The Health Insurance Portability and Accountability Act of 1996 is a United States Act of Congress enacted by the 104th United States Congress and signed into law by President Bill Clinton on August 21, 1996. It aimed to alter the transfer of healthcare information, stipulated the guidelines by which personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and addressed some limitations on healthcare insurance coverage. It generally prohibits healthcare providers and businesses called covered entities from disclosing protected information to anyone other than a patient and the patient's authorized representatives without their consent. The bill does not restrict patients from receiving information about themselves. Furthermore, it does not prohibit patients from voluntarily sharing their health information however they choose, nor does it require confidentiality where a patient discloses medical information to family members, friends or other individuals not employees of a covered entity.
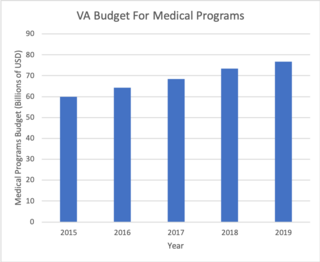
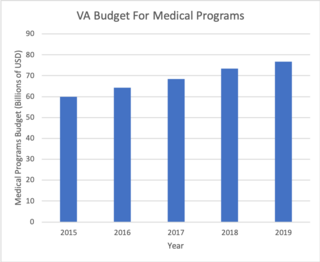
The Veterans Health Administration (VHA) is the component of the United States Department of Veterans Affairs (VA) led by the Under Secretary of Veterans Affairs for Health that implements the healthcare program of the VA through a nationalized healthcare service in the United States, providing healthcare and healthcare-adjacent services to veterans through the administration and operation of 146 VA Medical Centers (VAMC) with integrated outpatient clinics, 772 Community Based Outpatient Clinics (CBOC), and 134 VA Community Living Centers Programs. It is the largest division in the department, and second largest in the entire federal government, employing over 350,000 employees. All VA hospitals, clinics and medical centers are owned by and operated by the Department of Veterans Affairs, and all of the staff employed in VA hospitals are federal employees. Because of this, veterans that qualify for VHA healthcare do not pay premiums or deductibles for their healthcare but may have to make copayments depending on the medical procedure. VHA is not a part of the US Department of Defense Military Health System.
A Federally Qualified Health Center (FQHC) is a reimbursement designation from the Bureau of Primary Health Care and the Centers for Medicare and Medicaid Services of the United States Department of Health and Human Services. This designation is significant for several health programs funded under the Health Center Consolidation Act.
A medical classification is used to transform descriptions of medical diagnoses or procedures into standardized statistical code in a process known as clinical coding. Diagnosis classifications list diagnosis codes, which are used to track diseases and other health conditions, inclusive of chronic diseases such as diabetes mellitus and heart disease, and infectious diseases such as norovirus, the flu, and athlete's foot. Procedure classifications list procedure code, which are used to capture interventional data. These diagnosis and procedure codes are used by health care providers, government health programs, private health insurance companies, workers' compensation carriers, software developers, and others for a variety of applications in medicine, public health and medical informatics, including:

