Interstitial cystitis (IC), a type of bladder pain syndrome (BPS), is chronic pain in the bladder and pelvic floor of unknown cause. It is the urologic chronic pelvic pain syndrome of women. Symptoms include feeling the need to urinate right away, needing to urinate often, and pain with sex. IC/BPS is associated with depression and lower quality of life. Many of those affected also have irritable bowel syndrome and fibromyalgia.

Bladder cancer is any of several types of cancer arising from the tissues of the urinary bladder. Symptoms include blood in the urine, pain with urination, and low back pain. It is caused when epithelial cells that line the bladder become malignant.

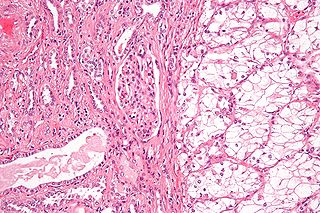
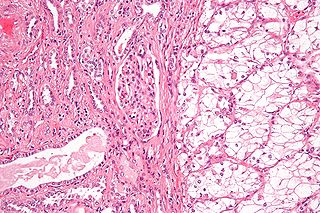
A Krukenberg tumor refers to a malignancy in the ovary that metastasized from a primary site, classically the gastrointestinal tract, although it can arise in other tissues such as the breast. Gastric adenocarcinoma, especially at the pylorus, is the most common source. Krukenberg tumors are often found in both ovaries, consistent with its metastatic nature.
Renal cell carcinoma (RCC) is a kidney cancer that originates in the lining of the proximal convoluted tubule, a part of the very small tubes in the kidney that transport primary urine. RCC is the most common type of kidney cancer in adults, responsible for approximately 90–95% of cases. RCC occurrence shows a male predominance over women with a ratio of 1.5:1. RCC most commonly occurs between 6th and 7th decade of life.
Glomerulation refers to bladder hemorrhages which are thought to be associated with some types of interstitial cystitis (IC).

Bladder exstrophy is a congenital anomaly that exists along the spectrum of the exstrophy-epispadias complex, and most notably involves protrusion of the urinary bladder through a defect in the abdominal wall. Its presentation is variable, often including abnormalities of the bony pelvis, pelvic floor, and genitalia. The underlying embryologic mechanism leading to bladder exstrophy is unknown, though it is thought to be in part due to failed reinforcement of the cloacal membrane by underlying mesoderm. Exstrophy means the inversion of a hollow organ.

Prostatectomy is the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

The sentinel lymph node is the hypothetical first lymph node or group of nodes draining a cancer. In case of established cancerous dissemination it is postulated that the sentinel lymph nodes are the target organs primarily reached by metastasizing cancer cells from the tumor.

Transitional cell carcinoma, also called urothelial carcinoma, is a type of cancer that typically occurs in the urinary system. It is the most common type of bladder cancer and cancer of the ureter, urethra, and urachus. It accounts for 95% of bladder cancer cases.

Urethral cancer is a rare cancer originating from the urethra. The disease has been classified by the TNM staging system and the World Health Organization.
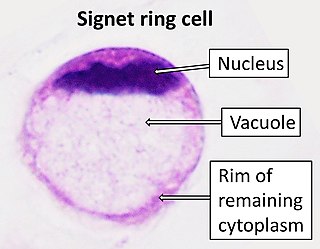
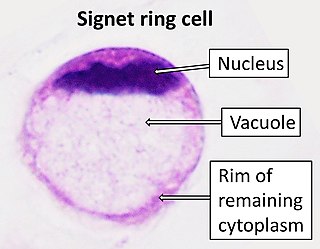
Signet ring cell carcinoma (SRCC) is a rare form of highly malignant adenocarcinoma that produces mucin. It is an epithelial malignancy characterized by the histologic appearance of signet ring cells.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
Lower urinary tract symptoms (LUTS) refer to a group of clinical symptoms involving the bladder, urinary sphincter, urethra and, in men, the prostate. The term is more commonly applied to men—over 40% of older men are affected—but lower urinary tract symptoms also affect women. The condition is also termed prostatism in men, but LUTS is preferred.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Douglas S. Scherr, M.D. is an American surgeon and specialist in Urologic Oncology. He is currently the Clinical Director of Urologic Oncology at Weill Cornell Medicine. He also holds an appointment at the Rockefeller University as a Visiting Associate Physician. Scherr was the first physician at Cornell to perform a robotic prostatectomy as well as a robotic cystectomy.

Papillary urothelial neoplasm of low malignant potential (PUNLMP) is an exophytic, (microscopically) nipple-shaped pre-malignant growth of the lining of the upper genitourinary tract, which includes the renal pelvis, ureters, urinary bladder and part of the urethra.

Combined small cell lung carcinoma is a form of multiphasic lung cancer that is diagnosed by a pathologist when a malignant tumor, arising from transformed cells originating in lung tissue, contains a component of;small cell lung carcinoma (SCLC), admixed with one components of any histological variant of non-small cell lung carcinoma (NSCLC) in any relative proportion.
Acinar adenocarcinoma is a histological subtype of gland-forming cancer that is diagnosed when cuboidal and/or columnar shaped malignant cells in the neoplastic tissue form acini and tubules. It is a common form of cancer occurring in the lung and prostate gland.

A pancreatic tumor is an abnormal growth in the pancreas. In adults, almost 90% are pancreatic cancer and a few are benign. Pancreatic tumors are rare in children.
Gaetano Ciancio is an Italian American surgeon at the University of Miami who specializes in kidney transplant. He is the chief medical and academic officer of the Miami Transplant Institute and the director of its Kidney & Kidney-Pancreas Programs. His most significant contributions to medicine are related to surgically treating kidney cancer once it has spread to the inferior vena cava and in optimizing the immunosuppression protocol after kidney transplant.