An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention of such infections. They may either kill or inhibit the growth of bacteria. A limited number of antibiotics also possess antiprotozoal activity. Antibiotics are not effective against viruses such as the ones which cause the common cold or influenza; drugs which inhibit growth of viruses are termed antiviral drugs or antivirals rather than antibiotics. They are also not effective against fungi; drugs which inhibit growth of fungi are called antifungal drugs.

Antimicrobial resistance (AMR) occurs when microbes evolve mechanisms that protect them from the effects of antimicrobials. All classes of microbes can evolve resistance where the drugs are no longer effective. Fungi evolve antifungal resistance, viruses evolve antiviral resistance, protozoa evolve antiprotozoal resistance, and bacteria evolve antibiotic resistance. Together all of these come under the umbrella of antimicrobial resistance. Microbes resistant to multiple antimicrobials are called multidrug resistant (MDR) and are sometimes referred to as superbugs. Although antimicrobial resistance is a naturally occurring process, it is often the result of improper usage of the drugs and management of the infections.

Drug resistance is the reduction in effectiveness of a medication such as an antimicrobial or an antineoplastic in treating a disease or condition. The term is used in the context of resistance that pathogens or cancers have "acquired", that is, resistance has evolved. Antimicrobial resistance and antineoplastic resistance challenge clinical care and drive research. When an organism is resistant to more than one drug, it is said to be multidrug-resistant.

Klebsiella pneumoniae is a Gram-negative, non-motile, encapsulated, lactose-fermenting, facultative anaerobic, rod-shaped bacterium. It appears as a mucoid lactose fermenter on MacConkey agar.

Campylobacteriosis is among the most common infections caused by a bacterium in humans, often as a foodborne illness. It is caused by the Campylobacter bacterium, most commonly C. jejuni. It produces an inflammatory, sometimes bloody, diarrhea or dysentery syndrome, and usually cramps, fever and pain.

Amoxicillin/clavulanic acid, also known as co-amoxiclav or amox-clav, sold under the brand name Augmentin, among others, is an antibiotic medication used for the treatment of a number of bacterial infections. It is a combination consisting of amoxicillin, a β-lactam antibiotic, and potassium clavulanate, a β-lactamase inhibitor. It is specifically used for otitis media, streptococcal pharyngitis, pneumonia, cellulitis, urinary tract infections, and animal bites. It is taken by mouth or by injection into a vein.
Multiple drug resistance (MDR), multidrug resistance or multiresistance is antimicrobial resistance shown by a species of microorganism to at least one antimicrobial drug in three or more antimicrobial categories. Antimicrobial categories are classifications of antimicrobial agents based on their mode of action and specific to target organisms. The MDR types most threatening to public health are MDR bacteria that resist multiple antibiotics; other types include MDR viruses, parasites.
An anaerobic lagoon or manure lagoon is a man-made outdoor earthen basin filled with animal waste that undergoes anaerobic respiration as part of a system designed to manage and treat refuse created by concentrated animal feeding operations (CAFOs). Anaerobic lagoons are created from a manure slurry, which is washed out from underneath the animal pens and then piped into the lagoon. Sometimes the slurry is placed in an intermediate holding tank under or next to the barns before it is deposited in a lagoon. Once in the lagoon, the manure settles into two layers: a solid or sludge layer and a liquid layer. The manure then undergoes the process of anaerobic respiration, whereby the volatile organic compounds are converted into carbon dioxide and methane. Anaerobic lagoons are usually used to pretreat high strength industrial wastewaters and municipal wastewaters. This allows for preliminary sedimentation of suspended solids as a pretreatment process.

Medical microbiology, the large subset of microbiology that is applied to medicine, is a branch of medical science concerned with the prevention, diagnosis and treatment of infectious diseases. In addition, this field of science studies various clinical applications of microbes for the improvement of health. There are four kinds of microorganisms that cause infectious disease: bacteria, fungi, parasites and viruses, and one type of infectious protein called prion.
Enterococcus faecium is a Gram-positive, gamma-hemolytic or non-hemolytic bacterium in the genus Enterococcus. It can be commensal in the gastrointestinal tract of humans and animals, but it may also be pathogenic, causing diseases such as neonatal meningitis or endocarditis.

Antibiotic misuse, sometimes called antibiotic abuse or antibiotic overuse, refers to the misuse or overuse of antibiotics, with potentially serious effects on health. It is a contributing factor to the development of antibiotic resistance, including the creation of multidrug-resistant bacteria, informally called "super bugs": relatively harmless bacteria can develop resistance to multiple antibiotics and cause life-threatening infections.

The Animal Drug Availability Act 1996 (ADAA) is a United States federal law. President Clinton signed the ADAA into law in October 1996. While still obligated to public health concerns, the Act intends more rapid drug approval and medicated feed approval to assist the animal health industry.

