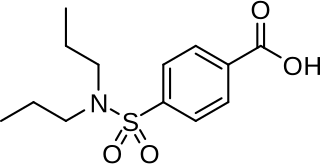
Furosemide is a loop diuretic medication used to treat edema due to heart failure, liver scarring, or kidney disease. It has had many trade names including Discoid, Frusemide, Lasix and Uremide. Furosemide may also be used for the treatment of high blood pressure. It can be taken intravenously or orally. When given intravenously, furosemide typically takes effect within five minutes; when taken orally, it typically metabolizes within an hour.
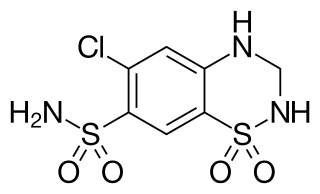
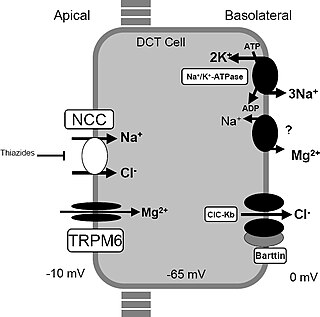
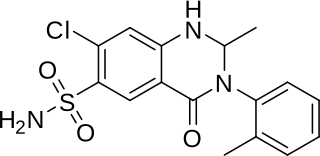
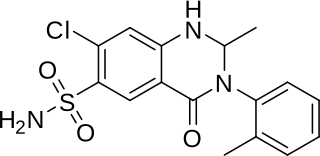
Hydrochlorothiazide, sold under the brand name Hydrodiuril among others, is a diuretic medication used to treat hypertension and swelling due to fluid build-up. Other uses include treating diabetes insipidus and renal tubular acidosis and to decrease the risk of kidney stones in those with a high calcium level in the urine. Hydrochlorothiazide is taken by mouth and may be combined with other blood pressure medications as a single pill to increase effectiveness. Hydrochlorothiazide is a thiazide medication which inhibits reabsorption of sodium and chloride ions from the distal convoluted tubules of the kidneys, causing a natriuresis. This initially increases urine volume and lowers blood volume. It is believed to reduce peripheral vascular resistance.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.
Atenolol is a beta blocker medication primarily used to treat high blood pressure and heart-associated chest pain. Atenolol, however, does not seem to improve mortality in those with high blood pressure. Other uses include the prevention of migraines and treatment of certain irregular heart beats. It is taken orally or by intravenous injection. It can also be used with other blood pressure medications.

Indapamide is a thiazide-like diuretic drug used in the treatment of hypertension, as well as decompensated heart failure. Combination preparations with perindopril are available. The thiazide-like diuretics reduce risk of major cardiovascular events and heart failure in hypertensive patients compared with hydrochlorothiazide with a comparable incidence of adverse events. Both thiazide diuretics and thiazide-like diuretics are effective in reducing risk of stroke. Both drug classes appear to have comparable rates of adverse effects as other antihypertensives such as angiotensin II receptor blockers and dihydropyridine calcium channel blockers and lesser prevalence of side-effects when compared to ACE-inhibitors and non-dihydropyridine calcium channel blockers.

Loop diuretics are diuretics that act on the Na-K-Cl cotransporter along the thick ascending limb of the loop of Henle in nephrons of the kidneys. They are primarily used in medicine to treat hypertension and edema often due to congestive heart failure or chronic kidney disease. While thiazide diuretics are more effective in patients with normal kidney function, loop diuretics are more effective in patients with impaired kidney function.

Amiloride, sold under the trade name Midamor among others, is a medication typically used with other medications to treat high blood pressure or swelling due to heart failure or cirrhosis of the liver. Amiloride is classified as a potassium-sparing diuretic. Amiloride is often used together with another diuretic, such as a thiazide or loop diuretic. It is taken by mouth. Onset of action is about two hours and it lasts for about a day.

Chlortalidone, also known as chlorthalidone, is a thiazide-like diuretic drug used to treat high blood pressure, swelling, diabetes insipidus, and renal tubular acidosis. Because chlortalidone is effective in most patients with high blood pressure, it is considered a preferred initial treatment. It is also used to prevent calcium-based kidney stones. It is taken by mouth. Effects generally begin within three hours and last for up to three days. Long-term treatment with chlortalidone is more effective than hydrochlorothiazide for prevention of heart attack or stroke.

Bendroflumethiazide, formerly bendrofluazide, trade name Aprinox, is a thiazide diuretic used to treat hypertension.

