exposed.

A dialysis catheter is a catheter used for exchanging blood to and from a hemodialysis machine and a patient.

A chest tube is a surgical drain that is inserted through the chest wall and into the pleural space or the mediastinum. The insertion of the tube is sometimes a lifesaving procedure. The tube can be used to remove clinically undesired substances such as air (pneumothorax), excess fluid, blood (hemothorax), chyle (chylothorax) or pus (empyema) from the intrathoracic space. An intrapleural chest tube is also known as a Bülau drain or an intercostal catheter (ICC), and can either be a thin, flexible silicone tube, or a larger, semi-rigid, fenestrated plastic tube, which often involves a flutter valve or underwater seal.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.
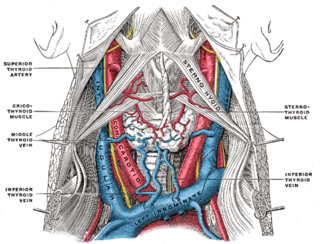
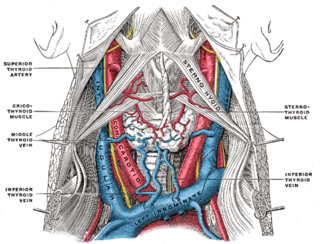
The internal jugular vein is a paired jugular vein that collects blood from the brain and the superficial parts of the face and neck. This vein runs in the carotid sheath with the common carotid artery and vagus nerve.

A peripherally inserted central catheter, less commonly called a percutaneous indwelling central catheter, is a form of intravenous access that can be used for a prolonged period of time or for administration of substances that should not be done peripherally. It is a catheter that enters the body through the skin (percutaneously) at a peripheral site, extends to the superior vena cava, and stays in place for days, weeks or even months.

A Hickman line is a central venous catheter most often used for the administration of chemotherapy or other medications, as well as for the withdrawal of blood for analysis. Some types are used mainly for the purpose of apheresis or dialysis. They have also been used in total parenteral nutrition (TPN). Hickman lines may remain in place for extended periods and are used when long-term intravenous access is required.

The subclavian vein is a paired large vein, one on either side of the body, that is responsible for draining blood from the upper extremities, allowing this blood to return to the heart. The left subclavian vein plays a key role in the absorption of lipids, by allowing products that have been carried by lymph in the thoracic duct to enter the bloodstream. The diameter of the subclavian veins is approximately 1–2 cm, depending on the individual.

The Seldinger technique, also known as Seldinger wire technique, is a medical procedure to obtain moderately safe access to blood vessels and other hollow organs. It is named after Sven Ivar Seldinger (1921–1998), a Swedish radiologist who introduced the procedure in 1953.
Vascular access refers to a rapid, direct method of introducing or removing devices or chemicals from the bloodstream. In hemodialysis, vascular access is used to remove the patient's blood so that it can be filtered through the dialyzer. Three primary methods are used to gain access to the blood: an intravenous catheter, an arteriovenous fistula (AV) or a synthetic graft. In the latter two, needles are used to puncture the graft or fistula each time dialysis is performed.
Obstructive shock is one of the four types of shock, caused by a physical obstruction in the flow of blood. Obstruction can occur at the level of the great vessels or the heart itself. Causes include pulmonary embolism, cardiac tamponade, and tension pneumothorax. These are all life-threatening. Symptoms may include shortness of breath, weakness, or altered mental status. Low blood pressure and tachycardia are often seen in shock. Other symptoms depend on the underlying cause.
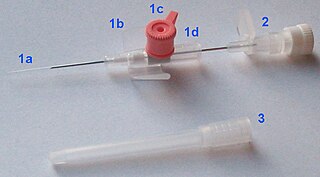
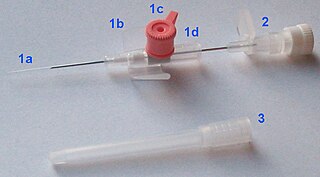
In medicine, a peripheral venous catheter, peripheral venous line, peripheral venous access catheter, or peripheral intravenous catheter, is a catheter placed into a peripheral vein for venous access to administer intravenous therapy such as medication fluids.

Cardiac resynchronisation therapy is the insertion of electrodes in the left and right ventricles of the heart, as well as on occasion the right atrium, to treat heart failure by coordinating the function of the left and right ventricles via a pacemaker, a small device inserted into the anterior chest wall.

A cardiac electrophysiology study is a minimally invasive procedure using catheters introduced through a vein or artery to record electrical activity from within the heart. This electrical activity is recorded when the heart is in a normal rhythm to assess the conduction system of the heart and to look for additional electrical connections, and during any abnormal heart rhythms that can be induced. EP studies are used to investigate the cause, location of origin, and best treatment for various abnormal heart rhythms, and are often followed by a catheter ablation during the same procedure.
Ambesh maneuver is a technique that involves the simple external compression of internal jugular vein in supraclavicular fossa to prevent and diagnose misplacement of the subclavian vein catheter into the internal jugular vein (IJV). The subclavian vein is a big vessel that drains the blood from the hand, forearm and the upper arm into the right side of the heart through superior vena cava. The subclavian veins lie just behind the clavicle on each side and therefore known as subclavian vein.
Venous access is any method used to access the bloodstream through the veins, either to administer intravenous therapy, parenteral nutrition, to obtain blood for analysis, or to provide an access point for blood-based treatments such as dialysis or apheresis. Access is most commonly achieved via the Seldinger technique, and guidance tools such as ultrasound and fluoroscopy can also be used to assist with visualizing access placement.
In medicine, vascular access is a means of accessing the bloodstream through the peripheral or central blood vessels in order to obtain blood or deliver medications including chemotherapy. A vascular access procedure involves insertion of a sterile plastic tube called a catheter into a blood vessel. Types of catheters can be either peripherally or centrally located. Peripheral catheters are approximately one inch (25 mm) long and are inserted into the small veins of the forearm. Central catheters are bigger and longer and are inserted into the large veins of the extremities, neck, or chest. Central venous catheters are the primary modality used for delivery of chemotherapeutic agents. The duration of central venous catheterization is dependent on the type of treatment given.