Related Research Articles

Dementia is a disorder which manifests as a set of related symptoms, which usually surfaces when the brain is damaged by injury or disease. The symptoms involve progressive impairments in memory, thinking, and behavior, which negatively affects a person's ability to function and carry out everyday activities. Aside from memory impairment and a disruption in thought patterns, the most common symptoms include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Consciousness is not affected. Dementia ultimately has a significant effect on the individual, caregivers, and on social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than what is caused by normal aging.

Binswanger's disease, also known as subcortical leukoencephalopathy and subcortical arteriosclerotic encephalopathy, is a form of small-vessel vascular dementia caused by damage to the white brain matter. White matter atrophy can be caused by many circumstances including chronic hypertension as well as old age. This disease is characterized by loss of memory and intellectual function and by changes in mood. These changes encompass what are known as executive functions of the brain. It usually presents between 54 and 66 years of age, and the first symptoms are usually mental deterioration or stroke.
Encephalopathy means any disorder or disease of the brain, especially chronic degenerative conditions. In modern usage, encephalopathy does not refer to a single disease, but rather to a syndrome of overall brain dysfunction; this syndrome has many possible organic and inorganic causes.

Progressive supranuclear palsy (PSP) is a late-onset degenerative disease involving the gradual deterioration and death of specific volumes of the brain. The condition leads to symptoms including loss of balance, slowing of movement, difficulty moving the eyes, and cognitive impairment. PSP may be mistaken for other neurodegenerative diseases such as Parkinson's, frontotemporal dementia and Alzheimer's. The cause of the condition is uncertain, but involves accumulation of tau protein within the brain. Medications such as levodopa and amantadine may be useful in some cases.
Semantic dementia (SD), also known as semantic variant primary progressive aphasia (svPPA), is a progressive neurodegenerative disorder characterized by loss of semantic memory in both the verbal and non-verbal domains. However, the most common presenting symptoms are in the verbal domain. Semantic dementia is a disorder of semantic memory that causes patients to lose the ability to match words or images to their meanings. However, it is fairly rare for patients with semantic dementia to develop category specific impairments, though there have been documented cases of it occurring. Typically, a more generalized semantic impairment results from dimmed semantic representations in the brain.

Primary progressive aphasia (PPA) is a type of neurological syndrome in which language capabilities slowly and progressively become impaired. As with other types of aphasia, the symptoms that accompany PPA depend on what parts of the left hemisphere are significantly damaged. However, unlike most other aphasias, PPA results from continuous deterioration in brain tissue, which leads to early symptoms being far less detrimental than later symptoms. Those with PPA slowly lose the ability to speak, write, read, and generally comprehend language. Eventually, almost every patient becomes mute and completely loses the ability to understand both written and spoken language. Although it was first described as solely impairment of language capabilities while other mental functions remain intact, it is now recognized that many, if not most of those with PPA experience impairment of memory, short-term memory formation and loss of executive functions. It was first described as a distinct syndrome by M. Marsel Mesulam in 1982. Primary progressive aphasias have a clinical and pathological overlap with the frontotemporal lobar degeneration (FTLD) spectrum of disorders and Alzheimer's disease. However, PPA is not considered synonymous to Alzheimer's disease due to the fact that, unlike those affected by Alzheimer's disease, those with PPA are generally able to maintain the ability to care for themselves, remain employed, and pursue interests and hobbies. Moreover, in diseases such as Alzheimer's disease, Pick's disease, and Creutzfeldt-Jakob disease, progressive deterioration of comprehension and production of language is just one of the many possible types of mental deterioration, such as the progressive decline of memory, motor skills, reasoning, awareness, and visuospatial skills.

A perivascular space, also known as a Virchow–Robin space, is a fluid-filled space surrounding certain blood vessels in several organs, including the brain, potentially having an immunological function, but more broadly a dispersive role for neural and blood-derived messengers. The brain pia mater is reflected from the surface of the brain onto the surface of blood vessels in the subarachnoid space. In the brain, perivascular cuffs are regions of leukocyte aggregation in the perivascular spaces, usually found in patients with viral encephalitis.

Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia. CBD symptoms typically begin in people from 50 to 70 years of age, and the average disease duration is six years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.
Toxic encephalopathy is a neurologic disorder caused by exposure to neurotoxic organic solvents such as toluene, following exposure to heavy metals such as manganese, as a side effect of melarsoprol treatment for African trypanosomiasis, adverse effects to prescription drugs, or exposure to extreme concentrations of any natural toxin such as cyanotoxins found in shellfish or freshwater cyanobacteria crusts. Toxic encephalopathy can occur following acute or chronic exposure to neurotoxicants, which includes all natural toxins. Exposure to toxic substances can lead to a variety of symptoms, characterized by an altered mental status, memory loss, and visual problems. Toxic encephalopathy can be caused by various chemicals, some of which are commonly used in everyday life, or cyanotoxins which are bio-accumulated from harmful algal blooms (HABs) which have settled on the benthic layer of a waterbody. Toxic encephalopathy can permanently damage the brain and currently treatment is mainly just for the symptoms.

