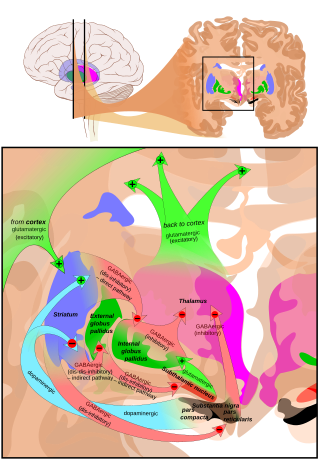
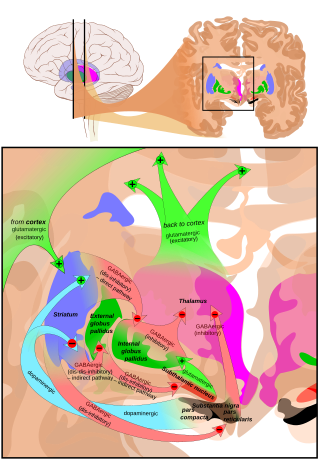
The putamen is a round structure located at the base of the forebrain (telencephalon). The putamen and caudate nucleus together form the dorsal striatum. It is also one of the structures that compose the basal nuclei. Through various pathways, the putamen is connected to the substantia nigra, the globus pallidus, the claustrum, and the thalamus, in addition to many regions of the cerebral cortex. A primary function of the putamen is to regulate movements at various stages and influence various types of learning. It employs GABA, acetylcholine, and enkephalin to perform its functions. The putamen also plays a role in degenerative neurological disorders, such as Parkinson's disease.

Binswanger's disease, also known as subcortical leukoencephalopathy and subcortical arteriosclerotic encephalopathy, is a form of small-vessel vascular dementia caused by damage to the white brain matter. White matter atrophy can be caused by many circumstances including chronic hypertension as well as old age. This disease is characterized by loss of memory and intellectual function and by changes in mood. These changes encompass what are known as executive functions of the brain. It usually presents between 54 and 66 years of age, and the first symptoms are usually mental deterioration or stroke.
Lewy body dementia is an umbrella term for two similar and common subtypes of dementia: dementia with Lewy bodies (DLB) and Parkinson's disease dementia (PDD). Both are characterized by changes in thinking, movement, behavior, and mood. The two conditions have similar features and may have similar causes, and are believed to belong on a spectrum of Lewy body disease that includes Parkinson's disease. As of 2014, they were more often misdiagnosed than any other common dementia.

The caudate nucleus is one of the structures that make up the corpus striatum, which is a component of the basal ganglia in the human brain. While the caudate nucleus has long been associated with motor processes due to its role in Parkinson's disease, it plays important roles in various other nonmotor functions as well, including procedural learning, associative learning and inhibitory control of action, among other functions. The caudate is also one of the brain structures which compose the reward system and functions as part of the cortico–basal ganglia–thalamic loop.

Frontotemporal dementia (FTD), also called frontotemporal degeneration disease or frontotemporal neurocognitive disorder, encompasses several types of dementia involving the progressive degeneration of the brain's frontal and temporal lobes. FTD is the second most prevalent type of early onset dementia after Alzheimer's disease. Men and women appear to be equally affected. FTD generally presents as a behavioral or language disorder with gradual onset. Signs and symptoms tend to appear in late adulthood, typically between the ages of 45 and 65, although it can affect people younger or older than this. Currently, no cure or approved symptomatic treatment for FTD exists, although some off-label drugs and behavioral methods are prescribed.

Athetosis is a symptom characterized by slow, involuntary, convoluted, writhing movements of the fingers, hands, toes, and feet and in some cases, arms, legs, neck and tongue. Movements typical of athetosis are sometimes called athetoid movements. Lesions to the brain are most often the direct cause of the symptoms, particularly to the corpus striatum. This symptom does not occur alone and is often accompanied by the symptoms of cerebral palsy, as it is often a result of this physical disability. Treatments for athetosis are not very effective, and in most cases are simply aimed at managing the uncontrollable movement, rather than the cause itself.
In neurology, abulia, or aboulia, refers to a lack of will or initiative and can be seen as a disorder of diminished motivation (DDM). Abulia falls in the middle of the spectrum of diminished motivation, with apathy being less extreme and akinetic mutism being more extreme than abulia. The condition was originally considered to be a disorder of the will, and aboulic individuals are unable to act or make decisions independently; and their condition may range in severity from subtle to overwhelming. In the case of akinetic mutism, many patients describe that as soon as they "will" or attempt a movement, a "counter-will" or "resistance" rises up to meet them.
Hyperkinesia refers to an increase in muscular activity that can result in excessive abnormal movements, excessive normal movements, or a combination of both. Hyperkinesia is a state of excessive restlessness which is featured in a large variety of disorders that affect the ability to control motor movement, such as Huntington's disease. It is the opposite of hypokinesia, which refers to decreased bodily movement, as commonly manifested in Parkinson's disease.

