Related Research Articles

Anosmia, also known as smell blindness, is the loss of the ability to detect one or more smells. Anosmia may be temporary or permanent. It differs from hyposmia, which is a decreased sensitivity to some or all smells.

Dementia with Lewy bodies (DLB) is a type of dementia characterized by changes in sleep, behavior, cognition, movement, and regulation of automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive impairment interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described by Kenji Kosaka in 1976.

The olfactory system or sense of smell is the sensory system used for smelling (olfaction). Olfaction is one of the special senses, that have directly associated specific organs. Most mammals and reptiles have a main olfactory system and an accessory olfactory system. The main olfactory system detects airborne substances, while the accessory system senses fluid-phase stimuli.
Trimethylaminuria (TMAU), also known as fish odor syndrome or fish malodor syndrome, is a rare metabolic disorder that causes a defect in the normal production of an enzyme named flavin-containing monooxygenase 3 (FMO3). When FMO3 is not working correctly or if not enough enzyme is produced, the body loses the ability to properly convert the fishy-smelling chemical trimethylamine (TMA) from precursor compounds in food digestion into trimethylamine oxide (TMAO), through a process called N-oxidation.
Parosmia is a dysfunctional smell detection characterized by the inability of the brain to correctly identify an odor's "natural" smell. Instead, the natural odor is usually transformed into an unpleasant aroma, typically a "burned", "rotting", "fecal", or "chemical" smell. There can also be rare instances of a pleasant odor called euosmia. The condition was rare and little-researched until it became relatively more widespread since 2020 as a side effect of COVID-19.
Richard L. Doty is a professor of psychology and otorhinolaryngology at the University of Pennsylvania. He has also been the director of the University of Pennsylvania's Smell and Taste Center since 1980.

Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia. CBD symptoms typically begin in people from 50 to 70 years of age, and typical survival before death is eight years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.
Memory disorders are the result of damage to neuroanatomical structures that hinders the storage, retention and recollection of memories. Memory disorders can be progressive, including Alzheimer's disease, or they can be immediate including disorders resulting from head injury.

The olfactory tubercle (OT), also known as the tuberculum olfactorium, is a multi-sensory processing center that is contained within the olfactory cortex and ventral striatum and plays a role in reward cognition. The OT has also been shown to play a role in locomotor and attentional behaviors, particularly in relation to social and sensory responsiveness, and it may be necessary for behavioral flexibility. The OT is interconnected with numerous brain regions, especially the sensory, arousal, and reward centers, thus making it a potentially critical interface between processing of sensory information and the subsequent behavioral responses.
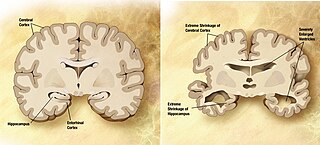
A neurodegenerative disease is caused by the progressive loss of structure or function of neurons, in the process known as neurodegeneration. Such neuronal damage may ultimately involve cell death. Neurodegenerative diseases include amyotrophic lateral sclerosis, multiple sclerosis, Parkinson's disease, Alzheimer's disease, Huntington's disease, multiple system atrophy, tauopathies, and prion diseases. Neurodegeneration can be found in the brain at many different levels of neuronal circuitry, ranging from molecular to systemic. Because there is no known way to reverse the progressive degeneration of neurons, these diseases are considered to be incurable; however research has shown that the two major contributing factors to neurodegeneration are oxidative stress and inflammation. Biomedical research has revealed many similarities between these diseases at the subcellular level, including atypical protein assemblies and induced cell death. These similarities suggest that therapeutic advances against one neurodegenerative disease might ameliorate other diseases as well.
Phantosmia, also called an olfactory hallucination or a phantom odor, is smelling an odor that is not actually there. This is intrinsically suspicious as the formal evaluation and detection of relatively low levels of odour particles is itself a very tricky task in air epistemology. It can occur in one nostril or both. Unpleasant phantosmia, cacosmia, is more common and is often described as smelling something that is burned, foul, spoiled, or rotten. Experiencing occasional phantom smells is normal and usually goes away on its own in time. When hallucinations of this type do not seem to go away or when they keep coming back, it can be very upsetting and can disrupt an individual's quality of life.
Hyposmia, or microsmia, is a reduced ability to smell and to detect odors. A related condition is anosmia, in which no odors can be detected. Some of the causes of olfaction problems are allergies, nasal polyps, viral infections and head trauma. In 2012 an estimated 9.8 million people aged 40 and older in the United States had hyposmia and an additional 3.4 million had anosmia/severe hyposmia.
Dysosmia is a disorder described as any qualitative alteration or distortion of the perception of smell. Qualitative alterations differ from quantitative alterations, which include anosmia and hyposmia. Dysosmia can be classified as either parosmia or phantosmia. Parosmia is a distortion in the perception of an odorant. Odorants smell different from what one remembers. Phantosmia is the perception of an odor when no odorant is present. The cause of dysosmia still remains a theory. It is typically considered a neurological disorder and clinical associations with the disorder have been made. Most cases are described as idiopathic and the main antecedents related to parosmia are URTIs, head trauma, and nasal and paranasal sinus disease. Dysosmia tends to go away on its own but there are options for treatment for patients that want immediate relief.

