Chilblains, also known as pernio, is a medical condition in which damage occurs to capillary beds in the skin, most often in the hands or feet, when blood perfuses into the nearby tissue, resulting in redness, itching, inflammation, and possibly blisters.

A bruise, also known as a contusion, is a type of hematoma of tissue, the most common cause being capillaries damaged by trauma, causing localized bleeding that extravasates into the surrounding interstitial tissues. Most bruises occur close enough to the epidermis such that the bleeding causes a visible discoloration. The bruise then remains visible until the blood is either absorbed by tissues or cleared by immune system action. Bruises which do not blanch under pressure can involve capillaries at the level of skin, subcutaneous tissue, muscle, or bone.

Vasculitis is a group of disorders that destroy blood vessels by inflammation. Both arteries and veins are affected. Lymphangitis is sometimes considered a type of vasculitis. Vasculitis is primarily caused by leukocyte migration and resultant damage. Although both occur in vasculitis, inflammation of veins (phlebitis) or arteries (arteritis) on their own are separate entities.

Rosacea is a long-term skin condition that typically affects the face. It results in redness, pimples, swelling, and small and superficial dilated blood vessels. Often, the nose, cheeks, forehead, and chin are most involved. A red, enlarged nose may occur in severe disease, a condition known as rhinophyma.

Henoch–Schönlein purpura (HSP), also known as IgA vasculitis, is a disease of the skin, mucous membranes, and sometimes other organs that most commonly affects children. In the skin, the disease causes palpable purpura, often with joint pain and abdominal pain. With kidney involvement, there may be a loss of small amounts of blood and protein in the urine, but this usually goes unnoticed; in a small proportion of cases, the kidney involvement proceeds to chronic kidney disease. HSP is often preceded by an infection, such as a throat infection.

Purpura is a condition of red or purple discolored spots on the skin that do not blanch on applying pressure. The spots are caused by bleeding underneath the skin secondary to platelet disorders, vascular disorders, coagulation disorders, or other causes. They measure 3–10 mm, whereas petechiae measure less than 3 mm, and ecchymoses greater than 1 cm.
Vulvitis is inflammation of the vulva, the external female mammalian genitalia that include the labia majora, labia minora, clitoris, and introitus. It may co-occur as vulvovaginitis with vaginitis, inflammation of the vagina, and may have infectious or non-infectious causes. The warm and moist conditions of the vulva make it easily affected. Vulvitis is prone to occur in any female especially those who have certain sensitivities, infections, allergies, or diseases that make them likely to have vulvitis. Postmenopausal women and prepubescent girls are more prone to be affected by it, as compared to women in their menstruation period. It is so because they have low estrogen levels which makes their vulvar tissue thin and dry. Women having diabetes are also prone to be affected by vulvitis due to the high sugar content in their cells, increasing their vulnerability. Vulvitis is not a disease, it is just an inflammation caused by an infection, allergy or injury. Vulvitis may also be symptom of any sexually transmitted infection or a fungal infection.

Sweet syndrome (SS), or acute febrile neutrophilic dermatosis, is a skin disease characterized by the sudden onset of fever, an elevated white blood cell count, and tender, red, well-demarcated papules and plaques that show dense infiltrates by neutrophil granulocytes on histologic examination.
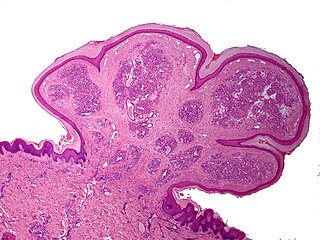
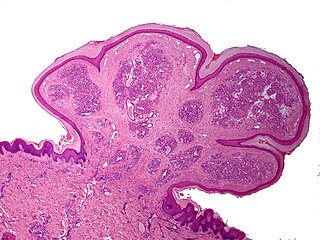
A pyogenic granuloma or lobular capillary hemangioma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh.

Angiokeratoma is a benign cutaneous lesion of capillaries, resulting in small marks of red to blue color and characterized by hyperkeratosis. Angiokeratoma corporis diffusum refers to Fabry's disease, but this is usually considered a distinct condition.

