Related Research Articles
In a support group, members provide each other with various types of help, usually nonprofessional and nonmaterial, for a particular shared, usually burdensome, characteristic. Members with the same issues can come together for sharing coping strategies, to feel more empowered and for a sense of community. The help may take the form of providing and evaluating relevant information, relating personal experiences, listening to and accepting others' experiences, providing sympathetic understanding and establishing social networks. A support group may also work to inform the public or engage in advocacy.

Telehealth is the distribution of health-related services and information via electronic information and telecommunication technologies. It allows long-distance patient and clinician contact, care, advice, reminders, education, intervention, monitoring, and remote admissions. Telemedicine is sometimes used as a synonym, or is used in a more limited sense to describe remote clinical services, such as diagnosis and monitoring. When rural settings, lack of transport, a lack of mobility, conditions due to outbreaks, epidemics or pandemics, decreased funding, or a lack of staff restrict access to care, telehealth may bridge the gap as well as provide distance-learning; meetings, supervision, and presentations between practitioners; online information and health data management and healthcare system integration. Telehealth could include two clinicians discussing a case over video conference; a robotic surgery occurring through remote access; physical therapy done via digital monitoring instruments, live feed and application combinations; tests being forwarded between facilities for interpretation by a higher specialist; home monitoring through continuous sending of patient health data; client to practitioner online conference; or even videophone interpretation during a consult.
eHealth describes healthcare services which are supported by digital processes, communication or technology such as electronic prescribing, Telehealth, or Electronic Health Records (EHRs). The use of electronic processes in healthcare dated back to at least the 1990s. Usage of the term varies as it covers not just "Internet medicine" as it was conceived during that time, but also "virtually everything related to computers and medicine". A study in 2005 found 51 unique definitions. Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet. It can also include health applications and links on mobile phones, referred to as mHealth or m-Health. Key components of eHealth include electronic health records (EHRs), telemedicine, health information exchange, mobile health applications, wearable devices, and online health information. These technologies enable healthcare providers, patients, and other stakeholders to access, manage, and exchange health information more effectively, leading to improved communication, decision-making, and overall healthcare outcomes.
A personal health record (PHR) is a health record where health data and other information related to the care of a patient is maintained by the patient. This stands in contrast to the more widely used electronic medical record, which is operated by institutions and contains data entered by clinicians to support insurance claims. The intention of a PHR is to provide a complete and accurate summary of an individual's medical history which is accessible online. The health data on a PHR might include patient-reported outcome data, lab results, and data from devices such as wireless electronic weighing scales or from a smartphone.
Thomas William "Tom" Ferguson was an American medical doctor, educator, and author. He was an early advocate for patient empowerment, urging patients to educate themselves, to assume control of their own health care, and to use the Internet as a way of accomplishing those goals.

Gunther Eysenbach is a German-Canadian researcher on healthcare, especially health policy, eHealth, and consumer health informatics.
The Journal of Medical Internet Research is a peer-reviewed open-access medical journal established in 1999 covering eHealth and "healthcare in the Internet age". The editors-in-chief are Gunther Eysenbach and Rita Kukafka. The publisher is JMIR Publications.
Online health communities are online social networks related to health. They primarily provide a means for patients and their families to learn about illnesses, to seek and offer social support, and to connect with others in similar circumstances. These online groups can be composed of individuals with illnesses, groups of medical professionals with shared interests, non-professional caregivers and family of patients, or a combination. The term "online health community" is primarily academic jargon.
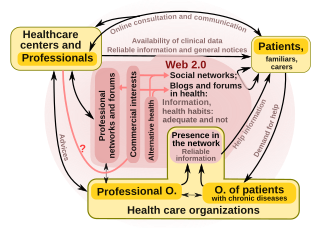
"Health 2.0" is a term introduced in the mid-2000s, as the subset of health care technologies mirroring the wider Web 2.0 movement. It has been defined variously as including social media, user-generated content, and cloud-based and mobile technologies. Some Health 2.0 proponents see these technologies as empowering patients to have greater control over their own health care and diminishing medical paternalism. Critics of the technologies have expressed concerns about possible misinformation and violations of patient privacy.

mHealth is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices. The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and personal digital assistants (PDAs), and wearable devices such as smart watches, for health services, information, and data collection. The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information. mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery/sharing of healthcare information for practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care as well as training and collaboration of health workers.
Patient participation is a trend that arose in answer to medical paternalism. Informed consent is a process where patients make decisions informed by the advice of medical professionals.
Shared decision-making in medicine (SDM) is a process in which both the patient and physician contribute to the medical decision-making process and agree on treatment decisions. Health care providers explain treatments and alternatives to patients and help them choose the treatment option that best aligns with their preferences as well as their unique cultural and personal beliefs.
Clinical point of care (POC) is the point in time when clinicians deliver healthcare products and services to patients at the time of care.

