Related Research Articles

A head injury is any injury that results in trauma to the skull or brain. The terms traumatic brain injury and head injury are often used interchangeably in the medical literature. Because head injuries cover such a broad scope of injuries, there are many causes—including accidents, falls, physical assault, or traffic accidents—that can cause head injuries.

Neurotrauma, brain damage or brain injury (BI) is the destruction or degeneration of brain cells. Brain injuries occur due to a wide range of internal and external factors. In general, brain damage refers to significant, undiscriminating trauma-induced damage.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, coma and death.

A concussion, also known as a mild traumatic brain injury (mTBI), is a head injury that temporarily affects brain functioning. Symptoms may include loss of consciousness (LOC); memory loss; headaches; difficulty with thinking, concentration, or balance; nausea; blurred vision; sleep disturbances, and mood changes. Any of these symptoms may begin immediately, or appear days after the injury. Concussion should be suspected if a person indirectly or directly hits their head and experiences any of the symptoms of concussion. It is not unusual for symptoms to last 2 weeks in adults and 4 weeks in children. Fewer than 10% of sports-related concussions among children are associated with loss of consciousness.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.
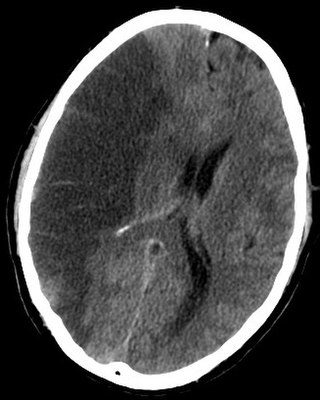
A traumatic brain injury (TBI), also known as an intracranial injury, is an injury to the brain caused by an external force. TBI can be classified based on severity, mechanism, or other features. Head injury is a broader category that may involve damage to other structures such as the scalp and skull. TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.
A penetrating head injury, or open head injury, is a head injury in which the dura mater, the outer layer of the meninges, is breached. Penetrating injury can be caused by high-velocity projectiles or objects of lower velocity such as knives, or bone fragments from a skull fracture that are driven into the brain. Head injuries caused by penetrating trauma are serious medical emergencies and may cause permanent disability or death.
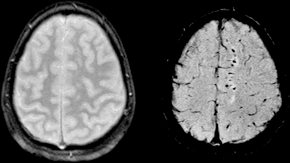
Diffuse axonal injury (DAI) is a brain injury in which scattered lesions occur over a widespread area in white matter tracts as well as grey matter. DAI is one of the most common and devastating types of traumatic brain injury and is a major cause of unconsciousness and persistent vegetative state after severe head trauma. It occurs in about half of all cases of severe head trauma and may be the primary damage that occurs in concussion. The outcome is frequently coma, with over 90% of patients with severe DAI never regaining consciousness. Those who awaken from the coma often remain significantly impaired.

Astrogliosis is an abnormal increase in the number of astrocytes due to the destruction of nearby neurons from central nervous system (CNS) trauma, infection, ischemia, stroke, autoimmune responses or neurodegenerative disease. In healthy neural tissue, astrocytes play critical roles in energy provision, regulation of blood flow, homeostasis of extracellular fluid, homeostasis of ions and transmitters, regulation of synapse function and synaptic remodeling. Astrogliosis changes the molecular expression and morphology of astrocytes, in response to infection for example, in severe cases causing glial scar formation that may inhibit axon regeneration.
An induced coma – also known as a medically induced coma (MIC), barbiturate-induced coma, or drug-induced coma – is a temporary coma brought on by a controlled dose of an anesthetic drug, often a barbiturate such as pentobarbital or thiopental. Other intravenous anesthetic drugs such as midazolam or propofol may be used.

Cerebral hypoxia is a form of hypoxia, specifically involving the brain; when the brain is completely deprived of oxygen, it is called cerebral anoxia. There are four categories of cerebral hypoxia; they are, in order of increasing severity: diffuse cerebral hypoxia (DCH), focal cerebral ischemia, cerebral infarction, and global cerebral ischemia. Prolonged hypoxia induces neuronal cell death via apoptosis, resulting in a hypoxic brain injury.
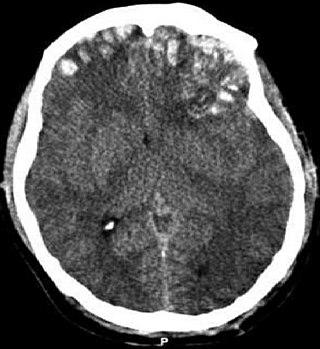
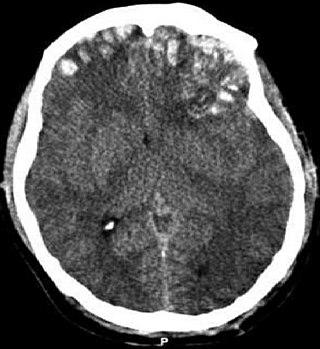
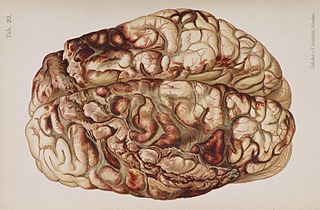
Cerebral contusion, Latin contusio cerebri, a form of traumatic brain injury, is a bruise of the brain tissue. Like bruises in other tissues, cerebral contusion can be associated with multiple microhemorrhages, small blood vessel leaks into brain tissue. Contusion occurs in 20–30% of severe head injuries. A cerebral laceration is a similar injury except that, according to their respective definitions, the pia-arachnoid membranes are torn over the site of injury in laceration and are not torn in contusion. The injury can cause a decline in mental function in the long term and in the emergency setting may result in brain herniation, a life-threatening condition in which parts of the brain are squeezed past parts of the skull. Thus treatment aims to prevent dangerous rises in intracranial pressure, the pressure within the skull.
Brain ischemia is a condition in which there is insufficient bloodflow to the brain to meet metabolic demand. This leads to poor oxygen supply or cerebral hypoxia and thus leads to the death of brain tissue or cerebral infarction/ischemic stroke. It is a sub-type of stroke along with subarachnoid hemorrhage and intracerebral hemorrhage.

