Skin is the layer of usually soft, flexible outer tissue covering the body of a vertebrate animal, with three main functions: protection, regulation, and sensation.

The integumentary system is the set of organs forming the outermost layer of an animal's body. It comprises the skin and its appendages, which act as a physical barrier between the external environment and the internal environment that it serves to protect and maintain the body of the animal. Mainly it is the body's outer skin.

Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells. Basal cells in the basal layer of the skin are sometimes referred to as basal keratinocytes. Keratinocytes form a barrier against environmental damage by heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses. A number of structural proteins, enzymes, lipids, and antimicrobial peptides contribute to maintain the important barrier function of the skin. Keratinocytes differentiate from epidermal stem cells in the lower part of the epidermis and migrate towards the surface, finally becoming corneocytes and eventually be shed off, which happens every 40 to 56 days in humans.
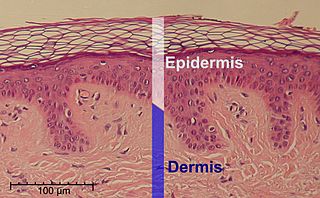
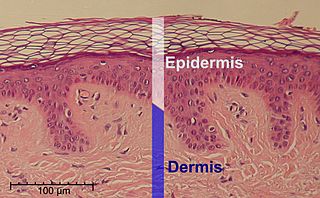
The epidermis is the outermost of the three layers that comprise the skin, the inner layers being the dermis and hypodermis. The epidermis layer provides a barrier to infection from environmental pathogens and regulates the amount of water released from the body into the atmosphere through transepidermal water loss.

The Malpighian layer of the epidermis is generally defined as both the stratum basale and the thicker stratum spinosum immediately above it as a single unit, although it is occasionally defined as the stratum basale specifically, or the stratum spinosum specifically.

A skin condition, also known as cutaneous condition, is any medical condition that affects the integumentary system—the organ system that encloses the body and includes skin, nails, and related muscle and glands. The major function of this system is as a barrier against the external environment.

The stratum corneum is the outermost layer of the epidermis. The human stratum corneum comprises several levels of flattened corneocytes that are divided into two layers: the stratum disjunctum and stratum compactum. The skin's protective acid mantle and lipid barrier sit on top of the stratum disjunctum. The stratum disjunctum is the uppermost and loosest layer of skin. The stratum compactum is the comparatively deeper, more compacted and more cohesive part of the stratum corneum. The corneocytes of the stratum disjunctum are larger, more rigid and more hydrophobic than that of the stratum compactum.

The stratum basale is the deepest layer of the five layers of the epidermis, the external covering of skin in mammals.

Desquamation occurs when the outermost layer of a tissue, such as the skin, is shed. The term is from Latin desquamare 'to scrape the scales off a fish'.

The stratum lucidum is a thin, clear layer of dead skin cells in the epidermis named for its translucent appearance under a microscope. It is readily visible by light microscopy only in areas of thick skin, which are found on the palms of the hands and the soles of the feet.

The stratum granulosum is a thin layer of cells in the epidermis lying above the stratum spinosum and below the stratum corneum. Keratinocytes migrating from the underlying stratum spinosum become known as granular cells in this layer. These cells contain keratohyalin granules, which are filled with histidine- and cysteine-rich proteins that appear to bind the keratin filaments together. Therefore, the main function of keratohyalin granules is to bind intermediate keratin filaments together.

The stratum spinosum is a layer of the epidermis found between the stratum granulosum and stratum basale. This layer is composed of polyhedral keratinocytes. These are joined with desmosomes. Their spiny appearance is due to shrinking of the microfilaments between desmosomes that occurs when stained with H&E. Keratinization begins in the stratum spinosum, although the actual keratinocytes begin in the stratum basale. They have large pale-staining nuclei as they are active in synthesizing fibrilar proteins, known as cytokeratin, which build up within the cells aggregating together forming tonofibrils. The tonofibrils go on to form the desmosomes, which allow for strong connections to form between adjacent keratinocytes. The stratum spinosum also contains Langerhans cells, which functions as a macrophage by engulfing bacteria, foreign particles, and damaged cells that occur in this layer.
The oral mucosa is the mucous membrane lining the inside of the mouth. It comprises stratified squamous epithelium, termed "oral epithelium", and an underlying connective tissue termed lamina propria. The oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which can reveal systemic conditions, such as diabetes or vitamin deficiency, or the local effects of chronic tobacco or alcohol use. The oral mucosa tends to heal faster and with less scar formation compared to the skin. The underlying mechanism remains unknown, but research suggests that extracellular vesicles might be involved.
Snakeskin may either refer to the skin of a live snake, the shed skin of a snake after molting, or to a type of leather that is made from the hide of a dead snake. Snakeskin and scales can have varying patterns and color formations, providing protection via camouflage from predators. The colors and iridescence in these scales are largely determined by the types and amount of chromatophores located in the dermis of the snake skin. The snake's skin and scales are also an important feature to their locomotion, providing protection and minimizing friction when gliding over surfaces.

A stratified squamous epithelium consists of squamous (flattened) epithelial cells arranged in layers upon a basal membrane. Only one layer is in contact with the basement membrane; the other layers adhere to one another to maintain structural integrity. Although this epithelium is referred to as squamous, many cells within the layers may not be flattened; this is due to the convention of naming epithelia according to the cell type at the surface. In the deeper layers, the cells may be columnar or cuboidal. There are no intercellular spaces. This type of epithelium is well suited to areas in the body subject to constant abrasion, as the thickest layers can be sequentially sloughed off and replaced before the basement membrane is exposed. It forms the outermost layer of the skin and the inner lining of the mouth, esophagus and vagina.

In cell biology, lamellar bodies are secretory organelles found in type II alveolar cells in the lungs, and in keratinocytes in the skin. They are oblong structures, appearing about 300-400 nm in width and 100-150 nm in length in transmission electron microscopy images. Lamellar bodies in the alveoli of the lungs fuse with the cell membrane and release pulmonary surfactant into the extracellular space.
Corneocytes are terminally differentiated keratinocytes and compose most of the stratum corneum, the outermost layer of the epidermis. They are regularly replaced through desquamation and renewal from lower epidermal layers and are essential for its function as a skin barrier.

Bullous impetigo is a bacterial skin infection caused by Staphylococcus aureus that results in the formation of large blisters called bullae, usually in areas with skin folds like the armpit, groin, between the fingers or toes, beneath the breast, and between the buttocks. It accounts for 30% of cases of impetigo, the other 70% being non-bullous impetigo.
Skin sloughing is the process of shedding dead surface cells from the skin. It is most associated with cosmetic skin maintenance via exfoliation, but can also occur biologically or for medical reasons.
TGM5 is a transglutaminase enzyme.