Related Research Articles

Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.

Pulmonary hypertension is a condition of increased blood pressure in the arteries of the lungs. Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise. Onset is typically gradual. According to the definition at the 6th World Symposium of Pulmonary Hypertension in 2018, a patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 20mmHg at rest, revised down from a purely arbitrary 25mmHg, and pulmonary vascular resistance (PVR) greater than 3 Wood units.
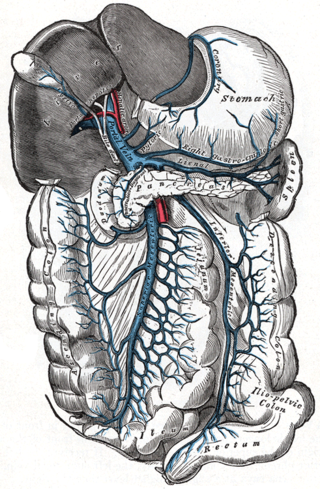
Portal hypertension is abnormally increased portal venous pressure – blood pressure in the portal vein and its branches, that drain from most of the intestine to the liver. Portal hypertension is defined as a hepatic venous pressure gradient greater than 5 mmHg. Cirrhosis is the most common cause of portal hypertension; other, less frequent causes are therefore grouped as non-cirrhotic portal hypertension. When it becomes severe enough to cause symptoms or complications, treatment may be given to decrease portal hypertension itself or to manage its complications.
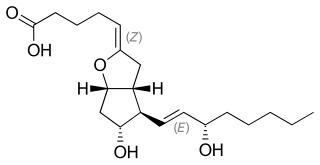
Prostacyclin (also called prostaglandin I2 or PGI2) is a prostaglandin member of the eicosanoid family of lipid molecules. It inhibits platelet activation and is also an effective vasodilator.
In vascular diseases, endothelial dysfunction is a systemic pathological state of the endothelium. Along with acting as a semi-permeable membrane, the endothelium is responsible for maintaining vascular tone and regulating oxidative stress by releasing mediators, such as nitric oxide, prostacyclin and endothelin, and controlling local angiotensin-II activity.

In haemodynamics, the body must respond to physical activities, external temperature, and other factors by homeostatically adjusting its blood flow to deliver nutrients such as oxygen and glucose to stressed tissues and allow them to function. Haemodynamic response (HR) allows the rapid delivery of blood to active neuronal tissues. The brain consumes large amounts of energy but does not have a reservoir of stored energy substrates. Since higher processes in the brain occur almost constantly, cerebral blood flow is essential for the maintenance of neurons, astrocytes, and other cells of the brain. This coupling between neuronal activity and blood flow is also referred to as neurovascular coupling.

Hepatorenal syndrome is a life-threatening medical condition that consists of rapid deterioration in kidney function in individuals with cirrhosis or fulminant liver failure. HRS is usually fatal unless a liver transplant is performed, although various treatments, such as dialysis, can prevent advancement of the condition.
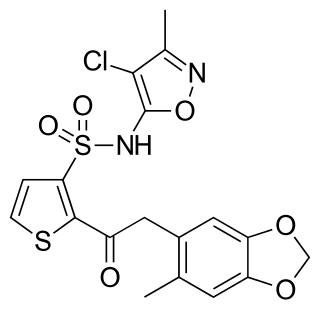
Sitaxentan sodium (TBC-11251) is a medication for the treatment of pulmonary arterial hypertension (PAH). It was marketed as Thelin by Encysive Pharmaceuticals until Pfizer purchased Encysive in February 2008. In 2010, Pfizer voluntarily removed sitaxentan from the market due to concerns about liver toxicity.

Endothelins are peptides with receptors and effects in many body organs. Endothelin constricts blood vessels and raises blood pressure. The endothelins are normally kept in balance by other mechanisms, but when overexpressed, they contribute to high blood pressure (hypertension), heart disease, and potentially other diseases.

Bosentan, sold under the brand name Tracleer and Safebo among others, is a dual endothelin receptor antagonist medication used in the treatment of pulmonary artery hypertension (PAH).

Gastric antral vascular ectasia (GAVE) is an uncommon cause of chronic gastrointestinal bleeding or iron deficiency anemia. The condition is associated with dilated small blood vessels in the pyloric antrum, which is a distal part of the stomach. The dilated vessels result in intestinal bleeding. It is also called watermelon stomach because streaky long red areas that are present in the stomach may resemble the markings on watermelon.

