Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine (TCM) in which thin needles are inserted into the body. Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientific knowledge, and it has been characterized as quackery.

Traditional Chinese medicine (TCM) is an alternative medical practice drawn from traditional medicine in China. It has been described as pseudoscientific, with the majority of its treatments having no known mechanism of action.

Acupressure is an alternative medicine technique often used in conjunction with acupuncture or reflexology. It is based on the concept of life energy, which flows through "meridians" in the body. In treatment, physical pressure is applied to acupuncture points, or ashi trigger points, with the aim of clearing blockages in these meridians. Pressure may be applied by hand, by elbow, or with various devices.

Moxibustion is a traditional Chinese medicine therapy which consists of burning dried mugwort on particular points on the body. It plays an important role in the traditional medical systems of China, Japan, Korea, Vietnam, and Mongolia. Suppliers usually age the mugwort and grind it up to a fluff; practitioners burn the fluff or process it further into a cigar-shaped stick. They can use it indirectly, with acupuncture needles, or burn it on the patient's skin.
The zangfu organs are functional entities stipulated by traditional Chinese medicine (TCM). These classifications are not based in physiology or science. They constitute the technological centrepiece of TCM's general concept of how the human body works. The term zang refers to the organs considered to be "solid" yin in nature – Heart, Liver, Spleen, Lung, Kidney – while fu refers to the "hollow" yang organs – Small Intestine, Large Intestine, Gall Bladder, Urinary Bladder, Stomach and San Jiao.

Tui na is form of alternative medicine similar to shiatsu. As a branch of traditional Chinese medicine, it is often used in conjunction with acupuncture, moxibustion, fire cupping, Chinese herbalism, tai chi or other Chinese internal martial arts, and qigong.

Cupping therapy is a form of pseudoscience in which a local suction is created on the skin with the application of heated cups. As alternative medicine it is practiced primarily in Asia but also in Eastern Europe, the Middle East, and Latin America. Cupping has been characterized as a pseudoscience and its practice as quackery.
The Liver is one of the zàng organs stipulated by traditional Chinese medicine (TCM). It is a functionally defined entity and not equivalent to the anatomical organ of the same name.
The Spleen is one of the zàng organs stipulated by traditional Chinese medicine (TCM). It is a functionally defined entity and not equivalent to the anatomical organ of the same name.

Traditional Korean medicine refers to the forms of traditional medicine practiced in Korea.

Myofascial trigger points (MTrPs), also known as trigger points, are described as hyperirritable spots in the skeletal muscle. They are associated with palpable nodules in taut bands of muscle fibers. They are a topic of ongoing controversy, as there is limited data to inform a scientific understanding of the phenomenon. Accordingly, a formal acceptance of myofascial "knots" as an identifiable source of pain is more common among bodyworkers, physical therapists, chiropractors, and osteopathic practitioners. Nonetheless, the concept of trigger points provides a framework which may be used to help address certain musculoskeletal pain.
Dry needling, also known as trigger point dry needling and intramuscular stimulation, is a treatment technique used by various healthcare practitioners, including physical therapists, physicians, and chiropractors, among others. Acupuncturists usually maintain that dry needling is adapted from acupuncture, but others consider dry needling as a variation of trigger point injections. It involves the use of either solid filiform needles or hollow-core hypodermic needles for therapy of muscle pain, including pain related to myofascial pain syndrome. Dry needling is mainly used to treat myofascial trigger points, but it is also used to target connective tissue, neural ailments, and muscular ailments. The American Physical Therapy Association defines dry needling as a technique used to treat dysfunction of skeletal muscle and connective tissue, minimize pain, and improve or regulate structural or functional damage.
Xiao Yao Wan, also known as Free and Easy Wanderer, is a Chinese classic herbal formula. It is commonly made into Chinese patent medicine.
The American Academy of Acupuncture and Oriental Medicine (AAAOM) was established in 1997 in response to the encouragement of staff and faculty at the Shandong University of Traditional Chinese Medicine in Jinan, China. Classes began in 1999 in a small collection of rooms in the University Technology Center building in Dinkytown, near the University of Minnesota, United States. At that time there were about 40 full and part-time students and the school consisted of two class rooms, four treatment rooms and a small series of adjoining offices which served as reception, administration office and pharmacy. The one clinic consultation room was little more than a closet with a window and enough space for a desk and two chairs.
Regulation of acupuncture is done by governmental bodies to ensure safe practice.
Cannabinoid hyperemesis syndrome (CHS) is recurrent nausea, vomiting, and cramping abdominal pain that can occur due to prolonged, high-dose cannabis use. These symptoms may be relieved temporarily by taking a hot shower or bath. Complications are related to persistent vomiting and dehydration which may lead to kidney failure and electrolyte problems.
Zouhuorumo, also known as qigong deviation, is a Chinese-culture concept traditionally used to indicate that something has gone wrong in spiritual or martial arts training. The qigong community uses this term to describe a physiological or psychological disorder believed to result during or after qigong practice, due to "improper practice" of qigong and other self-cultivation techniques. The concept was highlighted in the social and political context of mass popularization of qigong in China. The Buddhist or Taoist community also uses this term when referring to people who practice esoteric techniques or meditation without the proper guidance of a teacher.
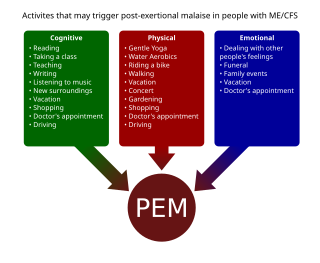
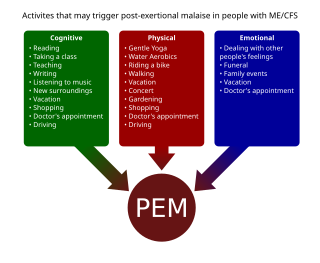
Post-exertional malaise (PEM), sometimes referred to as post-exertional symptom exacerbation (PESE), is a worsening of symptoms that occurs after minimal exertion. It is the hallmark symptom of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and common in long COVID and fibromyalgia. PEM is often severe enough to be disabling, and is triggered by ordinary activities that healthy people tolerate. Typically, it begins 12–48 hours after the activity that triggers it, and lasts for days, but this is highly variable and may persist much longer. Management of PEM is symptom-based, and patients are recommended to pace their activities to avoid triggering PEM.

Tongue diagnosis in Chinese Medicine is a method of diagnosing disease and disease patterns by visual inspection of the tongue and its various features. It is one of the major diagnostic methods in Chinese Medicine since the time of the Yellow Emperor's Inner Classic. It is considered a part of the “Inspection” method within the four methods of diagnosis. Practitioners claim that the tongue provides important clues reflecting the conditions of the internal organs. Like other diagnostic methods in Traditional Chinese Medicine, tongue diagnosis is based on the “outer reflects the inner” principle, which is that external structures often reflect the conditions of the internal structures and can give us important indications of internal disharmony.