Universal precautions refers to the practice, in medicine, of avoiding contact with patients' bodily fluids, by means of the wearing of nonporous articles such as medical gloves, goggles, and face shields. The infection control techniques were essentially good hygiene habits, such as hand washing and the use of gloves and other barriers, the correct handling of hypodermic needles, scalpels, and aseptic techniques. Following the AIDS outbreak in the 1980s, the US CDC formally introduced them in 1985–88. Every patient was treated as if infected, and therefore precautions were taken to minimize risk.

Legionella is a genus of pathogenic gram-negative bacteria that includes the species L. pneumophila, causing legionellosis including a pneumonia-type illness called Legionnaires' disease and a mild flu-like illness called Pontiac fever.

Hand washing, also known as hand hygiene, is the act of cleaning one's hands with soap or handwash and water to remove viruses/bacteria/microorganisms, dirt, grease, or other harmful and unwanted substances stuck to the hands. Drying of the washed hands is part of the process as wet and moist hands are more easily recontaminated. If soap and water are unavailable, hand sanitizer that is at least 60% (v/v) alcohol in water can be used as long as hands are not visibly excessively dirty or greasy. Hand hygiene is central to preventing the spread of infectious diseases in home and everyday life settings.

Clostridioides difficile infection , also known as Clostridium difficile infection, is a symptomatic infection due to the spore-forming bacterium Clostridioides difficile. Symptoms include watery diarrhea, fever, nausea, and abdominal pain. It makes up about 20% of cases of antibiotic-associated diarrhea. Antibiotics can contribute to detrimental changes in gut microbiota; specifically, they decrease short-chain fatty acid absorption which results in osmotic, or watery, diarrhea. Complications may include pseudomembranous colitis, toxic megacolon, perforation of the colon, and sepsis.

A disinfectant is a chemical substance or compound used to inactivate or destroy microorganisms on inert surfaces. Disinfection does not necessarily kill all microorganisms, especially resistant bacterial spores; it is less effective than sterilization, which is an extreme physical or chemical process that kills all types of life. Disinfectants are generally distinguished from other antimicrobial agents such as antibiotics, which destroy microorganisms within the body, and antiseptics, which destroy microorganisms on living tissue. Disinfectants are also different from biocides—the latter are intended to destroy all forms of life, not just microorganisms. Disinfectants work by destroying the cell wall of microbes or interfering with their metabolism. It is also a form of decontamination, and can be defined as the process whereby physical or chemical methods are used to reduce the amount of pathogenic microorganisms on a surface.

Klebsiella pneumoniae is a Gram-negative, non-motile, encapsulated, lactose-fermenting, facultative anaerobic, rod-shaped bacterium. It appears as a mucoid lactose fermenter on MacConkey agar.

A hospital-acquired infection, also known as a nosocomial infection, is an infection that is acquired in a hospital or other healthcare facility. To emphasize both hospital and nonhospital settings, it is sometimes instead called a healthcare-associated infection. Such an infection can be acquired in hospital, nursing home, rehabilitation facility, outpatient clinic, diagnostic laboratory or other clinical settings. A number of dynamic processes can bring contamination into operating rooms and other areas within nosocomial settings. Infection is spread to the susceptible patient in the clinical setting by various means. Healthcare staff also spread infection, in addition to contaminated equipment, bed linens, or air droplets. The infection can originate from the outside environment, another infected patient, staff that may be infected, or in some cases, the source of the infection cannot be determined. In some cases the microorganism originates from the patient's own skin microbiota, becoming opportunistic after surgery or other procedures that compromise the protective skin barrier. Though the patient may have contracted the infection from their own skin, the infection is still considered nosocomial since it develops in the health care setting. Nosocomial infection tends to lack evidence that it was present when the patient entered the healthcare setting, thus meaning it was acquired post-admission.

A wet wipe, also known as a wet towel, moist towelette, disposable wipe, disinfecting wipe, or a baby wipe is a small to medium-sized moistened piece of plastic or cloth that either comes folded and individually wrapped for convenience or, in the case of dispensers, as a large roll with individual wipes that can be torn off. Wet wipes are used for cleaning purposes like personal hygiene and household cleaning; each is a separate product depending on the chemicals added and medical or office cleaning wipes are not intended for skin hygiene.
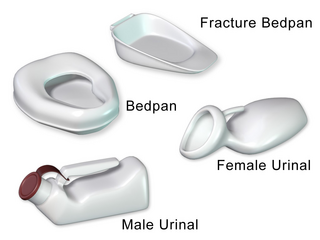
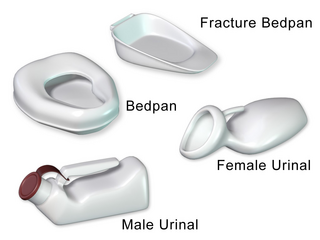
A bedpan or bed pan is a device used as a receptacle for the urine and/or feces of a person who is confined to a bed and therefore not able to use a toilet or chamber pot.
Infection prevention and control is the discipline concerned with preventing healthcare-associated infections; a practical rather than academic sub-discipline of epidemiology. In Northern Europe, infection prevention and control is expanded from healthcare into a component in public health, known as "infection protection". It is an essential part of the infrastructure of health care. Infection control and hospital epidemiology are akin to public health practice, practiced within the confines of a particular health-care delivery system rather than directed at society as a whole.

