A patient is any recipient of health care services that are performed by healthcare professionals. The patient is most often ill or injured and in need of treatment by a physician, nurse, optometrist, dentist, veterinarian, or other health care provider.

Community health refers to non-treatment based health services that are delivered outside hospitals and clinics. Community health is a subset of public health that is taught to and practiced by clinicians as part of their normal duties. Community health volunteers and community health workers work with primary care providers to facilitate entry into, exit from and utilization of the formal health system by community members as well as providing supplementary services such as support groups or wellness events that are not offered by medical institutions.
Spatial epidemiology is a subfield of epidemiology focused on the study of the spatial distribution of health outcomes; it is closely related to health geography.
The Drug Effectiveness Review Project (DERP) is a self-governed collaboration of state Medicaid and public pharmacy programs that commission high-quality evidence-based research products to assist policymakers and other decision-makers grappling with difficult drug coverage decisions. Housed at the Center for Evidence-based Policy at Oregon Health & Science University in Portland, Oregon, DERP produces concise, comparative, evidence-based research products that evaluate the efficacy, effectiveness, and safety of drugs in many widely used drug classes.
A catchment area in human geography, is the area from which a location, such as a city, service or institution, attracts a population that uses its services and economic opportunities. Catchment areas may be defined based on from where people are naturally drawn to a location or as established by governments or organizations such as education authorities or healthcare providers, for the provision of services.

In medicine, rural health or rural medicine is the interdisciplinary study of health and health care delivery in rural environments. The concept of rural health incorporates many fields, including wilderness medicine, geography, midwifery, nursing, sociology, economics, and telehealth or telemedicine.
End-of-life care (EOLC) is health care provided in the time leading up to a person's death. End-of-life care can be provided in the hours, days, or months before a person dies and encompasses care and support for a person's mental and emotional needs, physical comfort, spiritual needs, and practical tasks.
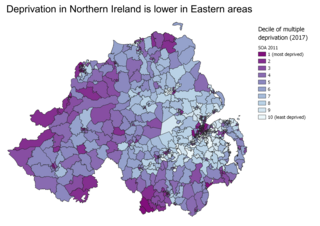
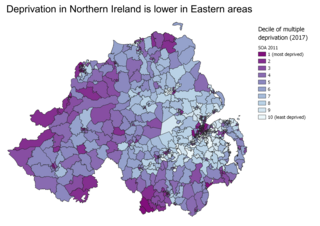
A deprivation index or poverty index is a data set to measure relative deprivation of small areas. Such indices are used in spatial epidemiology to identify socio-economic confounding.
In data analysis involving geographical locations, geo-imputation or geographical imputation methods are steps taken to replace missing values for exact locations with approximate locations derived from associated data. They assign a reasonable location or geographic based attribute to a person by using both the demographic characteristics of the person and the population characteristics from a larger geographic aggregate area in which the person was geocoded. For example, if a person's census tract was known and no other address information was available then geo-imputation methods could be used to probabilistically assign that person to a smaller geographic area, such as a census block group.
The two-step floating catchment area (2SFCA) method is a method for combining a number of related types of information into a single, immediately meaningful, index that allows comparisons to be made across different locations. Its importance lies in the improvement over considering the individual sources of information separately, where none on its own provides an adequate summary.
Primary Care Case Management (PCCM), is a program of the United States government healthcare service Medicaid. It oversees the United States system of managed care used by state Medicaid agencies in which a primary care provider is responsible for approving and monitoring the care of enrolled Medicaid beneficiaries, typically for a small monthly case management fee in addition to fee-for-service reimbursement for treatment. In the mid-1980s, states began enrolling beneficiaries in their PCCM programs in an attempt to increase access and reduce inappropriate emergency department and other high cost care. Use increased steadily through the 1990s.
Consumer Assessment of Healthcare Providers and Systems (CAHPS) refers to a set of surveys that ask patients to report on their health care experiences. The surveys are free to anyone who wants to use them. They focus on aspects of healthcare quality that patients find important and are well-equipped to assess, such as the communication skills of providers and ease of access to healthcare services. To customize a standardized CAHPS survey, users can add questions on a variety of topics.
Registered health information administrator (RHIA), previously known as registered record administrator, is a professional certification administered by the American Health Information Management Association (AHIMA) in the United States. Passing the exam results in certification for health information management.
The Patient Activation Measure (PAM) is a commercial product which assesses an individual's knowledge, skill, and confidence for managing one's health and healthcare. Individuals who measure high on this assessment typically understand the importance of taking a pro-active role in managing their health and have the skills and confidence to do so.

Women's health in India can be examined in terms of multiple indicators, which vary by geography, socioeconomic standing and culture. To adequately improve the health of women in India multiple dimensions of wellbeing must be analysed in relation to global health averages and also in comparison to men in India. Health is an important factor that contributes to human wellbeing and economic growth.

Cultural competence in healthcare refers to the ability for healthcare professionals to demonstrate cultural competence toward patients with diverse values, beliefs, and feelings. This process includes consideration of the individual social, cultural, and psychological needs of patients for effective cross-cultural communication with their health care providers. The goal of cultural competence in health care is to reduce health disparities and to provide optimal care to patients regardless of their race, gender, ethnic background, native languages spoken, and religious or cultural beliefs. Cultural competency training is important in health care fields where human interaction is common, including medicine, nursing, allied health, mental health, social work, pharmacy, oral health, and public health fields.
Rural health care in Australia involves the delivery of health services by private, community and public hospitals in areas classified as rural and remote. Researchers note that the health of those living in rural areas is quantitatively and qualitatively different to those living in major metropolitan areas. These differences include often significant gaps in service delivery, accessibility and lower health outcomes.

Renee Yuen-Jan Hsia is an American emergency physician. She is a professor of Emergency Medicine and Associate Chair of Health Services Research at the University of California, San Francisco, as well as an attending physician in the emergency department at the Zuckerberg San Francisco General Hospital and Trauma Center. She is also a core faculty member of the UCSF Philip R. Lee Institute for Health Policy Studies. Her research is aimed at studying how health services and regionalization of care impact access to emergency care.
The gap in socioeconomic status between racial groups in South Africa has been a key contributor to health disparities, with White South Africans, a minority group, having overall better health outcomes than majority Black South Africans. White South Africans, a minority group, have overall better access and health outcomes than other racial groups in South Africa. Black and Colored South Africans, have poorer overall health outcomes and are disproportionately unable to access the private healthcare system in South Africa.

Concerns of both a current and future shortage of medical doctors due to the supply and demand for physicians in the United States have come from multiple entities including professional bodies such as the American Medical Association (AMA). The AMA itself has been criticized for creating the shortage in the first place.