Osmotherapy is the use of osmotically active substances to reduce the volume of intracranial contents. Osmotherapy serves as the primary medical treatment for cerebral edema. The primary purpose of osmotherapy is to improve elasticity and decrease intracranial volume by removing free water, accumulated as a result of cerebral edema, from brain's extracellular and intracellular space into vascular compartment by creating an osmotic gradient between the blood and brain. Normal serum osmolality ranges from 280 to 290 mOsm/kg and serum osmolality to cause water removal from brain without much side effects ranges from 300 to 320 mOsm/kg. Usually, 90 mL of space is created in the intracranial vault by 1.6% reduction in brain water content. Osmotherapy has cerebral dehydrating effects. The main goal of osmotherapy is to decrease intracranial pressure (ICP) by shifting excess fluid from brain. This is accomplished by intravenous administration of osmotic agents which increase serum osmolality in order to shift excess fluid from intracellular or extracellular space of the brain to intravascular compartment. The resulting brain shrinkage effectively reduces intracranial volume and decreases ICP.
Post-traumatic epilepsy (PTE) is a form of acquired epilepsy that results from brain damage caused by physical trauma to the brain. A person with PTE experiences repeated post-traumatic seizures more than a week after the initial injury. PTE is estimated to constitute 5% of all cases of epilepsy and over 20% of cases of acquired epilepsy.
Post-traumatic seizures (PTS) are seizures that result from traumatic brain injury (TBI), brain damage caused by physical trauma. PTS may be a risk factor for post-traumatic epilepsy (PTE), but a person having a seizure or seizures due to traumatic brain injury does not necessarily have PTE, which is a form of epilepsy, a chronic condition in which seizures occur repeatedly. However, "PTS" and "PTE" may be used interchangeably in medical literature.

Focal and diffuse brain injury are ways to classify brain injury: focal injury occurs in a specific location, while diffuse injury occurs over a more widespread area. It is common for both focal and diffuse damage to occur as a result of the same event; many traumatic brain injuries have aspects of both focal and diffuse injury. Focal injuries are commonly associated with an injury in which the head strikes or is struck by an object; diffuse injuries are more often found in acceleration/deceleration injuries, in which the head does not necessarily contact anything, but brain tissue is damaged because tissue types with varying densities accelerate at different rates. In addition to physical trauma, other types of brain injury, such as stroke, can also produce focal and diffuse injuries. There may be primary and secondary brain injury processes.
Traumatic brain injury can cause a variety of complications, health effects that are not TBI themselves but that result from it. The risk of complications increases with the severity of the trauma; however even mild traumatic brain injury can result in disabilities that interfere with social interactions, employment, and everyday living. TBI can cause a variety of problems including physical, cognitive, emotional, and behavioral complications.

