Related Research Articles
Health care reform is for the most part governmental policy that affects health care delivery in a given place. Health care reform typically attempts to:
Socialized medicine is a term used in the United States to describe and discuss systems of universal health care—medical and hospital care for all by means of government regulation of health care and subsidies derived from taxation. Because of historically negative associations with socialism in American culture, the term is usually used pejoratively in American political discourse. The term was first widely used in the United States by advocates of the American Medical Association in opposition to President Harry S. Truman's 1947 health care initiative. It was later used in opposition to Medicare. The Affordable Care Act has been described in terms of socialized medicine, but the act's objective is rather socialized insurance, not government ownership of hospitals and other facilities as is common in other nations.
A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.

Health economics is a branch of economics concerned with issues related to efficiency, effectiveness, value and behavior in the production and consumption of health and healthcare. Health economics is important in determining how to improve health outcomes and lifestyle patterns through interactions between individuals, healthcare providers and clinical settings. In broad terms, health economists study the functioning of healthcare systems and health-affecting behaviors such as smoking, diabetes, and obesity.

Publicly funded healthcare is a form of health care financing designed to meet the cost of all or most healthcare needs from a publicly managed fund. Usually this is under some form of democratic accountability, the right of access to which are set down in rules applying to the whole population contributing to the fund or receiving benefits from it.

The healthcare industry is an aggregation and integration of sectors within the economic system that provides goods and services to treat patients with curative, preventive, rehabilitative, and palliative care. It encompasses the creation and commercialization of products and services conducive to the preservation and restoration of well-being. The contemporary healthcare sector comprises three fundamental facets, namely services, products, and finance. It can be further subdivided into numerous sectors and categories and relies on interdisciplinary teams of highly skilled professionals and paraprofessionals to address the healthcare requirements of both individuals and communities.
Health insurance or medical insurance is a type of insurance that covers the whole or a part of the risk of a person incurring medical expenses. As with other types of insurance, risk is shared among many individuals. By estimating the overall risk of health risk and health system expenses over the risk pool, an insurer can develop a routine finance structure, such as a monthly premium or payroll tax, to provide the money to pay for the health care benefits specified in the insurance agreement. The benefit is administered by a central organization, such as a government agency, private business, or not-for-profit entity.

Two-tier healthcare is a situation in which a basic government-provided healthcare system provides basic care, and a secondary tier of care exists for those who can pay for additional, better quality or faster access. Most countries have both publicly and privately funded healthcare, but the degree to which it creates a quality differential depends on the way the two systems are managed, funded, and regulated.

Primary care trusts (PCTs) were part of the National Health Service in England from 2001 to 2013. PCTs were largely administrative bodies, responsible for commissioning primary, community and secondary health services from providers. Until 31 May 2011, they also provided community health services directly. Collectively PCTs were responsible for spending around 80 per cent of the total NHS budget. Primary care trusts were abolished on 31 March 2013 as part of the Health and Social Care Act 2012, with their work taken over by clinical commissioning groups.

Healthcare in the United Kingdom is a devolved matter, with England, Northern Ireland, Scotland and Wales each having their own systems of publicly funded healthcare, funded by and accountable to separate governments and parliaments, together with smaller private sector and voluntary provision. As a result of each country having different policies and priorities, a variety of differences have developed between these systems since devolution.

The National Health Service and Community Care Act 1990 introduced an internal market into the supply of healthcare in the United Kingdom, making the state an 'enabler' rather than a supplier of health and social care provision.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use for most people. The NHS also conducts research through the National Institute for Health and Care Research (NIHR).
Healthcare in England is mainly provided by the National Health Service (NHS), a public body that provides healthcare to all permanent residents in England, that is free at the point of use. The body is one of four forming the UK National Health Service as health is a devolved matter; there are differences with the provisions for healthcare elsewhere in the United Kingdom, and in England it is overseen by NHS England. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing and able to pay.
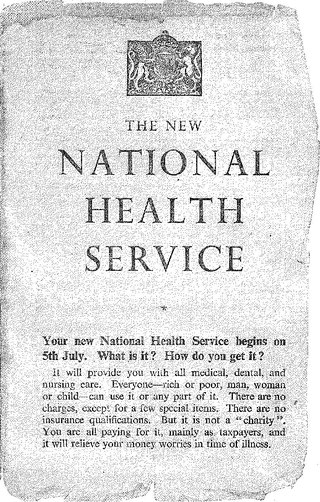
The National Health Service in England was created by the National Health Service Act 1946. Responsibility for the NHS in Wales was passed to the Secretary of State for Wales in 1969, leaving the Secretary of State for Social Services responsible for the NHS in England by itself.