An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.
A personal health record (PHR) is a health record where health data and other information related to the care of a patient is maintained by the patient. This stands in contrast to the more widely used electronic medical record, which is operated by institutions and contains data entered by clinicians to support insurance claims. The intention of a PHR is to provide a complete and accurate summary of an individual's medical history which is accessible online. The health data on a PHR might include patient-reported outcome data, lab results, and data from devices such as wireless electronic weighing scales or from a smartphone.
The eHealth Exchange, formerly known as the Nationwide Health Information Network, is an initiative for the exchange of healthcare information. It was developed under the auspices of the U.S. Office of the National Coordinator for Health Information Technology (ONC), and now managed by a non-profit industry coalition called Sequoia Project. The exchange is a web-services based series of specifications designed to securely exchange healthcare related data. The NwHIN is related to the Direct Project which uses a secure email-based approach. One of the latest goals is to increase the amount of onboarding information about the NwHIN to prospective vendors of health care systems.
WEDI, pronounced "wee dee", is a not-for-profit user group in the United States for users of Electronic Data Interchange (EDI) in public and private healthcare. It is sometimes referred to by other names including some or all of the words Workgroup for Electronic Data Interchange.
Patient portals are healthcare-related online applications that allow patients to interact and communicate with their healthcare providers, such as physicians and hospitals. Typically, portal services are available on the Internet at all hours of the day and night. Some patient portal applications exist as stand-alone web sites and sell their services to healthcare providers. Other portal applications are integrated into the existing web site of a healthcare provider. Still others are modules added onto an existing electronic medical record (EMR) system. What all of these services share is the ability of patients to interact with their medical information via the Internet. Currently, the lines between an EMR, a personal health record, and a patient portal are blurring. For example, Intuit Health and Microsoft HealthVault describe themselves as personal health records (PHRs), but they can interface with EMRs and communicate through the Continuity of Care Record standard, displaying patient data on the Internet so it can be viewed through a patient portal.
The Office of the National Coordinator for Health Information Technology (ONC) is a staff division of the Office of the Secretary, within the U.S. Department of Health and Human Services. ONC leads national health IT efforts, charged as the principal federal entity to coordinate nationwide efforts to implement and use the most advanced health information technology and the electronic exchange of health information.

The Veterans Health Information Systems and Technology Architecture (VISTA) is the system of record for the clinical, administrative and financial operations of the Veterans Health Administration VISTA consists of over 180 clinical, financial, and administrative applications integrated within a single shared lifelong database (figure 1).
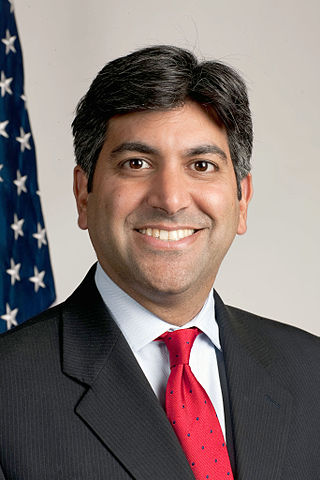
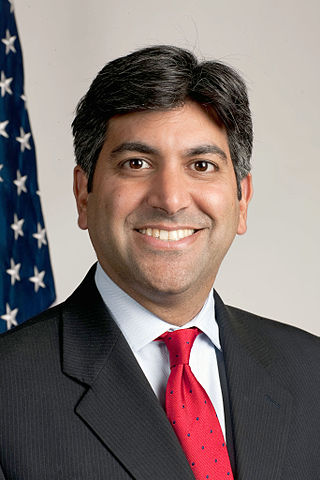
Aneesh Paul Chopra is an American executive who served as the first Chief Technology Officer of the United States. He was appointed in 2009 by President Barack Obama and was at the White House through 2012. Chopra previously served as Virginia's Secretary of Technology under Governor Tim Kaine. Chopra was a candidate in 2013 for the Democratic nomination for Lieutenant Governor of Virginia. He is the author of Innovative State: How New Technologies Can Transform Government (2014) and co-founder and president of CareJourney. In 2015 he joined Albright Stonebridge Group as a senior advisor.