Hand sanitizer is a liquid, gel or foam generally used to kill many viruses/bacteria/microorganisms on the hands. In most settings, hand washing with soap and water is generally preferred. Hand sanitizer is less effective at killing certain kinds of germs, such as norovirus and Clostridium difficile, and unlike hand washing, it cannot physically remove harmful chemicals. People may incorrectly wipe off hand sanitizer before it has dried, and some are less effective because their alcohol concentrations are too low.
Any cause that reduces or increases reproductive success in a portion of a population potentially exerts evolutionary pressure, selective pressure or selection pressure, driving natural selection. It is a quantitative description of the amount of change occurring in processes investigated by evolutionary biology, but the formal concept is often extended to other areas of research.

In health care facilities, isolation represents one of several measures that can be taken to implement in infection control: the prevention of communicable diseases from being transmitted from a patient to other patients, health care workers, and visitors, or from outsiders to a particular patient. Various forms of isolation exist, in some of which contact procedures are modified, and others in which the patient is kept away from all other people. In a system devised, and periodically revised, by the U.S. Centers for Disease Control and Prevention (CDC), various levels of patient isolation comprise application of one or more formally described "precaution".
Transmission-based precautions are infection-control precautions in health care, in addition to the so-called "standard precautions". They are the latest routine infection prevention and control practices applied for patients who are known or suspected to be infected or colonized with infectious agents, including certain epidemiologically important pathogens, which require additional control measures to effectively prevent transmission. Universal precautions are also important to address as far as transmission-based precautions. Universal precautions is the practice of treating all bodily fluids as if it is infected with HIV, HBV, or other blood borne pathogens.
Carbapenem-resistant Enterobacteriaceae (CRE) or carbapenemase-producing Enterobacteriaceae (CPE) are Gram-negative bacteria that are resistant to the carbapenem class of antibiotics, considered the drugs of last resort for such infections. They are resistant because they produce an enzyme called a carbapenemase that disables the drug molecule. The resistance can vary from moderate to severe. Enterobacteriaceae are common commensals and infectious agents. Experts fear CRE as the new "superbug". The bacteria can kill up to half of patients who get bloodstream infections. Tom Frieden, former head of the Centers for Disease Control and Prevention has referred to CRE as "nightmare bacteria". Examples of enzymes found in certain types of CRE are KPC and NDM. KPC and NDM are enzymes that break down carbapenems and make them ineffective. Both of these enzymes, as well as the enzyme VIM have also been reported in Pseudomonas.

Prevention of viral hemorrhagic fever is similar for the different viruses. There are a number of different viral hemorrhagic fevers including Ebola virus disease, Lassa fever, Rift valley fever, Marburg virus disease, Crimean-Congo haemorrhagic fever (CCHF) and yellow fever. Lassa, Ebola, Marburg and CCHF can be spread by direct contact with the body fluids of those infected. Thus the content here covers the prevention of Ebola.

Hazard controls for COVID-19 in workplaces are the application of occupational safety and health methodologies for hazard controls to the prevention of COVID-19. Vaccination is the most effective way to protect against severe illness or death from COVID-19. Multiple layers of controls are recommended, including measures such as remote work and flextime, increased ventilation, personal protective equipment (PPE) and face coverings, social distancing, and enhanced cleaning programs.
A patient under investigation refers to a person who had been in close contact with a person with confirmed infection or/and may have been to place where there is an outbreak or superspreading event. This person exhibits the symptoms of the disease and is required to be tested, and undergo a quarantine or isolation while waiting for the laboratory results. It is a term used by health care workers in classifying patients during evaluation and testing in contact tracing in times of infectious disease outbreaks.
Accelerated hydrogen peroxide (AHP) is a trademark for solution of hydrogen peroxide whose antibacterial efficacy is enhanced by a surfactant and an organic acid. It is also a disinfectant/cleaning agent that stabilizes hydrogen peroxide so that it can be used for extended periods of time.