Progressive supranuclear palsy (PSP) is a late-onset neurodegenerative disease involving the gradual deterioration and death of specific volumes of the brain. The condition leads to symptoms including loss of balance, slowing of movement, difficulty moving the eyes, and cognitive impairment. PSP may be mistaken for other types of neurodegeneration such as Parkinson's disease, frontotemporal dementia and Alzheimer's disease. The cause of the condition is uncertain, but involves the accumulation of tau protein within the brain. Medications such as levodopa and amantadine may be useful in some cases.

Hypokinesia is one of the classifications of movement disorders, and refers to decreased bodily movement. Hypokinesia is characterized by a partial or complete loss of muscle movement due to a disruption in the basal ganglia. Hypokinesia is a symptom of Parkinson's disease shown as muscle rigidity and an inability to produce movement. It is also associated with mental health disorders and prolonged inactivity due to illness, amongst other diseases.
Parkinson-plus syndromes (PPS) are a group of neurodegenerative diseases featuring the classical features of Parkinson's disease with additional features that distinguish them from simple idiopathic Parkinson's disease (PD). Parkinson-plus syndromes are either inherited genetically or occur sporadically.

Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia. CBD symptoms typically begin in people from 50 to 70 years of age, and typical survival before death is eight years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.

Tauopathies are a class of neurodegenerative diseases characterized by the aggregation of abnormal tau protein. Hyperphosphorylation of tau proteins causes them to dissociate from microtubules and form insoluble aggregates called neurofibrillary tangles. Various neuropathologic phenotypes have been described based on the anatomical regions and cell types involved as well as the unique tau isoforms making up these deposits. The designation 'primary tauopathy' is assigned to disorders where the predominant feature is the deposition of tau protein. Alternatively, diseases exhibiting tau pathologies attributed to different and varied underlying causes are termed 'secondary tauopathies'. Some neuropathologic phenotypes involving tau protein is Alzheimer's disease, Pick disease, Progressive supranuclear palsy, and corticobasal degeneration.
Pseudobulbar palsy is a medical condition characterized by the inability to control facial movements and caused by a variety of neurological disorders. Patients experience difficulty chewing and swallowing, have increased reflexes and spasticity in tongue and the bulbar region, and demonstrate slurred speech, sometimes also demonstrating uncontrolled emotional outbursts.

Frontotemporal dementia and parkinsonism linked to chromosome 17 (FTDP-17) is an autosomal dominant neurodegenerative tauopathy and Parkinson plus syndrome. FTDP-17 is caused by mutations in the MAPT gene located on the q arm of chromosome 17, and has three cardinal features: behavioral and personality changes, cognitive impairment, and motor symptoms. FTDP-17 was defined during the International Consensus Conference in Ann Arbor, Michigan, in 1996.

Basal ganglia disease is a group of physical problems that occur when the group of nuclei in the brain known as the basal ganglia fail to properly suppress unwanted movements or to properly prime upper motor neuron circuits to initiate motor function. Research indicates that increased output of the basal ganglia inhibits thalamocortical projection neurons. Proper activation or deactivation of these neurons is an integral component for proper movement. If something causes too much basal ganglia output, then the ventral anterior (VA) and ventral lateral (VL) thalamocortical projection neurons become too inhibited, and one cannot initiate voluntary movement. These disorders are known as hypokinetic disorders. However, a disorder leading to abnormally low output of the basal ganglia leads to reduced inhibition, and thus excitation, of the thalamocortical projection neurons which synapse onto the cortex. This situation leads to an inability to suppress unwanted movements. These disorders are known as hyperkinetic disorders.
The applause sign is a behavioural indicator, relevant to neurodegenerative conditions, characterised by a patient’s inability to execute the same number of hand claps as demonstrated by an examiner.

Athetoid cerebral palsy, or dyskinetic cerebral palsy, is a type of cerebral palsy primarily associated with damage, like other forms of CP, to the basal ganglia in the form of lesions that occur during brain development due to bilirubin encephalopathy and hypoxic–ischemic brain injury. Unlike spastic or ataxic cerebral palsies, ADCP is characterized by both hypertonia and hypotonia, due to the affected individual's inability to control muscle tone. Clinical diagnosis of ADCP typically occurs within 18 months of birth and is primarily based upon motor function and neuroimaging techniques. While there are no cures for ADCP, some drug therapies as well as speech, occupational therapy, and physical therapy have shown capacity for treating the symptoms.
In ophthalmology, apraxia of lid opening (ALO) is an inability to initiate voluntary opening of the eyelid following a period of eyelid closure, with normal function at other times. Manual lifting of the eyelid often resolves the problem and the lid is able to stay open.
Corticobasal syndrome (CBS) is a rare, progressive atypical Parkinsonism syndrome and is a tauopathy related to frontotemporal dementia. CBS is typically caused by the deposit of tau proteins forming in different areas of the brain.