Right ventricular hypertrophy (RVH) is a condition defined by an abnormal enlargement of the cardiac muscle surrounding the right ventricle. The right ventricle is one of the four chambers of the heart. It is located towards the lower-end of the heart and it receives blood from the right atrium and pumps blood into the lungs.

Treprostinil, sold under the brand names Remodulin for infusion, Orenitram for oral, and Tyvaso for inhalation, is a vasodilator that is used for the treatment of pulmonary arterial hypertension. Treprostinil is a synthetic analog of prostacyclin (PGI2).
In medicine, hepatopulmonary syndrome is a syndrome of shortness of breath and hypoxemia caused by vasodilation in the lungs of patients with liver disease. Dyspnea and hypoxemia are worse in the upright position.

The Prostacyclin receptor, also termed the prostaglandin I2 receptor or just IP, is a receptor belonging to the prostaglandin (PG) group of receptors. IP binds to and mediates the biological actions of prostacyclin (also termed Prostaglandin I2, PGI2, or when used as a drug, epoprostenol). IP is encoded in humans by the PTGIR gene. While possessing many functions as defined in animal model studies, the major clinical relevancy of IP is as a powerful vasodilator: stimulators of IP are used to treat severe and even life-threatening diseases involving pathological vasoconstriction.
Persistent fetal circulation is a condition caused by a failure in the systemic circulation and pulmonary circulation to convert from the antenatal circulation pattern to the "normal" pattern. Infants experience a high mean arterial pulmonary artery pressure and a high afterload at the right ventricle. This means that the heart is working against higher pressures, which makes it more difficult for the heart to pump blood.
Nitric oxide is a molecule and chemical compound with chemical formula of NO. In mammals including humans, nitric oxide is a signaling molecule involved in several physiological and pathological processes. It is a powerful vasodilator with a half-life of a few seconds in the blood. Standard pharmaceuticals such as nitroglycerine and amyl nitrite are precursors to nitric oxide. Low levels of nitric oxide production are typically due to ischemic damage in the liver.

Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage to the liver leads to repair of liver tissue and subsequent formation of scar tissue. Over time, scar tissue can replace normal functioning tissue, leading to the impaired liver function of cirrhosis. The disease typically develops slowly over months or years. Early symptoms may include tiredness, weakness, loss of appetite, unexplained weight loss, nausea and vomiting, and discomfort in the right upper quadrant of the abdomen. As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin. The fluid build-up in the abdomen develop spontaneous infections. More serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus, stomach, or intestines, and liver cancer.
Alveolar capillary dysplasia (ACD) is a rare, congenital diffuse lung disease characterized by abnormal blood vessels in the lungs that cause highly elevated pulmonary blood pressure and an inability to effectively oxygenate and remove carbon dioxide from the blood. ACD typically presents in newborn babies within hours of birth as rapid and labored breathing, blue-colored lips or skin, quickly leading to respiratory failure and death. Atypical forms of ACD have been reported with initially milder symptoms and survival of many months before the onset of respiratory failure or lung transplantation.