The sense of smell, or olfaction, is the special sense through which smells are perceived. The sense of smell has many functions, including detecting desirable foods, hazards, and pheromones, and plays a role in taste.
Olfactory memory refers to the recollection of odors. Studies have found various characteristics of common memories of odor memory including persistence and high resistance to interference. Explicit memory is typically the form focused on in the studies of olfactory memory, though implicit forms of memory certainly supply distinct contributions to the understanding of odors and memories of them. Research has demonstrated that the changes to the olfactory bulb and main olfactory system following birth are extremely important and influential for maternal behavior. Mammalian olfactory cues play an important role in the coordination of the mother infant bond, and the following normal development of the offspring. Maternal breast odors are individually distinctive, and provide a basis for recognition of the mother by her offspring.

Parkinson's disease (PD), or simply Parkinson's, is a chronic degenerative disorder of the central nervous system that affects both the motor system and non-motor systems. The symptoms usually emerge slowly, and as the disease progresses, non-motor symptoms become more common. Early symptoms are tremor, rigidity, slowness of movement, and difficulty with walking. Problems may also arise with cognition, behaviour, sleep, and sensory systems. Parkinson's disease dementia is common in advanced stages.
Signs and symptoms of Parkinson's disease are varied. Parkinson's disease affects movement, producing motor symptoms. Non-motor symptoms, which include dysautonomia, cognitive and neurobehavioral problems, and sensory and sleep difficulties, are also common. When other diseases mimic Parkinson's disease, they are categorized as parkinsonism.