The Health and Social Care Act 2012 is an act of the Parliament of the United Kingdom. It provided for the most extensive reorganisation of the structure of the National Health Service in England to date. It removed responsibility for the health of citizens from the Secretary of State for Health, which the post had carried since the inception of the NHS in 1948. It abolished primary care trusts (PCTs) and strategic health authorities (SHAs) and transferred between £60 billion and £80 billion of "commissioning", or healthcare funds, from the abolished PCTs to several hundred clinical commissioning groups, partly run by the general practitioners (GPs) in England. A new executive agency of the Department of Health, Public Health England, was established under the act on 1 April 2013.

The National Health Action Party (NHA) is a political party in the United Kingdom.

Private healthcare in the UK, where universal state-funded healthcare is provided by the National Health Service, is a niche market.
The NHS internal market was established by the National Health Service and Community Care Act 1990, to separate the roles of purchasers and providers within the National Health Service in the United Kingdom. Previously, healthcare was provided by regional health authorities which were given a budget to run hospitals and community health services in their area. The Health and Social Care Act 2012 was intended to open up the internal market to external competition. The 2019 NHS Long Term Plan called for the establishment of integrated care systems across England by 2021, effectively ending the internal market.
The private provision of NHS services has been considered a controversial topic since the early 1990s. Keep Our NHS Public, NHS Support Federation and other groups have campaigned against the threat of privatisation, largely in England.
References
- 1 2 Lewis, Paul. (2017). Quasi-markets: An Overview and Analysis
- ↑ Carey, Gemma; Malbon, Eleanor; Green, Celia; Reeders, Daniel; Marjolin, Axelle (2020-01-02). "Quasi-market shaping, stewarding and steering in personalization: the need for practice-orientated empirical evidence". Policy Design and Practice. 3 (1): 30–44. doi: 10.1080/25741292.2019.1704985 . S2CID 214424506.
- ↑ Jordahl, Henrik (19 December 2019). "Perspectives on Public Sector Outsourcing: Quasi-markets and Prices". CESifo Economic Studies. 65 (4): 343–348. doi: 10.1093/cesifo/ifz015 . Retrieved 2023-04-23.
- ↑ Grand, Julian Le; Bartlett, Will, eds. (1993). Quasi-Markets and Social Policy. doi:10.1007/978-1-349-22873-7. ISBN 978-0-333-56519-3.
- ↑ Jordahl, Henrik (2019-12-01). "Perspectives on Public Sector Outsourcing: Quasi-markets and Prices". CESifo Economic Studies. 65 (4): 343–348. doi: 10.1093/cesifo/ifz015 . ISSN 1610-241X.
- ↑ Klein, Rudolf (27 November 1999). "Markets, politicians, and the NHS". British Medical Journal. 319 (7222): 1383–4. doi:10.1136/bmj.319.7222.1383. PMC 1117121 . PMID 10574834.
- ↑ Arrow, Kenneth (December 1963). "Uncertainty and the Welfare Economics of Medical Care" (PDF). American Economic Review. LIII (5).
- ↑ Valkama, Pekka; Kankaanpää, Jari; Anttiroiko, Ari-Veikko (June 2018). "Financial and structural impacts of quasi-marketization of the Helsinki Metropolitan Area's bus services". Case Studies on Transport Policy. 6 (2): 246–256. doi: 10.1016/j.cstp.2018.04.002 . S2CID 55793724 – via Elsevier Science Direct.