Pruritic urticarial papules and plaques of pregnancy (PUPPP), known in United Kingdom as polymorphic eruption of pregnancy (PEP), is a chronic hives-like rash that strikes some women during pregnancy. Some skin changes are known to occur in people who are pregnant while other skin conditions, or dermatoses, that people have prior to getting pregnant will become altered or symptoms will increase. Pruritic urticarial papules and plaques of pregnancy (PUPPP) is one of many skin conditions that is specific to pregnancy and occurs in about 1 in every 160 (0.625%) of pregnancies.

Granuloma annulare (GA) is a common, sometimes chronic skin condition which presents as reddish bumps on the skin arranged in a circle or ring. It can initially occur at any age, though two-thirds of patients are under 30 years old, and it is seen most often in children and young adults. Females are two times as likely to have it as males.

Grover's disease (GD) is a polymorphic, pruritic, papulovesicular dermatosis characterized histologically by acantholysis with or without dyskeratosis. Once confirmed, most cases of Grover's disease last six to twelve months, which is why it was originally called "transient". However it may last much longer. Nevertheless, it is not to be confused with relapsing linear acantholytic dermatosis.
Cerebral vasculitis is vasculitis involving the brain and occasionally the spinal cord. It affects all of the vessels: very small blood vessels (capillaries), medium-size blood vessels, or large blood vessels. If blood flow in a vessel with vasculitis is reduced or stopped, the parts of the body that receive blood from that vessel begins to die. It may produce a wide range of neurological symptoms, such as headache, skin rashes, feeling very tired, joint pains, difficulty moving or coordinating part of the body, changes in sensation, and alterations in perception, thought or behavior, as well as the phenomena of a mass lesion in the brain leading to coma and herniation. Some of its signs and symptoms may resemble multiple sclerosis. 10% have associated bleeding in the brain.

Dermatitis herpetiformis (DH) is a chronic autoimmune blistering skin condition, characterised by intensely itchy blisters filled with a watery fluid. DH is a cutaneous manifestation of coeliac disease, although the exact causal mechanism is not known. DH is neither related to nor caused by herpes virus; the name means that it is a skin inflammation having an appearance similar to herpes.
Necrotizing vasculitis, also called systemic necrotizing vasculitus, is a category of vasculitis, comprising vasculitides that present with necrosis. Examples include giant cell arteritis, microscopic polyangiitis, and granulomatosis with polyangiitis. ICD-10 uses the variant "necrotizing vasculopathy". ICD-9, while classifying these conditions together, does not use a dedicated phrase, instead calling them "polyarteritis nodosa and allied conditions".

Pigmented purpuric dermatosis refers to one of the three major classes of skin conditions characterized by purpuric skin eruptions.

Cutaneous small-vessel vasculitis (CSVV), is inflammation of small blood vessels, usually accompanied by small lumps beneath the skin. The condition is also known as hypersensitivity vasculitis, cutaneous leukocytoclastic vasculitis, hypersensitivity angiitis, cutaneous leukocytoclastic angiitis, cutaneous necrotizing vasculitis and cutaneous necrotizing venulitis,
Cutaneous manifestations of COVID-19 are characteristic signs or symptoms of the Coronavirus disease 2019 that occur in the skin. The American Academy of Dermatology reports that skin lesions such as morbilliform, pernio, urticaria, macular erythema, vesicular purpura, papulosquamous purpura and retiform purpura are seen in people with COVID-19. Pernio-like lesions were more common in mild disease while retiform purpura was seen only in critically ill patients. The major dermatologic patterns identified in individuals with COVID-19 are urticarial rash, confluent erythematous/morbilliform rash, papulovesicular exanthem, chilbain-like acral pattern, livedo reticularis and purpuric "vasculitic" pattern. Chilblains and Multisystem inflammatory syndrome in children are also cutaneous manifestations of COVID-19.
Retiform purpura is the result of total vascular blockage and damage to the skin's blood vessels. These lesions can appear due to intravascular issues where clots, proteins, or emboli block skin vessels. They can also result from direct harm to the vessel walls, as seen in conditions like vasculitis, calciphylaxis, and certain severe opportunistic infections.