Frontal lobe disorder, also frontal lobe syndrome, is an impairment of the frontal lobe of the brain due to disease or frontal lobe injury. The frontal lobe plays a key role in executive functions such as motivation, planning, social behaviour, and speech production. Frontal lobe syndrome can be caused by a range of conditions including head trauma, tumours, neurodegenerative diseases, neurodevelopmental disorders, neurosurgery and cerebrovascular disease. Frontal lobe impairment can be detected by recognition of typical signs and symptoms, use of simple screening tests, and specialist neurological testing.

Organic brain syndrome, also known as organic brain disease, organic brain disorder, organic mental syndrome, or organic mental disorder, refers to any syndrome or disorder of mental function whose cause is alleged to be known as organic (physiologic) rather than purely of the mind. These names are older and nearly obsolete general terms from psychiatry, referring to many physical disorders that cause impaired mental function. They are meant to exclude psychiatric disorders. Originally, the term was created to distinguish physical causes of mental impairment from psychiatric disorders, but during the era when this distinction was drawn, not enough was known about brain science for this cause-based classification to be more than educated guesswork labeled with misplaced certainty, which is why it has been deemphasized in current medicine. While mental or behavioural abnormalities related to the dysfunction can be permanent, treating the disease early may prevent permanent damage in addition to fully restoring mental functions. An organic cause to brain dysfunction is suspected when there is no indication of a clearly defined psychiatric or "inorganic" cause, such as a mood disorder.
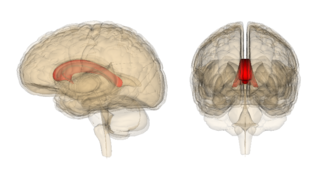
Marchiafava–Bignami disease is a progressive neurological disease of alcohol use disorder, characterized by corpus callosum demyelination and necrosis and subsequent atrophy. The disease was first described in 1903 by the Italian pathologists Amico Bignami and Ettore Marchiafava in an Italian Chianti drinker. In this autopsy, Marchiafava and Bignami noticed that the middle two-thirds of the corpus callosum were necrotic. It is very difficult to diagnose and there is no specific treatment. Until 2008 only around 300 cases had been reported. If caught early enough, most patients survive.
Alcohol-related dementia (ARD) is an alcohol-related cognitive impairment. While the validity of classifying ARD clinically is debated, it refers to a recognized neurocognitive conditions believed to be caused by long-term, excessive consumption of alcoholic beverages.
Mild cognitive impairment (MCI) is a neurocognitive disorder which involves cognitive impairments beyond those expected based on an individual's age and education but which are not significant enough to interfere with instrumental activities of daily living. MCI may occur as a transitional stage between normal aging and dementia, especially Alzheimer's disease. It includes both memory and non-memory impairments. The cause of the disorder remains unclear, as well as both its prevention and treatment, with some 50 percent of people diagnosed with it going on to develop Alzheimer's disease within five years. The diagnosis can also serve as an early indicator for other types of dementia, although MCI may remain stable or even remit.
Pseudodementia is a condition where mental cognition can be temporarily decreased. The term pseudodementia is applied to the range of functional psychiatric conditions such as depression and schizophrenia, that may mimic organic dementia, but are essentially reversible on treatment. Pseudodementia typically involves three cognitive components: memory issues, deficits in executive functioning, and deficits in speech and language. Specific cognitive symptoms might include trouble recalling words or remembering things in general, decreased attentional control and concentration, difficulty completing tasks or making decisions, decreased speed and fluency of speech, and impaired processing speed. People with pseudodementia are typically very distressed about the cognitive impairment they experience. There are two specific treatments that have been found to be effective for the treatment of depression, and these treatments may also be beneficial in the treatment of pseudodementia. Cognitive behavioral therapy (CBT) involves exploring and changing thought patterns and behaviors in order to improve one's mood. Interpersonal therapy focuses on the exploration of an individual's relationships and identifying any ways in which they may be contributing to feelings of depression. Some antidepressant drugs have also been found to alleviate cognitive deficits arising from depression; in particular, the novel SSRI vortioxetine has been studied for treating pseudodementia.

Posterior cortical atrophy (PCA), also called Benson's syndrome, is a rare form of dementia which is considered a visual variant or an atypical variant of Alzheimer's disease (AD). The disease causes atrophy of the posterior part of the cerebral cortex, resulting in the progressive disruption of complex visual processing. PCA was first described by D. Frank Benson in 1988.