Staphylococcus hyicus is a Gram-positive, facultatively anaerobic bacterium in the genus Staphylococcus. It consists of clustered cocci and forms white circular colonies when grown on blood agar. S. hyicus is a known animal pathogen. It causes disease in poultry, cattle, horses, and pigs. Most notably, it is the agent that causes porcine exudative epidermitis, also known as greasy pig disease, in piglets. S. hyicus is generally considered to not be zoonotic, however it has been shown to be able to cause bacteremia and sepsis in humans.
Antimicrobials destroy bacteria, viruses, fungi, algae, and other microbes. The cells of bacteria (prokaryotes), such as salmonella, differ from those of higher-level organisms (eukaryotes), such as fish. Antibiotics are chemicals designed to either kill or inhibit the growth of pathogenic bacteria while exploiting the differences between prokaryotes and eukaryotes in order to make them relatively harmless in higher-level organisms. Antibiotics are constructed to act in one of three ways: by disrupting cell membranes of bacteria, by impeding DNA or protein synthesis, or by hampering the activity of certain enzymes unique to bacteria.

Antibiotic use in livestock is the use of antibiotics for any purpose in the husbandry of livestock, which includes treatment when ill (therapeutic), treatment of a group of animals when at least one is diagnosed with clinical infection (metaphylaxis), and preventative treatment (prophylaxis). Antibiotics are an important tool to treat animal as well as human disease, safeguard animal health and welfare, and support food safety. However, used irresponsibly, this may lead to antibiotic resistance which may impact human, animal and environmental health.
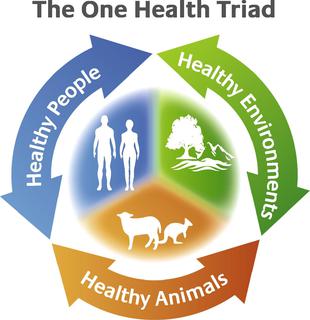
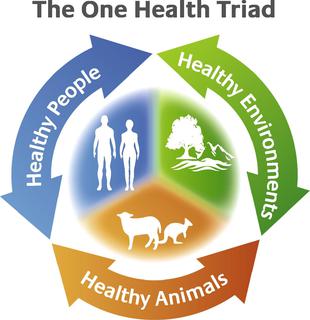
The concept of One Health is the unity of multiple practices that work together locally, nationally, and globally to help achieve optimal health for people, animals, and the environment. When the people, animals, and environment are put together they make up the One Health Triad .The One Health Triad shows how the health of people, animals, and the environment is linked to one another. With One Health being a worldwide concept, it makes it easier to advance health care in the 21st century. When this concept is used, and implied properly it can help protect and save the lives of both people, animals, and the environment in the present and future generations.
ESKAPE is an acronym comprising the scientific names of six highly virulent and antibiotic resistant bacterial pathogens including: Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp. The acronym is sometimes extended to ESKAPEE to include Escherichia coli. This group of Gram-positive and Gram-negative bacteria can evade or 'escape' commonly used antibiotics due to their increasing multi-drug resistance (MDR). As a result, throughout the world, they are the major cause of life-threatening nosocomial or hospital-acquired infections in immunocompromised and critically ill patients who are most at risk. P. aeruginosa and S. aureus are some of the most ubiquitous pathogens in biofilms found in healthcare. P. aeruginosa is a Gram-negative, rod-shaped bacterium, commonly found in the gut flora, soil, and water that can be spread directly or indirectly to patients in healthcare settings. The pathogen can also be spread in other locations through contamination, including surfaces, equipment, and hands. The opportunistic pathogen can cause hospitalized patients to have infections in the lungs, blood, urinary tract, and in other body regions after surgery. S. aureus is a Gram-positive, cocci-shaped bacterium, residing in the environment and on the skin and nose of many healthy individuals. The bacterium can cause skin and bone infections, pneumonia, and other types of potentially serious infections if it enters the body. S. aureus has also gained resistance to many antibiotic treatments, making healing difficult. Because of natural and unnatural selective pressures and factors, antibiotic resistance in bacteria usually emerges through genetic mutation or acquires antibiotic-resistant genes (ARGs) through horizontal gene transfer - a genetic exchange process by which antibiotic resistance can spread.
Antimicrobial resistance (AMR) directly kills about 1,600 people each year in Australia. This is a currently serious threat to both humans and animals in the country. Antimicrobial resistance occurs when a microorganism evolves and gains the ability to become more resistant or completely resistant to the medicine that was previously used to treat it. Drug-resistant bacteria are increasingly difficult to treat, requiring replacement or higher-dose drugs that may be more expensive or more toxic. Resistance can develop through one of the three mechanisms: natural resistant ability in some types of microorganisms, a mutation in genes or receiving the resistance from another species. Antibodies appear naturally due to random mutations, or more often after gradual accumulation over time, and because of abuse of antibiotics. Multidrug-resistance, or MDR, are the microorganisms that are resistant to many types of antimicrobials. "Superbugs" is the term also used for multidrug-resistant microbes, or totally drug-resistant (TDR).
Antibiotic use in the United States poultry farming industry is the controversial prophylactic use of antibiotics in the country's poultry farming industry. It differs from the common practice in Europe, where antibiotics for growth promotion were disallowed in the 1950s.