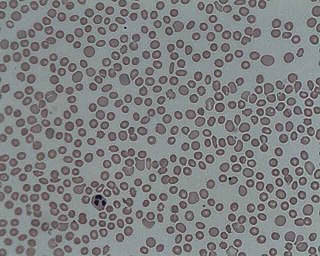
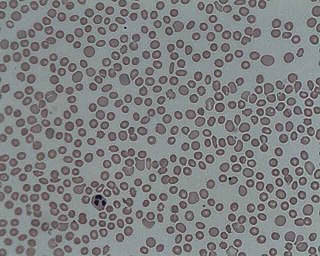
Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, platelets, and other clotting factors.

Platelets or thrombocytes are a component of blood whose function is to react to bleeding from blood vessel injury by clumping, thereby initiating a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm derived from the megakaryocytes of the bone marrow or lung, which then enter the circulation. Platelets are found only in mammals, whereas in other vertebrates, thrombocytes circulate as intact mononuclear cells.

Immune thrombocytopenic purpura (ITP), also known as idiopathic thrombocytopenic purpura or immune thrombocytopenia, is a type of thrombocytopenic purpura characterized by a low platelet count in the absence of other causes, and accompanied by a red-purple rash called purpura. It leads to an increased risk of bleeding. ITP manifests in two distinct clinical syndromes: an acute form observed in children, and chronic conditions observed in adults. The acute form often follows an infection and typically resolves within two months, while chronic immune thrombocytopenia persists for longer than six months and its specific cause is unknown.

Thrombotic thrombocytopenic purpura (TTP) is a blood disorder that results in blood clots forming in small blood vessels throughout the body. This results in a low platelet count, low red blood cells due to their breakdown, and often kidney, heart, and brain dysfunction. Symptoms may include large bruises, fever, weakness, shortness of breath, confusion, and headache. Repeated episodes may occur.

A blood donation occurs when a person voluntarily has blood drawn and used for transfusions and/or made into biopharmaceutical medications by a process called fractionation. Donation may be of whole blood, or of specific components directly (apheresis). Blood banks often participate in the collection process as well as the procedures that follow it.
In hematology, thrombocytopenia is a condition characterized by abnormally low levels of platelets in the blood. Low levels of platelets in turn may lead to prolonged or excessive bleeding. It is the most common coagulation disorder among intensive care patients and is seen in a fifth of medical patients and a third of surgical patients.

Plateletpheresis is the process of collecting thrombocytes, more commonly called platelets, a component of blood involved in blood clotting. The term specifically refers to the method of collecting the platelets, which is performed by a device used in blood donation that separates the platelets and returns other portions of the blood to the donor. Platelet transfusion can be a life-saving procedure in preventing or treating serious complications from bleeding and hemorrhage in patients who have disorders manifesting as thrombocytopenia or platelet dysfunction. This process may also be used therapeutically to treat disorders resulting in extraordinarily high platelet counts such as essential thrombocytosis.

Transfusion-related acute lung injury (TRALI) is the serious complication of transfusion of blood products that is characterized by the rapid onset of excess fluid in the lungs. It can cause dangerous drops in the supply of oxygen to body tissues. Although changes in transfusion practices have reduced the incidence of TRALI, it was the leading cause of transfusion-related deaths in the United States from fiscal year 2008 through fiscal year 2012.