Thiazide refers to both a class of sulfur-containing organic molecules and a class of diuretics based on the chemical structure of benzothiadiazine. The thiazide drug class was discovered and developed at Merck and Co. in the 1950s. The first approved drug of this class, chlorothiazide, was marketed under the trade name Diuril beginning in 1958. In most countries, thiazides are the least expensive antihypertensive drugs available.
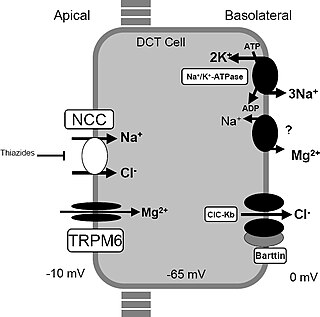
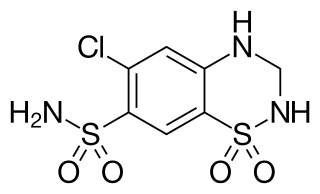
Gitelman syndrome (GS) is an autosomal recessive kidney tubule disorder characterized by low blood levels of potassium and magnesium, decreased excretion of calcium in the urine, and elevated blood pH. It is the most frequent hereditary salt-losing tubulopathy. Gitelman syndrome is caused by disease-causing variants on both alleles of the SLC12A3 gene. The SLC12A3 gene encodes the thiazide-sensitive sodium-chloride cotransporter, which can be found in the distal convoluted tubule of the kidney.

Potassium-sparing diuretics refers to drugs that cause diuresis without causing potassium loss in the urine. They are typically used as an adjunct in management of hypertension, cirrhosis, and congestive heart failure. The steroidal aldosterone antagonists can also be used for treatment of primary hyperaldosteronism. Spironolactone, a steroidal aldosterone antagonist, is also used in management of female hirsutism and acne from PCOS or other causes.
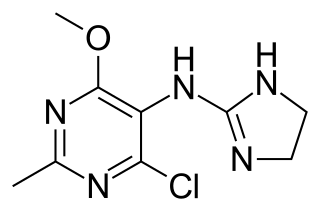
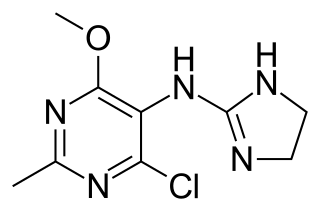
Moxonidine (INN) is a new-generation alpha-2/imidazoline receptor agonist antihypertensive drug licensed for the treatment of mild to moderate essential hypertension. It may have a role when thiazides, beta-blockers, ACE inhibitors, and calcium channel blockers are not appropriate or have failed to control blood pressure. In addition, it demonstrates favourable effects on parameters of the insulin resistance syndrome, apparently independent of blood pressure reduction. It is also a growth hormone releaser. It is manufactured by Solvay Pharmaceuticals under the brand name Physiotens and Moxon.
Probenecid, also sold under the brand name Probalan, is a medication that increases uric acid excretion in the urine. It is primarily used in treating gout and hyperuricemia.
Metolazone is a thiazide-like diuretic marketed under the brand names Zytanix, Metoz, Zaroxolyn, and Mykrox. It is primarily used to treat congestive heart failure and high blood pressure. Metolazone indirectly decreases the amount of water reabsorbed into the bloodstream by the kidney, so that blood volume decreases and urine volume increases. This lowers blood pressure and prevents excess fluid accumulation in heart failure. Metolazone is sometimes used together with loop diuretics such as furosemide or bumetanide, but these highly effective combinations can lead to dehydration and electrolyte abnormalities.

Bartter syndrome (BS) is a rare inherited disease characterised by a defect in the thick ascending limb of the loop of Henle, which results in low potassium levels (hypokalemia), increased blood pH (alkalosis), and normal to low blood pressure. There are two types of Bartter syndrome: neonatal and classic. A closely associated disorder, Gitelman syndrome, is milder than both subtypes of Bartter syndrome.

Perindopril is a medication used to treat high blood pressure, heart failure, or stable coronary artery disease.

Perindopril/indapamide is a combination medication which contains perindopril and indapamide both of which are used for the treatment of essential hypertension.

Dent's disease is a rare X-linked recessive inherited condition that affects the proximal renal tubules of the kidney. It is one cause of Fanconi syndrome, and is characterized by tubular proteinuria, excess calcium in the urine, formation of calcium kidney stones, nephrocalcinosis, and chronic kidney failure.

A diuretic is any substance that promotes diuresis, the increased production of urine. This includes forced diuresis. A diuretic tablet is sometimes colloquially called a water tablet. There are several categories of diuretics. All diuretics increase the excretion of water from the body, through the kidneys. There exist several classes of diuretic, and each works in a distinct way. Alternatively, an antidiuretic, such as vasopressin, is an agent or drug which reduces the excretion of water in urine.