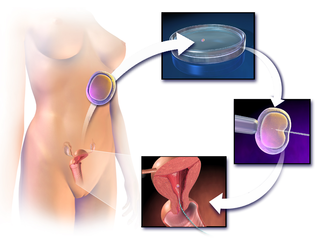
In vitro fertilisation (IVF) is a process of fertilisation where an egg is combined with sperm in vitro. The process involves monitoring and stimulating a woman's ovulatory process, removing an ovum or ova from their ovaries and letting a man's sperm fertilise them in a culture medium in a laboratory. After the fertilised egg (zygote) undergoes embryo culture for 2–6 days, it is transferred by catheter into the uterus, with the intention of establishing a successful pregnancy.
A multiple birth is the culmination of one multiple pregnancy, wherein the mother gives birth to two or more babies. A term most applicable to vertebrate species, multiple births occur in most kinds of mammals, with varying frequencies. Such births are often named according to the number of offspring, as in twins and triplets. In non-humans, the whole group may also be referred to as a litter, and multiple births may be more common than single births. Multiple births in humans are the exception and can be exceptionally rare in the largest mammals.

The Human Fertilisation and Embryology Authority (HFEA) is an executive non-departmental public body of the Department of Health and Social Care in the United Kingdom. It is a statutory body that regulates and inspects all clinics in the United Kingdom providing in vitro fertilisation (IVF), artificial insemination and the storage of human eggs, sperm or embryos. It also regulates human embryo research.
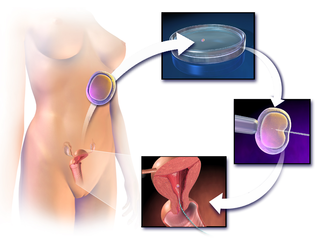
Assisted reproductive technology (ART) includes medical procedures used primarily to address infertility. This subject involves procedures such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), cryopreservation of gametes or embryos, and/or the use of fertility medication. When used to address infertility, ART may also be referred to as fertility treatment. ART mainly belongs to the field of reproductive endocrinology and infertility. Some forms of ART may be used with regard to fertile couples for genetic purpose. ART may also be used in surrogacy arrangements, although not all surrogacy arrangements involve ART. The existence of sterility will not always require ART to be the first option to consider, as there are occasions when its cause is a mild disorder that can be solved with more conventional treatments or with behaviors based on promoting health and reproductive habits.

Edwin Carlyle "Carl" Wood,, FRANZCOG was a prominent Australian gynaecologist, best known for his pioneering work developing and commercialising the technique of in-vitro fertilisation (IVF). He gained considerable international and national attention for his wide-ranging contributions in the field of women's health over a period of almost 50 years, although not all of it was positive given the controversial nature of many of his endeavours.
Emeritus Professor Sittampalam Shanmugaratnam, also known as Shan Ratnam, was a Singaporean obstetrician and gynaecologist.

Sir Robert Geoffrey Edwards was a British physiologist and pioneer in reproductive medicine, and in-vitro fertilisation (IVF) in particular. Along with obstetrician and gynaecologist Patrick Steptoe and nurse and embryologist Jean Purdy, Edwards successfully pioneered conception through IVF, which led to the birth of Louise Brown on 25 July 1978. They founded the first IVF programme for infertile patients and trained other scientists in their techniques. Edwards was the founding editor-in-chief of Human Reproduction in 1986. In 2010, he was awarded the Nobel Prize in Physiology or Medicine "for the development of in vitro fertilization".

Reproductive medicine is a branch of medicine concerning the male and female reproductive systems. It encompasses a variety of reproductive conditions, their prevention and assessment, as well as their subsequent treatment and prognosis.

Peter Robert Brinsden MBBS, MRCS, LRCP, FRCOG is known for the treatment of infertility in couples. From 1989 to 2006 he was the medical director of Bourn Hall Clinic in the UK, a leading centre for the treatment of fertility problems, and where about 6,000 babies have been conceived using IVF and other assisted conception treatments.

Bourn Hall Clinic in Bourn, Cambridgeshire, England, is a centre for the treatment of infertility. The original building, Bourn Hall, is about 400 years old. Since becoming a medical centre, it has been greatly extended.

