Waterhouse–Friderichsen syndrome (WFS) is defined as adrenal gland failure due to bleeding into the adrenal glands, commonly caused by severe bacterial infection. Typically, it is caused by Neisseria meningitidis.

An ulcer is a sore on the skin or a mucous membrane, accompanied by the disintegration of tissue. Ulcers can result in complete loss of the epidermis and often portions of the dermis and even subcutaneous fat. Ulcers are most common on the skin of the lower extremities and in the gastrointestinal tract. An ulcer that appears on the skin is often visible as an inflamed tissue with an area of reddened skin. A skin ulcer is often visible in the event of exposure to heat or cold, irritation, or a problem with blood circulation.

Chancroid is a bacterial sexually transmitted infection characterized by painful sores on the genitalia. Chancroid is known to spread from one individual to another solely through sexual contact. However, there have been reports of accidental infection through the hand.
Bloodstream infections (BSIs) are infections of blood caused by blood-borne pathogens. The detection of microbes in the blood is always abnormal. A bloodstream infection is different from sepsis, which is characterized by severe inflammatory or immune responses of the host organism to pathogens.

Acute septic arthritis, infectious arthritis, suppurative arthritis, pyogenic arthritis, osteomyelitis, or joint infection is the invasion of a joint by an infectious agent resulting in joint inflammation. Generally speaking, symptoms typically include redness, heat and pain in a single joint associated with a decreased ability to move the joint. Onset is usually rapid. Other symptoms may include fever, weakness and headache. Occasionally, more than one joint may be involved, especially in neonates, younger children and immunocompromised individuals. In neonates, infants during the first year of life, and toddlers, the signs and symptoms of septic arthritis can be deceptive and mimic other infectious and non-infectious disorders.

Oral candidiasis (Acute pseudomembranous candidiasis), also known as oral thrush among other names, is candidiasis that occurs in the mouth. That is, oral candidiasis is a mycosis (yeast/fungal infection) of Candida species on the mucous membranes of the mouth.

Bacterial pneumonia is a type of pneumonia caused by bacterial infection.

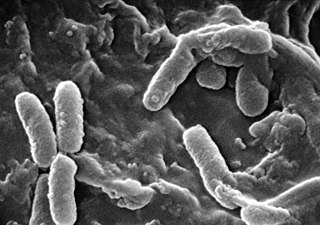
Pseudomonas aeruginosa is a common encapsulated, Gram-negative, aerobic–facultatively anaerobic, rod-shaped bacterium that can cause disease in plants and animals, including humans. A species of considerable medical importance, P. aeruginosa is a multidrug resistant pathogen recognized for its ubiquity, its intrinsically advanced antibiotic resistance mechanisms, and its association with serious illnesses – hospital-acquired infections such as ventilator-associated pneumonia and various sepsis syndromes. P. aeruginosa is able to selectively inhibit various antibiotics from penetrating its outer membrane - and has high resistance to several antibiotics. According to the World Health Organization P. aeruginosa poses one of the greatest threats to humans in terms of antibiotic resistance.

Gas gangrene is a bacterial infection that produces tissue gas in gangrene. This deadly form of gangrene usually is caused by Clostridium perfringens bacteria. About 1,000 cases of gas gangrene are reported yearly in the United States.
Community-acquired pneumonia (CAP) refers to pneumonia contracted by a person outside of the healthcare system. In contrast, hospital-acquired pneumonia (HAP) is seen in patients who have recently visited a hospital or who live in long-term care facilities. CAP is common, affecting people of all ages, and its symptoms occur as a result of oxygen-absorbing areas of the lung (alveoli) filling with fluid. This inhibits lung function, causing dyspnea, fever, chest pains and cough.

Pyoderma gangrenosum is a rare, inflammatory skin disease where painful pustules or nodules become ulcers that progressively grow. Pyoderma gangrenosum is not infectious.
Purpura fulminans is an acute, often fatal, thrombotic disorder which manifests as blood spots, bruising and discolouration of the skin resulting from coagulation in small blood vessels within the skin and rapidly leads to skin necrosis and disseminated intravascular coagulation.

Hot tub folliculitis, also called Pseudomonalfolliculitis or Pseudomonas aeruginosa folliculitis, is a common type of folliculitis featuring inflammation of hair follicles and surrounding skin.
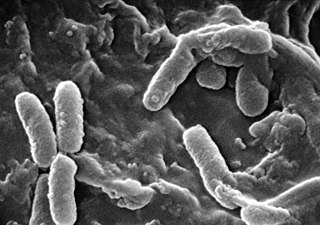
Pseudomonas infection refers to a disease caused by one of the species of the genus Pseudomonas.
Acne necrotica presents with a primary lesion that is a pruritic or painful erythematous follicular-based papule that develops central necrosis and crusting and heals with a varioliform scar.

Majocchi's granuloma is a skin condition characterized by deep, pustular plaques, and is a form of tinea corporis. It is a localized form of fungal folliculitis. Lesions often have a pink and scaly central component with pustules or folliculocentric papules at the periphery. The name comes from Domenico Majocchi, who discovered the disorder in 1883. Majocchi was a professor of dermatology at the University of Parma and later the University of Bologna. This disease is most commonly caused by filamentous fungi in the genus Trichophyton.

Helicobacter cinaedi is a bacterium in the family Helicobacteraceae, Campylobacterales order, Helicobacteraceae family, Helicobacter genus. It was formerly known as Campylobacter cinaedi until molecular analysis published in 1991 led to a major revision of the genus Campylobacter. H. cinaedi is a curved, spiral, or fusiform rod with flagellum at both of its ends which it uses to dart around. The bacterium is a pathogen.

Progressive vaccinia is a rare cutaneous condition caused by the vaccinia virus, characterized by painless but progressive necrosis and ulceration.
Pancreatic abscess is a late complication of acute necrotizing pancreatitis, occurring more than 4 weeks after the initial attack. A pancreatic abscess is a collection of pus resulting from tissue necrosis, liquefaction, and infection. It is estimated that approximately 3% of the patients with acute pancreatitis will develop an abscess.

Diabetic foot infection is any infection of the foot in a diabetic person. The most frequent cause of hospitalization for diabetic patients is due to foot infections. Symptoms may include pus from a wound, redness, swelling, pain, warmth, tachycardia, or tachypnea. Complications can include infection of the bone, tissue death, amputation, or sepsis. They are common and occur equally frequently in males and females. Older people are more commonly affected.