Pulmonary veno-occlusive disease (PVOD) is a rare form of pulmonary hypertension caused by progressive blockage of the small veins in the lungs. The blockage leads to high blood pressures in the arteries of the lungs, which, in turn, leads to heart failure. The disease is progressive and fatal, with median survival of about 2 years from the time of diagnosis to death. The definitive therapy is lung transplantation.
References
- ↑ Adapted from: Tapper EB: http://wikidoc.org/index.php/Portopulmonary_hypertension
- ↑ Kuo, PC; Plotkin, JS; Gaine, S; Schroeder, RA; Rustgi, VK; Rubin, LJ; Johnson, LB (27 April 1999). "Portopulmonary hypertension and the liver transplant candidate". Transplantation. 67 (8): 1087–93. doi:10.1097/00007890-199904270-00001. PMID 10232556.
- 1 2 Torregrosa, M; Genesca, J; Gonzalez, A; Evangelista, A; Mora, A; Margarit, C; Esteban, R; Guardia, J (27 February 2001). "Role of Doppler echocardiography in the assessment of portopulmonary hypertension in liver transplantation candidates". Transplantation. 71 (4): 572–4. doi: 10.1097/00007890-200102270-00015 . PMID 11258439. S2CID 42061691.
- 1 2 3 4 Tapper, EB; Knowles, D; Heffron, T; Lawrence, EC; Csete, M (June 2009). "Portopulmonary hypertension: imatinib as a novel treatment and the Emory experience with this condition". Transplantation Proceedings. 41 (5): 1969–71. doi:10.1016/j.transproceed.2009.02.100. PMID 19545770.
- 1 2 3 Le Pavec et al. Portopulmonary Hypertension: Survival and Prognostic Factors. Am J Respir Crit Care Med Vol 178. pp 637–643, 2008
- 1 2 Kawut, SM; Krowka, MJ; Trotter, JF; Roberts, KE; Benza, RL; Badesch, DB; Taichman, DB; Horn, EM; Zacks, S; Kaplowitz, N; Brown RS, Jr; Fallon, MB; Pulmonary Vascular Complications of Liver Disease Study, Group. (July 2008). "Clinical risk factors for portopulmonary hypertension". Hepatology. 48 (1): 196–203. doi:10.1002/hep.22275. PMC 2824885 . PMID 18537192.
- 1 2 Benjaminov, FS; Prentice, M; Sniderman, KW; Siu, S; Liu, P; Wong, F (September 2003). "Portopulmonary hypertension in decompensated cirrhosis with refractory ascites". Gut. 52 (9): 1355–62. doi:10.1136/gut.52.9.1355. PMC 1773797 . PMID 12912870.
- 1 2 Hadengue, A; Benhayoun, MK; Lebrec, D; Benhamou, JP (February 1991). "Pulmonary hypertension complicating portal hypertension: prevalence and relation to splanchnic hemodynamics". Gastroenterology. 100 (2): 520–8. doi:10.1016/0016-5085(91)90225-a. PMID 1985048.
- ↑ Martínez-Palli, G; Taurà, P; Balust, J; Beltrán, J; Zavala, E; Garcia-Valdecasas, JC (November 2005). "Liver transplantation in high-risk patients: hepatopulmonary syndrome and portopulmonary hypertension". Transplantation Proceedings. 37 (9): 3861–4. doi:10.1016/j.transproceed.2005.09.119. PMID 16386564.
- ↑ Budhiraja, R; Hassoun, PM (February 2003). "Portopulmonary hypertension: a tale of two circulations". Chest. 123 (2): 562–76. doi:10.1378/chest.123.2.562. PMID 12576381.
- ↑ Moller, S; Henriksen, JH (28 January 2006). "Cardiopulmonary complications in chronic liver disease". World Journal of Gastroenterology. 12 (4): 526–38. doi: 10.3748/wjg.v12.i4.526 . PMC 4066083 . PMID 16489664.
- ↑ Christman, BW; McPherson, CD; Newman, JH; King, GA; Bernard, GR; Groves, BM; Loyd, JE (9 July 1992). "An imbalance between the excretion of thromboxane and prostacyclin metabolites in pulmonary hypertension". The New England Journal of Medicine. 327 (2): 70–5. doi:10.1056/NEJM199207093270202. PMID 1603138.
- ↑ Maruyama, T; Ohsaki, K; Shimoda, S; Kaji, Y; Harada, M (January 2005). "Thromboxane-dependent portopulmonary hypertension". The American Journal of Medicine. 118 (1): 93–4. doi:10.1016/j.amjmed.2004.11.007. PMID 15639216.
- ↑ Giaid, A (September 1998). "Nitric oxide and endothelin-1 in pulmonary hypertension". Chest. 114 (3 Suppl): 208S–212S. doi:10.1378/chest.114.3_supplement.208s. PMID 9741571.