Stephen L. Ondra is the chief medical adviser for the MITRE Corporation’s work as operator of the CMS Alliance to Modernize Healthcare federally funded research and development center. Ondra advises all HHS organizations to advance private insurance markets, Medicare and Medicaid, value-based payments, and healthcare quality. Ondra was most recently CEO of Cygnus-AI Inc., a company specializing in artificial intelligence and clinical decision support tools for diagnostic radiology. He was also founder and chief executive officer of North Star Health Care Consulting, and served on the board of directors of Triple-S Management and electroCore. A neurosurgeon and neuroscientist, Ondra has also served in senior positions in the Federal government, having a role in health reform efforts and the implementation of the Affordable Care Act. He advises corporations, provider organizations and early-stage start-ups on the transition to value-based care and health IT strategy.
An accountable care organization (ACO) is a healthcare organization that ties provider reimbursements to quality metrics and reductions in the cost of care. ACOs in the United States are formed from a group of coordinated health-care practitioners. They use alternative payment models, normally, capitation. The organization is accountable to patients and third-party payers for the quality, appropriateness and efficiency of the health care provided. According to the Centers for Medicare and Medicaid Services, an ACO is "an organization of health care practitioners that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries who are enrolled in the traditional fee-for-service program who are assigned to it".
The Health Information Technology for Economic and Clinical Health Act, abbreviated the HITECH Act, was enacted under Title XIII of the American Recovery and Reinvestment Act of 2009. Under the HITECH Act, the United States Department of Health and Human Services resolved to spend $25.9 billion to promote and expand the adoption of health information technology. The Washington Post reported the inclusion of "as much as $36.5 billion in spending to create a nationwide network of electronic health records." At the time it was enacted, it was considered "the most important piece of health care legislation to be passed in the last 20 to 30 years" and the "foundation for health care reform."
The Fast Healthcare Interoperability Resources standard is a set of rules and specifications for exchanging electronic health care data. It is designed to be flexible and adaptable, so that it can be used in a wide range of settings and with different health care information systems. The goal of FHIR is to enable the seamless and secure exchange of health care information, so that patients can receive the best possible care. The standard describes data formats and elements and an application programming interface (API) for exchanging electronic health records (EHR). The standard was created by the Health Level Seven International (HL7) health-care standards organization.

Medical image sharing is the electronic exchange of medical images between hospitals, physicians and patients. Rather than using traditional media, such as a CD or DVD, and either shipping it out or having patients carry it with them, technology now allows for the sharing of these images using the cloud. The primary format for images is DICOM. Typically, non-image data such as reports may be attached in standard formats like PDF during the sending process. Additionally, there are standards in the industry, such as IHE Cross Enterprise Document Sharing for Imaging (XDS-I), for managing the sharing of documents between healthcare enterprises. A typical architecture involved in setup is a locally installed server, which sits behind the firewall, allowing secure transmissions with outside facilities. In 2009, the Radiological Society of North America launched the "Image Share" project, with the goal of giving patients control of their imaging histories by allowing them to manage these records as they would online banking or shopping.
Health care analytics is the health care analysis activities that can be undertaken as a result of data collected from four areas within healthcare; claims and cost data, pharmaceutical and research and development (R&D) data, clinical data, and patient behavior and sentiment data (patient behaviors and preferences,. Health care analytics is a growing industry in the United States, expected to grow to more than $31 billion by 2022. The industry focuses on the areas of clinical analysis, financial analysis, supply chain analysis, as well as marketing, fraud and HR analysis.
Federal and state governments, insurance companies and other large medical institutions are heavily promoting the adoption of electronic health records. The US Congress included a formula of both incentives and penalties for EMR/EHR adoption versus continued use of paper records as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the, American Recovery and Reinvestment Act of 2009.

My Health Record (MHR) is the national digital health record platform for Australia, and is managed by the Australian Digital Health Agency. It was originally established as the Personally Controlled Electronic Health Record (PCEHR), a shared electronic health summary set up by the Australian government with implementation overseen by the National Electronic Health Transition Authority (NEHTA). The purpose of the MHR is to provide a secure electronic summary of people's medical history which will eventually include information such as current medications, adverse drug reactions, allergies and immunisation history in an easily accessible format. This MHR is stored in a network of connected systems with the ability to improve the sharing of information amongst health care providers to improve patient outcomes no matter where in Australia a patient presents for treatment. PCEHR was an opt-in system with a unique individual healthcare identifier (IHI) being assigned to participants and the option of masking and limiting information available for viewing controlled by the patient or a nominated representative; MHR uses an opt-out system.