A neurological disorder is any disorder of the nervous system. Structural, biochemical or electrical abnormalities in the brain, spinal cord or other nerves can result in a range of symptoms. Examples of symptoms include paralysis, muscle weakness, poor coordination, loss of sensation, seizures, confusion, pain and altered levels of consciousness. There are many recognized neurological disorders, some relatively common, but many rare. They may be assessed by neurological examination, and studied and treated within the specialities of neurology and clinical neuropsychology.
Pleurothotonus, commonly known as Pisa syndrome, is a rare neurological disorder which occurs due to prolonged exposure to antipsychotic drugs. It is characterized by dystonia, and abnormal and sustained involuntary muscle contraction. This may cause twisting or jerking movements of the body or a body part. Although Pisa syndrome develops most commonly in those undergoing long-term treatment with antipsychotics, it has been reported less frequently in patients receiving other medications, such as an acetylcholinesterase inhibitor. However, it has also been seen in those with other diseases causing neurodegeneration and in those who are not receiving any medication. The characteristic development of Pisa syndrome consists of two types of dystonia: acute dystonia and tardive dystonia. The underlying pathology of drug-induced Pisa syndrome is very complex, and development may be due to an underlying dopaminergic-cholinergic imbalance, or serotonergic/noradrenergic dysfunction.
Chronic solvent-induced encephalopathy (CSE) is a condition induced by long-term exposure to organic solvents, often - but not always - in the workplace, that lead to a wide variety of persisting sensorimotor polyneuropathies and neurobehavioral deficits even after solvent exposure has been removed. This syndrome can also be referred to as psycho-organic syndrome, organic solvent syndrome, chronic painter's syndrome, occupational solvent encephalopathy, solvent intoxication, toxic solvent syndrome, painters disease, psycho-organic syndrome, chronic toxic encephalopathy, or neurasthenic syndrome. The multiple names of solvent-induced syndromes combined with inconsistency in research methods makes referencing this disease difficult and its catalog of symptoms vague.
Steroid dementia syndrome describes the signs and symptoms of hippocampal and prefrontal cortical dysfunction, such as deficits in memory, attention, and executive function, induced by glucocorticoids. Dementia-like symptoms have been found in some individuals who have been exposed to glucocorticoid medication, often dispensed in the form of asthma, arthritis, and anti-inflammatory steroid medications. The condition reverses, but not always completely, within months after steroid treatment is stopped.
References
- 1 2 3 "psycho-organic syndrome". TheFreeDictionary.com. Retrieved 2015-11-02.
- 1 2 3 "Does the psycho-organic syndrome exist?". www.researchgate.net. Retrieved 2015-11-02.
- 1 2 3 4 "The main symptoms of psycho-organic syndrome". medical-notes-help.com. Archived from the original on 2015-12-22. Retrieved 2015-11-02.
- 1 2 3 4 5 6 "PEOI General psychopathology". www.peoi.org. Retrieved 2015-11-03.
- 1 2 "Organic brain diseases". www.peoi.org. Retrieved 2015-11-03.
- 1 2 Dick, F D (2006-03-01). "Solvent neurotoxicity". Occupational and Environmental Medicine. 63 (3): 221–226. doi:10.1136/oem.2005.022400. ISSN 1351-0711. PMC 2078137 . PMID 16497867.
- ↑ Möller, C.; Odkvist, L. M.; Thell, J.; Larsby, B.; Hydén, D.; Bergholtz, L. M.; Tham, R. (1989-02-01). "Otoneurological findings in psycho-organic syndrome caused by industrial solvent exposure". Acta Oto-Laryngologica. 107 (1–2): 5–12. doi:10.3109/00016488909127473. ISSN 0001-6489. PMID 2784610.
- ↑ Thomas, C.; Driessen, M.; Arolt, V. (2010-05-01). "[Diagnostic work-up and treatment of acute psycho-organic syndrome]". Der Nervenarzt. 81 (5): 613–628, quiz 629–630. doi:10.1007/s00115-010-3013-9. ISSN 1433-0407. PMC 7095979 . PMID 20454878.
- ↑ Dick, F D (2006-03-01). "Solvent neurotoxicity". Occupational and Environmental Medicine. 63 (3): 221–226. doi:10.1136/oem.2005.022400. ISSN 1351-0711. PMC 2078137 . PMID 16497867.
- ↑ Flodin, Ulf; Edling, Christer; Axelson, Olav (1984-01-01). "Clinical studies of psychoorganic syndromes among workers with exposure to solvents". American Journal of Industrial Medicine. 5 (4): 287–295. doi:10.1002/ajim.4700050405. ISSN 1097-0274. PMID 6720692.