The Wikipedia online encyclopedia has, since the late 2000s, served as a popular source for health information for both laypersons and, in many cases, health care practitioners. Health-related articles on Wikipedia are popularly accessed as results from search engines, which frequently deliver links to Wikipedia articles. Independent assessments have been made of the number and demographics of people who seek health information on Wikipedia, the scope of health information on Wikipedia, and the quality and reliability of the information on Wikipedia.
Digital health is a discipline that includes digital care programs, technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and to make medicine more personalized and precise. It uses information and communication technologies to facilitate understanding of health problems and challenges faced by people receiving medical treatment and social prescribing in more personalised and precise ways. The definitions of digital health and its remits overlap in many ways with those of health and medical informatics.
Health information on the Internet refers to all health-related information communicated through or available on the Internet.
Infodemiology was defined by Gunther Eysenbach in the early 2000s as information epidemiology. It is an area of science research focused on scanning the internet for user-contributed health-related content, with the ultimate goal of improving public health. It is also defined as the science of mitigating public health problems resulting from an infodemic.
Digital medicine refers to the application of advanced digital technologies, such as artificial intelligence, machine learning, and big data analytics, to improve patient outcomes and healthcare delivery. It involves the integration of technology and medicine to facilitate the creation, storage, analysis, and dissemination of health information, with the aim of enhancing clinical decision-making, improving patient care, and reducing costs.
Health data is any data "related to health conditions, reproductive outcomes, causes of death, and quality of life" for an individual or population. Health data includes clinical metrics along with environmental, socioeconomic, and behavioral information pertinent to health and wellness. A plurality of health data are collected and used when individuals interact with health care systems. This data, collected by health care providers, typically includes a record of services received, conditions of those services, and clinical outcomes or information concerning those services. Historically, most health data has been sourced from this framework. The advent of eHealth and advances in health information technology, however, have expanded the collection and use of health data—but have also engendered new security, privacy, and ethical concerns. The increasing collection and use of health data by patients is a major component of digital health.

