Nail clubbing, also known as digital clubbing or clubbing, is a deformity of the finger or toe nails associated with a number of diseases, mostly of the heart and lungs. When it occurs together with joint effusions, joint pains, and abnormal skin and bone growth it is known as hypertrophic osteoarthropathy.

Pulmonary hypertension is a condition of increased blood pressure in the arteries of the lungs. Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise. Onset is typically gradual. According to the definition at the 6th World Symposium of Pulmonary Hypertension in 2018, a patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 20mmHg at rest, revised down from a purely arbitrary 25mmHg, and pulmonary vascular resistance (PVR) greater than 3 Wood units.
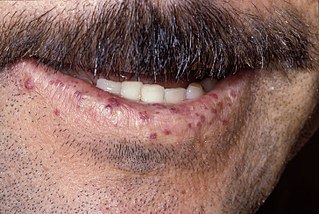
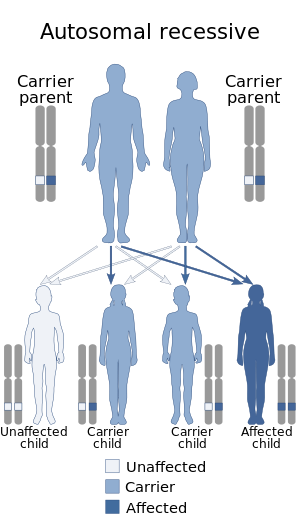
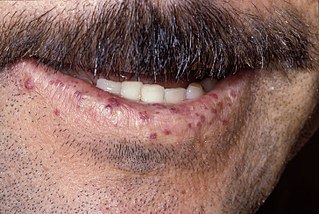
Hereditary hemorrhagic telangiectasia (HHT), also known as Osler–Weber–Rendu disease and Osler–Weber–Rendu syndrome, is a rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation in the skin, mucous membranes, and often in organs such as the lungs, liver, and brain.

Eisenmenger syndrome or Eisenmenger's syndrome is defined as the process in which a long-standing left-to-right cardiac shunt caused by a congenital heart defect causes pulmonary hypertension and eventual reversal of the shunt into a cyanotic right-to-left shunt. Because of the advent of fetal screening with echocardiography early in life, the incidence of heart defects progressing to Eisenmenger syndrome has decreased.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

CREST syndrome, also known as the limited cutaneous form of systemic sclerosis (lcSSc), is a multisystem connective tissue disorder. The acronym "CREST" refers to the five main features: calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia.

Pulmonary angiography is a medical fluoroscopic procedure used to visualize the pulmonary arteries and much less frequently, the pulmonary veins. It is a minimally invasive procedure performed most frequently by an interventional radiologist or interventional cardiologist to visualise the arteries of the lungs.

Lymphangioleiomyomatosis (LAM) is a rare, progressive and systemic disease that typically results in cystic lung destruction. It predominantly affects women, especially during childbearing years. The term sporadic LAM is used for patients with LAM not associated with tuberous sclerosis complex (TSC), while TSC-LAM refers to LAM that is associated with TSC.

Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss, and nail clubbing. Complications may include pulmonary hypertension, respiratory failure, pneumothorax, and lung cancer.

Iloprost is a medication used to treat pulmonary arterial hypertension (PAH), scleroderma, Raynaud's phenomenon and other diseases in which the blood vessels are constricted and blood cannot flow to the tissues. This damages the tissues and causes high blood pressure. There is ongoing research into using it as a frostbite treatment. Iloprost works by opening (dilating) the blood vessels to allow the blood to flow through again. It was developed by the pharmaceutical company Schering AG and is marketed by Bayer Schering Pharma AG in Europe and Actelion Pharmaceuticals in the USA. Iloprost is given via inhalation, and a therapeautic benefit of the drug is that a very low dose is required because of the deposition in the lung. Iloprost has few systemic side effects for that reason.

In thoracic surgery, a pulmonary thromboendarterectomy (PTE), also referred to as pulmonary endarterectomy (PEA), is an operation that removes organized clotted blood (thrombus) from the pulmonary arteries, which supply blood to the lungs.
Portopulmonary hypertension (PPH) is defined by the coexistence of portal and pulmonary hypertension. PPH is a serious complication of liver disease, present in 0.25 to 4% of all patients with cirrhosis. Once an absolute contraindication to liver transplantation, it is no longer, thanks to rapid advances in the treatment of this condition. Today, PPH is comorbid in 4-6% of those referred for a liver transplant.

Lymphangiomatosis is a condition where a lymphangioma is not present in a single localised mass, but in a widespread or multifocal manner. It is a rare type of tumor which results from an abnormal development of the lymphatic system.
DLCO or TLCO is the extent to which oxygen passes from the air sacs of the lungs into the blood. Commonly, it refers to the test used to determine this parameter. It was introduced in 1909.
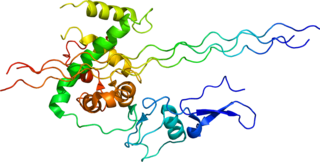
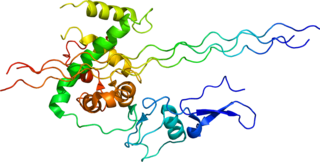
Type III Collagen is a homotrimer, or a protein composed of three identical peptide chains (monomers), each called an alpha 1 chain of type III collagen. Formally, the monomers are called collagen type III, alpha-1 chain and in humans are encoded by the COL3A1 gene. Type III collagen is one of the fibrillar collagens whose proteins have a long, inflexible, triple-helical domain.
In medicine, hepatopulmonary syndrome is a syndrome of shortness of breath and hypoxemia caused by vasodilation in the lungs of patients with liver disease. Dyspnea and hypoxemia are worse in the upright position.

Pulmonary veno-occlusive disease (PVOD) is a rare form of pulmonary hypertension caused by progressive blockage of the small veins in the lungs. The blockage leads to high blood pressures in the arteries of the lungs, which, in turn, leads to heart failure. The disease is progressive and fatal, with median survival of about 2 years from the time of diagnosis to death. The definitive therapy is lung transplantation.

Pulmonary alveolar microlithiasis (PAM) is a rare, inherited disorder of lung phosphate balance that is associated with small stone formation in the airspaces of the lung. Mutations in the gene SLC34A2 result in loss of a key sodium, phosphate co-transporter, known to be expressed in distal alveolar type II cells, as well as in the mammary gland, and to a lesser extent in intestine, kidney, skin, prostate and testes. As the disease progresses, the lung fields become progressively more dense (white) on the chest xray, and low oxygen level, lung inflammation and fibrosis, elevated pressures in the lung blood vessels, and respiratory failure ensue, usually in middle age. The clinical course of PAM can be highly variable, with some patients remaining asymptomatic for decades, and others progressing more rapidly. There is no effective treatment, and the mechanisms of stone formation, inflammation and scarring are not known.