- ↑ Gerbes, AL; Møller, S; Gülberg, V; Henriksen, JH (March 1995). "Endothelin-1 and -3 plasma concentrations in patients with cirrhosis: role of splanchnic and renal passage and liver function". Hepatology. 21 (3): 735–9. PMID 7875671.
- ↑ Stewart, DJ; Levy, RD; Cernacek, P; Langleben, D (15 March 1991). "Increased plasma endothelin-1 in pulmonary hypertension: marker or mediator of disease?". Annals of Internal Medicine. 114 (6): 464–9. doi:10.7326/0003-4819-114-6-464. PMID 1994793.
- ↑ Luo, B; Liu, L; Tang, L; Zhang, J; Stockard, CR; Grizzle, WE; Fallon, MB (May 2003). "Increased pulmonary vascular endothelin B receptor expression and responsiveness to endothelin-1 in cirrhotic and portal hypertensive rats: a potential mechanism in experimental hepatopulmonary syndrome". Journal of Hepatology. 38 (5): 556–63. doi:10.1016/s0168-8278(03)00012-6. PMID 12713865.
- ↑ Egermayer, P; Town, GI; Peacock, AJ (February 1999). "Role of serotonin in the pathogenesis of acute and chronic pulmonary hypertension". Thorax. 54 (2): 161–8. doi:10.1136/thx.54.2.161. PMC 1745408 . PMID 10325923.
- ↑ Schraufnagel DE, Kay JM. Structural and pathologic changes in lung vasculature in chronic liver disease. Clin Chest Med 1996; 17: 1
- ↑ Matsubara, O; Nakamura, T; Uehara, T; Kasuga, T (May 1984). "Histometrical investigation of the pulmonary artery in severe hepatic disease". The Journal of Pathology. 143 (1): 31–7. doi:10.1002/path.1711430106. PMID 6737114. S2CID 25097088.
- 1 2 Swanson, KL; Wiesner, RH; Nyberg, SL; Rosen, CB; Krowka, MJ (November 2008). "Survival in portopulmonary hypertension: Mayo Clinic experience categorized by treatment subgroups". American Journal of Transplantation. 8 (11): 2445–53. doi:10.1111/j.1600-6143.2008.02384.x. PMID 18782292. S2CID 25269798.
- 1 2 Kim et al. Accuracy of Doppler Echos in the assessment of PTHN in liver transplant candidates. Liver Transplant. 6:453, 2000
- ↑ Colle, IO; Moreau, R; Godinho, E; Belghiti, J; Ettori, F; Cohen-Solal, A; Mal, H; Bernuau, J; Marty, J; Lebrec, D; Valla, D; Durand, F (February 2003). "Diagnosis of portopulmonary hypertension in candidates for liver transplantation: a prospective study". Hepatology. 37 (2): 401–9. doi:10.1053/jhep.2003.50060. PMID 12540791. S2CID 38503767.
- ↑ Tapper EB, unpublished data
- ↑ Swanson KL, Krowka MJ (2006). "Chapter 9 - Portopulmonary Hypertension". Pulmonary Vascular Disease: 132–142. doi:10.1016/B978-1-4160-2246-6.50015-8. ISBN 9781416022466 . Retrieved 11 August 2021.
- ↑ Steudel, W; Hurford, WE; Zapol, WM (October 1999). "Inhaled nitric oxide: basic biology and clinical applications". Anesthesiology. 91 (4): 1090–121. doi:10.1097/00000542-199910000-00030. PMID 10519513.
- ↑ Lowson. Inhaled alternative to nitric oxide. Anesthesiology 2002;96:1504-13
- ↑ "Methemoglobinemia". The Lecturio Medical Concept Library. Retrieved 11 August 2021.
- ↑ Kerins et al. Prostacyclin and Prostaglandin E1: Molecular mechanisms and therapeutic utility. Prog Hemostasis Thrombosis 1991;10:307-37
- ↑ Vane et al. Pharmacodynamic profile of prostacyclin. Am J Cardiol 1995;75:3A-10A
- ↑ Eichelbrönner, O; Reinelt, H; Wiedeck, H; Mezödy, M; Rossaint, R; Georgieff, M; Radermacher, P (September 1996). "Aerosolized prostacyclin and inhaled nitric oxide in septic shock--different effects on splanchnic oxygenation?". Intensive Care Medicine. 22 (9): 880–7. doi:10.1007/BF02044111. PMID 8905421. S2CID 8567462.
- ↑ Minder, S; Fischler, M; Muellhaupt, B; Zalunardo, MP; Jenni, R; Clavien, PA; Speich, R (October 2004). "Intravenous iloprost bridging to orthotopic liver transplantation in portopulmonary hypertension". The European Respiratory Journal. 24 (4): 703–7. doi: 10.1183/09031936.04.00133203 . PMID 15459152. S2CID 8665441.