Internet-based treatments for trauma survivors is a growing class of online treatments that allow for an individual who has experienced trauma to seek and receive treatment without needing to attend psychotherapy in person. The progressive movement to online resources and the need for more accessible mental health services has given rise to the creation of online-based interventions aimed to help those who have experienced traumatic events. Cognitive behavioral therapy (CBT) has shown to be particularly effective in the treatment of trauma-related disorders and adapting CBT to an online format has been shown to be as effective as in-person CBT in the treatment of trauma. Due to its positive outcomes, CBT-based internet treatment options for trauma survivors has been an expanding field in both research and clinical settings.
References
- 1 2 Masters, K.; Ng'Ambi, D.; Todd, G. (2010). "'I Found it on the Internet': Preparing for the e-patient in Oman". Sultan Qaboos University Medical Journal. 10 (2): 169–179. PMC 3074705 . PMID 21509226.
- ↑ "Fox, Susannah; Fallows, Deborah. 2003. Health searches and email have become more commonplace, but there is room for improvement in searches and overall Internet access" (PDF). Archived from the original (PDF) on 2023-03-25. Retrieved 2011-07-05.
- ↑ Eysenbach G Medicine 2.0: Social Networking, Collaboration, Participation, Apomediation, and Openness. J Med Internet Res 2008;10(3):e22
- ↑ Kevin Kruse. "What do you mean, 'e-patient'?". Blog.kruresearch.com. Archived from the original on 2013-08-25. Retrieved 2013-09-13.
- ↑ Hewitt-Taylor, Jaqui; Bond, Carol S (8 November 2012). "What E-patients Want From the Doctor-Patient Relationship: Content Analysis of Posts on Discussion Boards" (PDF). Journal of Medical Internet Research. 14 (6): e155. doi: 10.2196/jmir.2068 . PMC 3510709 . PMID 23137788.
- ↑ Finding Answers Online in Sickness and in Health, 5/2/2006, Pew Internet Archived 2008-03-06 at the Wayback Machine .
- ↑ Eysenbach G (2003). "The impact of the Internet on cancer outcomes". CA: A Cancer Journal for Clinicians. 53 (6): 356–71. CiteSeerX 10.1.1.526.4309 . doi:10.3322/canjclin.53.6.356. PMID 15224975. S2CID 10192148.
- ↑ Jacobson P (2007). "Empowering the physician-patient relationship: The effect of the Internet". Partnership: The Canadian Journal of Library and Information Practice and Research. 2 (1). doi: 10.21083/partnership.v2i1.244 . ISSN 1911-9593.
- ↑ Ahmad F, Hudak PL, Bercovitz K, Hollenberg E, Levinson W (2006). "Are Physicians Ready for Patients With Internet-Based Health Information?". Journal of Medical Internet Research. 8 (3): e22. doi: 10.2196/jmir.8.3.e22 . PMC 2018833 . PMID 17032638.
- ↑ Crocco AG, Villasis-Keever M, Jadad AR (June 2002). "Analysis of cases of harm associated with use of health information on the internet". JAMA. 287 (21): 2869–71. doi: 10.1001/jama.287.21.2869 . PMID 12038937.
- ↑ Feder, Judith; Sands, Daniel Z. (2008-02-25). "A Reader and Author Respond to 'ePatients: Engaging Patients in Their Own Care'". Medscape Journal of Medicine. 10 (2): 46. ISSN 1934-1997. PMC 2270894 . PMID 18382715.
- 1 2 3 Ferguson, Tom; Frydman, Gilles (2004-05-15). "The First Generation of E-Patients: These New Medical Colleagues Could Provide Sustainable Healthcare Solutions". British Medical Journal. 328 (7449): 1148–1149. doi:10.1136/bmj.328.7449.1148. ISSN 0959-8138. PMC 411079 . PMID 15142894.
- ↑ Santana, Silvina; Lausen, Berthold; Bujnowska-Fedak, Maria; Chronaki, Catherine E.; Prokosch, Hans-Ulrich; Wynn, Rolf (2011-04-16). "Informed citizen and empowered citizen in health: results from an European survey". BMC Family Practice. 12: 20. doi: 10.1186/1471-2296-12-20 . ISSN 1471-2296. PMC 3101118 . PMID 21496309.
- ↑ Gómez-Zúñiga, Beni; Fernandez-Luque, Luis; Pousada, Modesta; Hernández-Encuentra, Eulàlia; Armayones, Manuel (2012-04-25). "ePatients on YouTube: Analysis of Four Experiences From the Patients' Perspective". Medicine 2.0. 1 (1): e1. doi: 10.2196/med2.2039 . ISSN 1923-2195. PMC 4084771 . PMID 25075229.
- ↑ Utengen, Audun; Rouholiman, Dara; Gamble, Jamison G; III, Francisco Jose Grajales; Pradhan, Nisha; Staley, Alicia C; Bernstein, Liza; Young, Sean D; Clauson, Kevin A (2017). "Patient Participation at Health Care Conferences: Engaged Patients Increase Information Flow, Expand Propagation, and Deepen Engagement in the Conversation of Tweets Compared to Physicians or Researchers". Journal of Medical Internet Research. 19 (8): e280. doi: 10.2196/jmir.8049 . PMC 5579322 . PMID 28818821.
- ↑ Salmi, Liz; Brudnicki, Selina; Isono, Maho; Riggare, Sara; Rodriquez, Cecilia; Schaper, Louise K.; Walker, Jan; Delbanco, Tom (2020-09-01). "Six countries, six individuals: resourceful patients navigating medical records in Australia, Canada, Chile, Japan, Sweden and the USA". BMJ Open. 10 (9): e037016. doi: 10.1136/bmjopen-2020-037016 . ISSN 2044-6055. PMC 7493106 . PMID 32933961.
- ↑ Ferguson, Tom. "e-patients: How they can help us heal health care" (PDF).