Platelet transfusion, also known as platelet concentrate, is used to prevent or treat bleeding in people with either a low platelet count or poor platelet function. Often this occurs in people receiving cancer chemotherapy. Preventive transfusion is often done in those with platelet levels of less than 10 x 109/L. In those who are bleeding transfusion is usually carried out at less than 50 x 109/L. Blood group matching (ABO, RhD) is typically recommended before platelets are given. Unmatched platelets, however, are often used due to the unavailability of matched platelets. They are given by injection into a vein.
Hemolytic disease of the newborn (anti-Rhc) can range from a mild to a severe disease. It is the third most common cause of severe HDN. Rh disease is the most common and hemolytic disease of the newborn (anti-Kell) is the second most common cause of severe HDN. It occurs more commonly in women who are Rh D negative.
Transfusion-associated graft-versus-host disease (TA-GvHD) is a rare complication of blood transfusion, in which the immunologically competent donor T lymphocytes mount an immune response against the recipient's lymphoid tissue. These donor lymphocytes engraft, recognize recipient cells as foreign and mount an immune response against recipient tissues. Donor lymphocytes are usually identified as foreign and destroyed by the recipient's immune system. However, in situations where the recipient is severely immunocompromised, or when the donor and recipient HLA type is similar, the recipient's immune system is not able to destroy the donor lymphocytes. This can result in transfusion associated graft-versus-host disease. This is in contrast with organ/tissue transplant associated GvHD, where matching HLA reduces the incident of the complication.
Neonatal alloimmune thrombocytopenia is a disease that affects babies in which the platelet count is decreased because the mother's immune system attacks her fetus' or newborn's platelets. A low platelet count increases the risk of bleeding in the fetus and newborn. If the bleeding occurs in the brain, there may be long-term effects.
Human platelet antigens (HPA) are polymorphisms in platelet antigens. These can stimulate production of alloantibodies (that is, antibodies against other people's antigens) in recipients of transfused platelets from donors with different HPAs. These antibodies cause neonatal alloimmune thrombocytopenia, post-transfusion purpura, and some cases of platelet transfusion refractoriness to infusion of donor platelets.

Neonatal isoerythrolysis (NI), also known as hemolytic icterus or hemolytic anemia, is a disease most commonly seen in kittens and foals, but has also been reported in puppies. It occurs when the mother has antibodies against the blood type of the newborn.
Hemolytic disease of the newborn (anti-RhE) is caused by the anti-RhE antibody of the Rh blood group system. The anti-RhE antibody can be naturally occurring, or arise following immune sensitization after a blood transfusion or pregnancy.
Platelet transfusion refractoriness is the repeated failure to achieve the desired level of blood platelets in a patient following a platelet transfusion. The cause of refractoriness may be either immune or non-immune. Among immune-related refractoriness, antibodies against HLA antigens are the primary cause. Non-immune causes include splenomegaly, fever, and sepsis.
This page is currently under construction.

Blood compatibility testing is conducted in a medical laboratory to identify potential incompatibilities between blood group systems in blood transfusion. It is also used to diagnose and prevent some complications of pregnancy that can occur when the baby has a different blood group from the mother. Blood compatibility testing includes blood typing, which detects the antigens on red blood cells that determine a person's blood type; testing for unexpected antibodies against blood group antigens ; and, in the case of blood transfusions, mixing the recipient's plasma with the donor's red blood cells to detect incompatibilities (crossmatching). Routine blood typing involves determining the ABO and RhD type, and involves both identification of ABO antigens on red blood cells and identification of ABO antibodies in the plasma. Other blood group antigens may be tested for in specific clinical situations.
A granulocyte transfusion is a medical procedure in which granulocytes are infused into a person's blood. Granulocyte transfusions were historically used to prevent and treat infections in people with neutropenia, but the practice declined in popularity in the 1980s. Interest in the procedure increased in the 1990s due to the development of more effective methods for harvesting granulocytes and a growing population of people with severe neutropenia from chemotherapy. However, the treatment's efficacy remains poorly understood and its use is controversial.

The monocyte monolayer assay (MMA) is used to determine the clinical significance of alloantibodies produced by blood transfusion recipients. The assay is used to assess the potential for intravascular hemolysis when incompatible cellular blood products are transfused to the anemic patient. When donor cells possess substances that are not produced by the recipient, the recipient's immune system produces antibodies against the substance; these are called alloantibodies. Specific white blood cells, called monocytes, are tasked with ingesting foreign material and become activated during certain inflammatory events. These activated monocytes come in contact with antibody-sensitized red blood cells (RBC) and may or may not exhibit phagocytosis (ingestion) and destroy the donor red blood cells. If monocytes destroy the RBC, the antibody attached to those RBC is considered clinically significant.