Ulegyria is a diagnosis used to describe a specific type of cortical scarring in the deep regions of the sulcus that leads to distortion of the gyri. Ulegyria is identified by its characteristic "mushroom-shaped" gyri, in which scarring causes shrinkage and atrophy in the deep sulcal regions while the surface gyri are spared. This condition is most often caused by hypoxic-ischemic brain injury in the perinatal period. The effects of ulegyria can range in severity, although it is most commonly associated with cerebral palsy, mental retardation and epilepsy. N.C. Bresler was the first to view ulegyria in 1899 and described this abnormal morphology in the brain as “mushroom-gyri." Although ulegyria was first identified in 1899, there is still limited information known or reported about the condition.
Sleep disorder is a common repercussion of traumatic brain injury (TBI). It occurs in 30%-70% of patients with TBI. TBI can be distinguished into two categories, primary and secondary damage. Primary damage includes injuries of white matter, focal contusion, cerebral edema and hematomas, mostly occurring at the moment of the trauma. Secondary damage involves the damage of neurotransmitter release, inflammatory responses, mitochondrial dysfunctions and gene activation, occurring minutes to days following the trauma. Patients with sleeping disorders following TBI specifically develop insomnia, sleep apnea, narcolepsy, periodic limb movement disorder and hypersomnia. Furthermore, circadian sleep-wake disorders can occur after TBI.
References
- 1 2 3 4 5 6 Scalea TM (2005). "Does it matter how head injured patients are resuscitated?". In Valadka AB, Andrews BT (eds.). Neurotrauma: Evidence-Based Answers To Common Questions. Thieme. pp. 3–4. ISBN 3-13-130781-1.
- ↑ Ortega-Pérez, Stefany; Amaya-Rey, Maria (2018). "Secondary Brain Injury: A Concept Analysis". Journal of Neuroscience Nursing. 50 (4): 220–224. doi:10.1097/JNN.0000000000000384. PMID 29985274. S2CID 51602244.
- 1 2 3 Gennarelli GA, Graham DI (2005). "Neuropathology". In Silver JM, McAllister TW, Yudofsky SC (eds.). Textbook Of Traumatic Brain Injury. Washington, DC: American Psychiatric Association. pp. 27–33. ISBN 1-58562-105-6 . Retrieved 2008-06-10.
- ↑ Granacher RP (2007). Traumatic Brain Injury: Methods for Clinical & Forensic Neuropsychiatric Assessment, Second Edition. Boca Raton: CRC. pp. 26–32. ISBN 978-0-8493-8138-6 . Retrieved 2008-07-06.
- 1 2 3 Hammeke TA, Gennarelli TA (2003). "Traumatic brain injury". In Schiffer RB, Rao SM, Fogel BS (eds.). Neuropsychiatry. Hagerstown, MD: Lippincott Williams & Wilkins. p. 1150. ISBN 0-7817-2655-7 . Retrieved 2008-06-16.
- 1 2 Porth, Carol (2007). Essentials of Pahtophysiology: Concepts of Altered Health States. Hagerstown, MD: Lippincott Williams & Wilkins. p. 838. ISBN 978-0-7817-7087-3 . Retrieved 2008-07-03.
- ↑ Pitkänen A, McIntosh TK (2006). "Animal models of post-traumatic epilepsy". Journal of Neurotrauma. 23 (2): 241–261. doi:10.1089/neu.2006.23.241. PMID 16503807.
- 1 2 3 4 5 LaPlaca MC, Simon CM, Prado GR, Cullen DR (2007). "CNS injury biomechanics and experimental models". In Weber JT (ed.). Neurotrauma: New Insights Into Pathology and Treatment. Elsevier. pp. 13–19. ISBN 978-0-444-53017-2 . Retrieved 2008-06-10.
- 1 2 Granacher RP (2007). Traumatic Brain Injury: Methods for Clinical & Forensic Neuropsychiatric Assessment, Second Edition. Boca Raton: CRC. pp. 26–32. ISBN 978-0-8493-8138-6 . Retrieved 2008-07-06.
- 1 2 Sullivan PG, Rabchevsky AG, Hicks RR, Gibson TR, Fletcher-Turner A, Scheff SW (2000). "Dose-response curve and optimal dosing regimen of cyclosporin A after traumatic brain injury in rats". Neuroscience. 101 (2): 289–95. doi:10.1016/S0306-4522(00)00380-8. PMID 11074152. S2CID 20457228.
- ↑ Sauaia A, Moore FA, Moore EE, et al. (February 1995). "Epidemiology of trauma deaths: A reassessment". J Trauma. 38 (2): 185–93. doi:10.1097/00005373-199502000-00006. PMID 7869433.
- ↑ Narayan RK, Michel ME, Ansell B, et al. (May 2002). "Clinical trials in head injury". J. Neurotrauma. 19 (5): 503–57. doi:10.1089/089771502753754037. PMC 1462953 . PMID 12042091.
- 1 2 Marion DW (2003). "Pathophysiology and treatment of intracranial hypertention". In Andrews BT (ed.). Intensive Care in Neurosurgery. New York: Thieme Medical Publishers. pp. 52–53. ISBN 1-58890-125-4 . Retrieved 2008-06-08.
- ↑ Andrews BT (2003). "Head injury management". In Andrews BT (ed.). Intensive Care in Neurosurgery. New York: Thieme Medical Publishers. p. 125. ISBN 1-58890-125-4 . Retrieved 2008-06-08.
- ↑ Garga N, Lowenstein DH (2006). "Posttraumatic epilepsy: A major problem in desperate need of major advances". Epilepsy Curr. 6 (1): 1–5. doi:10.1111/j.1535-7511.2005.00083.x. PMC 1363374 . PMID 16477313.
- ↑ Armin SS, Colohan AR, Zhang JH (June 2006). "Traumatic subarachnoid hemorrhage: Our current understanding and its evolution over the past half century". Neurol. Res. 28 (4): 445–52. doi:10.1179/016164106X115053. PMID 16759448. S2CID 23726077.