The Human Fertilisation and Embryology Act 1990 is an Act of the Parliament of the United Kingdom. It created the Human Fertilisation and Embryology Authority which is in charge of human embryo research, along with monitoring and licensing fertility clinics in the United Kingdom.
Fertility tourism is the practice of traveling to another country or jurisdiction for fertility treatment, and may be regarded as a form of medical tourism. A person who can become pregnant is considered to have fertility issues if they are unable to have a clinical pregnancy after 12 months of unprotected intercourse. Infertility, or the inability to get pregnant, affects about 8-12% of couples looking to conceive or 186 million people globally. In some places, rates of infertility surpass the global average and can go up to 30% depending on the country. Areas with lack of resources, such as assisted reproductive technologies (ARTs), tend to correlate with the highest rates of infertility.
The Suleman octuplets are six male and two female children conceived via in vitro fertilization (IVF) and subsequently born to Nadya Suleman on January 26, 2009, in Bellflower, California. Residing in Lancaster, California, they are the first known octuplets to survive their infancy. The extremely controversial circumstances of their high-order multiple birth have led to debates in the field of assisted reproductive technology and an investigation by the Medical Board of California of the fertility specialist involved in the case.
Sperm donation is the provision by a man of his sperm with the intention that it be used in the artificial insemination or other "fertility treatment" of one or more women who are not his sexual partners in order that they may become pregnant by him. Where pregnancies go to full term, the sperm donor will be the biological father of every baby born from his donations. The man is known as a sperm donor and the sperm he provides is known as "donor sperm" because the intention is that the man will give up all legal rights to any child produced from his sperm, and will not be the legal father. Sperm donation may also be to known as "semen donation".
Mitochondrial replacement therapy (MRT), sometimes called mitochondrial donation, is the replacement of mitochondria in one or more cells to prevent or ameliorate disease. MRT originated as a special form of in vitro fertilisation in which some or all of the future baby's mitochondrial DNA (mtDNA) comes from a third party. This technique is used in cases when mothers carry genes for mitochondrial diseases. The therapy is approved for use in the United Kingdom. A second application is to use autologous mitochondria to replace mitochondria in damaged tissue to restore the tissue to a functional state. This has been used in clinical research in the United States to treat cardiac-compromised newborns.
Cryopreservation of embryos is the process of preserving an embryo at sub-zero temperatures, generally at an embryogenesis stage corresponding to pre-implantation, that is, from fertilisation to the blastocyst stage.
Partner-assisted reproduction, reception of oocytes from partner (ROPA), reciprocal IVF,shared motherhood, partner IVF or co-IVF is a method of family building that is used by couples who both possess female reproductive organs. The method uses in vitro fertilization (IVF), a method that means eggs are removed from the ovaries, fertilized in a laboratory, and then one or more of the resulting embryos are placed in the uterus to hopefully create a pregnancy. Reciprocal IVF differs from standard IVF in that two partners are involved: the eggs are taken from one partner, and the other partner carries the pregnancy. In this way, the process is mechanically identical to IVF with egg donation. Reciprocal IVF offers the highest chance for pregnancy and a lower chance of a multiple births.
The history of in vitro fertilisation (IVF) goes back more than half a century. In 1959 the first birth in a nonhuman mammal resulting from IVF occurred, and in 1978 the world's first baby conceived by IVF was born. As medicine advanced, IVF was transformed from natural research to a stimulated clinical treatment. There have been many refinements in the IVF process, and today millions of births have occurred with the help of IVF all over the world.
Simon Fishel is an English physiologist, biochemist and pioneering in vitro fertilisation (IVF) specialist.

Jean Marian Purdy was a British nurse and embryologist and a pioneer of fertility treatment. Purdy was responsible with Robert Edwards and Patrick Steptoe for developing in vitro fertilisation. Louise Joy Brown, the first test-tube baby, was born on 25 July 1978, and Purdy was the first to see the embryonic cells dividing. Edwards was awarded the 2010 Nobel Prize in Physiology or Medicine for his work on the development of in vitro fertilisation; however, because the Nobel Prize is not awarded posthumously, neither Purdy nor Steptoe were eligible for consideration. Purdy was a co-founder of the Bourn Hall Clinic but her role there and in the development of IVF was ignored for 30 years.