A cholinergic neuron is a nerve cell which mainly uses the neurotransmitter acetylcholine (ACh) to send its messages. Many neurological systems are cholinergic. Cholinergic neurons provide the primary source of acetylcholine to the cerebral cortex, and promote cortical activation during both wakefulness and rapid eye movement sleep. The cholinergic system of neurons has been a main focus of research in aging and neural degradation, specifically as it relates to Alzheimer's disease. The dysfunction and loss of basal forebrain cholinergic neurons and their cortical projections are among the earliest pathological events in Alzheimer's disease.
The peanut butter test is a diagnostic test which aims to detect Alzheimer's disease by measuring subjects' ability to smell peanut butter through each nostril. The original study, published in the Journal of the Neurological Sciences in October 2013, involves measuring the ability of people to smell peanut butter held close to their nose. The researchers believe that people with Alzheimer's were not able to smell the peanut butter as well through their left nostril as their right one.
Smell training or olfactory training is the act of regularly sniffing or exposing oneself to robust aromas with the intention of regaining a sense of smell. The stimulating smells used are often selected from major smell categories, such as aromatic, flowery, fruity, and resinous. Using strong scents, the patient is asked to sniff each different smell for a minimum of 20 seconds, no less than two times per day, for three to six months or more. It is used as a rehabilitative therapy to help people who have anosmia or post-viral olfactory dysfunction, a symptom of COVID-19. It was considered a promising experimental treatment in a 2017 meta-analysis.
References
- 1 2 Doty, RL; Frye RE; Agrawal U (1989). "Internal consistency reliability of the fractionated and whole University of Pennsylvania Smell Identification Test". Perception & Psychophysics. 45 (5): 381–384. doi: 10.3758/bf03210709 . PMID 2726398.
- ↑ Doty, RL; Shaman P; Applebaum SL; et al. (1984). "Smell Identification ability: changes with age". Science. 226 (4681): 1441–1443. Bibcode:1984Sci...226.1441D. doi:10.1126/science.6505700. PMID 6505700.
- ↑ Doty, R (2007). "Office procedures for quantitative assessment of olfactory function". American Journal of Rhinology. 24 (4): 460–473. doi:10.2500/ajr.2007.21.3043. PMID 17882917. S2CID 26631047.
- ↑ Ogihara, H (2011). "Applicability of the cross-culturally modified University of Pennsylvania Smell Identification Test in a Japanese population". Allergy. 6 (25): 404–410. doi:10.2500/ajra.2011.25.3658. PMID 22185745. S2CID 21289611.
- ↑ Doty, RL (1995). The Smell Identification Test Administration Manual. Sensonics Inc. pp. 1–57.
- ↑ Doty, RL; Marcus A; Lee WW. (1996). "Development of the 12-item cross-cultural smell identification test (CC-SIT)". Laryngoscope. 106 (3): 353–356. doi:10.1097/00005537-199603000-00021. PMID 8614203. S2CID 24605655.
- ↑ Nordin, S; Bramerson A; Liden E; et al. (1999). "The Scandinavian Odor-Identification Test: Development, reliability, validity, and normative data". Acta Otolaryngol. 118 (2): 226–234. doi:10.1080/00016489850154946. PMID 9583791.
- ↑ Liu, HC; Wang SJ; Lin KP; et al. (1995). "Performance on a smell screening test (the MODSIT): A study of 510 predominantly illiterate Chinese subjects". Physiological Behavior. 58 (6): 1251–1255. doi:10.1016/0031-9384(95)02042-x. PMID 8623028. S2CID 31456625.
- ↑ Ship, JA; Weiffenback JM (1993). "Age, gender, medical treatment and medication effects on smell identification". Journal of Gerontology. 48 (1): 26–32. doi:10.1093/geronj/48.1.m26. PMID 8418141.
- ↑ Roalf, DR; Turetsky BI; Owzar K; et al. (2006). "Unifhinal Olfactory function in schizophrenia patients and first degree relatives". Journal of Neuropsychiatry and Clinical Neurosciences. 18. 18 (3): 389–396. doi:10.1176/jnp.2006.18.3.389. PMID 16963589.
- ↑ Segal, NL; Topolski TD; Wilson SM; et al. (1995). "Twin analysis of odor identification and perception". Physiological Behavior. 57 (3): 605–609. doi:10.1016/0031-9384(94)00328-3. PMID 7538679. S2CID 25897237.
- ↑ Frye, RE; Schwartz BS; Doty RL (1990). "Dose-related effects of cigarette smoking on olfactory function". JAMA. 263 (9): 1233–1236. doi:10.1001/jama.263.9.1233. PMID 2304239.
- ↑ Hirsch, AR; Zavala G. (1999). "Long-term effects on the olfactory system of exposure to hydrogen sulphide". Occupational and Environmental Medicine. 56 (4): 284–287. doi:10.1136/oem.56.4.284. PMC 1757725 . PMID 10450248.
- ↑ Bylsma, F.; Moberg, P.; Doty, R.; Brandt, J. (1997). "Odor identification in Huntington's disease patients and asymptomatic gene carriers". The Journal of Neuropsychiatry and Clinical Neurosciences. 9 (4): 598–600. doi:10.1176/jnp.9.4.598. PMID 9447504.
- ↑ Keshavan, M.; Montrose, D.; Diwadkar, V.; Sweeney, J. (2009). "Olfactory identification in your relatives at risk for schizophrenia". Acta Neuropsychiatrica. 21 (3): 121–124. doi:10.1111/j.1601-5215.2009.00390.x. PMC 3169013 . PMID 21909191.
- ↑ Amoore, JE (1967). "Specific anosmia: A clue to the olfactory code". Nature. 214 (5093): 1095–1098. Bibcode:1967Natur.214.1095A. doi:10.1038/2141095a0. PMID 4861233. S2CID 4222453.
- ↑ Yousem, D.; Geckle, R.; Bilker, W.; Kroger, H.; Doty, R. (1999). "Posttraumatic smell loss: relationship of psychophysical tests and volumes of the olfactory bulbs and tracts and the temporal lobes". Academic Radiology. 5. 6 (5): 264–272. doi: 10.1016/s1076-6332(99)80449-8 . PMID 10228615.
- ↑ Boldrey, E.; Naffziger, H.; rnstein, L. (1950). "Signs and symptoms of supratentorial brain tumors in childhood". The Journal of Pediatrics. 37 (4): 463–468. doi:10.1016/s0022-3476(50)80255-x. PMID 14779246.
- ↑ Vance, D. (2007). "Olfactory and psychomotor symptoms in HIV and aging: potential precursors to cognitive loss". Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 13. 13 (10): SC1-3. PMID 17901863.
- ↑ Hawkes, C.; Shephard B; Kobal G. (August 1997). "Assessment of Olfaction in multiple sclerosis: evidence of dysfunction by olfactory evoked response and identification tests". Journal of Neurology, Neurosurgery, and Psychiatry. 63 (2): 145–151. doi:10.1136/jnnp.63.2.145. PMC 2169670 . PMID 9285449.
- ↑ Lange, R; Donathan, C.; Hughes, L. (2002). "Assessing olfactory abilities with the University of Pennsylvania smell identification test: a Rasch scaling approach". Journal of Alzheimer's Disease. 4. 4 (2): 77–91. doi:10.3233/JAD-2002-4202. PMID 12214131.
- ↑ Wang, J.; et al. (2010). "Olfactory deficit detected by fMRI in early Alzheimer's disease". Brain Research. 1357: 184–194. doi:10.1016/j.brainres.2010.08.018. PMC 3515873 . PMID 20709038.
- ↑ Velaugudhan, L; Pritchard M; Powell J; Proitsi P; Lovestone S (July 2013). "Smell identification function as a severity and progression marker in Alzheimer's disease". International Psychogeriatrics. 25 (7): 1157–1166. doi:10.1017/s1041610213000446. PMID 23597130. S2CID 35876259.
- 1 2 Doty, RL (June 2012). "Olfaction in Parkinson's disease and related disorders". Neurobiology of Disease. 3. 46 (3): 527–552. doi:10.1016/j.nbd.2011.10.026. PMC 3429117 . PMID 22192366.