- ↑ et al. Successful use of chronic epoprostenol as a bridge to liver transplant in severe PPHTN. Transplant 1998 4:457
- ↑ Kuo PC, Johnson LB, Plotkin JS, Howell CD, Bartlett ST, Rubin LJ. Continuous intravenous infusion of epoprostenol for the treatment of portopulmonary hypertension. Transplantation 1997; 63: 604
- ↑ Lowson, SM (March 2005). "Inhaled alternatives to nitric oxide". Critical Care Medicine. 33 (3 Suppl): S188-95. doi:10.1097/01.ccm.0000156792.40298.5a. PMID 15753727. S2CID 3103356.
- ↑ Makisalo, H; Koivusalo, A; Vakkuri, A; Hockerstedt, K (July 2004). "Sildenafil for portopulmonary hypertension in a patient undergoing liver transplantation". Liver Transplantation. 10 (7): 945–50. doi: 10.1002/lt.20153 . PMID 15237383. S2CID 43228732.
- ↑ Berkels, R; Klotz, T; Sticht, G; Englemann, U; Klaus, W (April 2001). "Modulation of human platelet aggregation by the phosphodiesterase type 5 inhibitor sildenafil". Journal of Cardiovascular Pharmacology. 37 (4): 413–21. doi:10.1097/00005344-200104000-00008. PMID 11300654. S2CID 38632760.
- ↑ Haraldsson et al. The additive pulmonary vasodilatory effect of inhaled prostacyclin and inhaled milrinone in postcardiac surgical patients with pulmonary hypertension. Aesth Analg 2001;93:1439-45
- ↑ Rubin, LJ; Badesch, DB; Barst, RJ; Galie, N; Black, CM; Keogh, A; Pulido, T; Frost, A; Roux, S; Leconte, I; Landzberg, M; Simonneau, G (21 March 2002). "Bosentan therapy for pulmonary arterial hypertension". The New England Journal of Medicine. 346 (12): 896–903. doi: 10.1056/NEJMoa012212 . PMID 11907289.
- ↑ Hoeper, MM; Halank, M; Marx, C; Hoeffken, G; Seyfarth, HJ; Schauer, J; Niedermeyer, J; Winkler, J (March 2005). "Bosentan therapy for portopulmonary hypertension". The European Respiratory Journal. 25 (3): 502–8. doi: 10.1183/09031936.05.00080804 . PMID 15738295. S2CID 14416325.
- ↑ Kuntzen, C; Gülberg, V; Gerbes, AL (January 2005). "Use of a mixed endothelin receptor antagonist in portopulmonary hypertension: a safe and effective therapy?". Gastroenterology. 128 (1): 164–8. doi: 10.1053/j.gastro.2004.09.005 . PMID 15633133.
- ↑ Wilkins, MR; Paul, GA; Strange, JW; Tunariu, N; Gin-Sing, W; Banya, WA; Westwood, MA; Stefanidis, A; Ng, LL; Pennell, DJ; Mohiaddin, RH; Nihoyannopoulos, P; Gibbs, JS (1 June 2005). "Sildenafil versus Endothelin Receptor Antagonist for Pulmonary Hypertension (SERAPH) study". American Journal of Respiratory and Critical Care Medicine. 171 (11): 1292–7. doi:10.1164/rccm.200410-1411OC. PMID 15750042.
- ↑ Schermuly, RT; Dony, E; Ghofrani, HA; Pullamsetti, S; Savai, R; Roth, M; Sydykov, A; Lai, YJ; Weissmann, N; Seeger, W; Grimminger, F (October 2005). "Reversal of experimental pulmonary hypertension by PDGF inhibition". The Journal of Clinical Investigation. 115 (10): 2811–21. doi:10.1172/JCI24838. PMC 1236676 . PMID 16200212.
- ↑ Ghofrani, HA; Seeger, W; Grimminger, F (29 September 2005). "Imatinib for the treatment of pulmonary arterial hypertension". The New England Journal of Medicine. 353 (13): 1412–3. doi:10.1056/NEJMc051946. PMID 16192491.
- ↑ Ramsay, MA; Simpson, BR; Nguyen, AT; Ramsay, KJ; East, C; Klintmalm, GB (September 1997). "Severe pulmonary hypertension in liver transplant candidates". Liver Transplantation and Surgery. 3 (5): 494–500. doi: 10.1002/lt.500030503 . PMID 9346791.
- ↑ Csete, M (July 1997). "Intraoperative management of liver transplant patients with pulmonary hypertension". Liver Transplantation and Surgery. 3 (4): 454–5. doi:10.1002/lt.500030422. PMID 9346782.
- ↑ Krowka, MJ; Plevak, DJ; Findlay, JY; Rosen, CB; Wiesner, RH; Krom, RA (July 2000). "Pulmonary hemodynamics and perioperative cardiopulmonary-related mortality in patients with portopulmonary hypertension undergoing liver transplantation". Liver Transplantation. 6 (4): 443–50. doi:10.1053/jlts.2000.6356. PMID 10915166. S2CID 25182926.