Related Research Articles

Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.
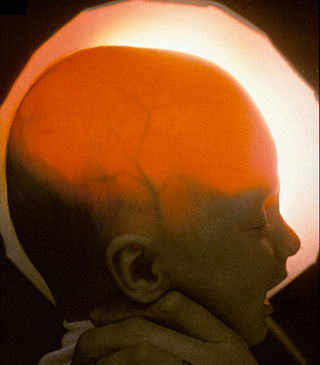
Hydranencephaly is a condition in which the brain's cerebral hemispheres are absent to a great degree and the remaining cranial cavity is filled with cerebrospinal fluid. "Cephalic" is the scientific term for "head" or "head end of body".

The ventricular system is a set of four interconnected cavities known as cerebral ventricles in the brain. Within each ventricle is a region of choroid plexus which produces the circulating cerebrospinal fluid (CSF). The ventricular system is continuous with the central canal of the spinal cord from the fourth ventricle, allowing for the flow of CSF to circulate.
Normal-pressure hydrocephalus (NPH), also called malresorptive hydrocephalus, is a form of communicating hydrocephalus in which excess cerebrospinal fluid (CSF) occurs in the ventricles, and with normal or slightly elevated cerebrospinal fluid pressure. As the fluid builds up, it causes the ventricles to enlarge and the pressure inside the head to increase, compressing surrounding brain tissue and leading to neurological complications. The disease presents in a classic triad of symptoms, which are memory impairment, urinary frequency, and balance problems/gait deviations. The disease was first described by Salomón Hakim and Adams in 1965.

In the brain, the interventricular foramina are channels that connect the paired lateral ventricles with the third ventricle at the midline of the brain. As channels, they allow cerebrospinal fluid (CSF) produced in the lateral ventricles to reach the third ventricle and then the rest of the brain's ventricular system. The walls of the interventricular foramina also contain choroid plexus, a specialized CSF-producing structure, that is continuous with that of the lateral and third ventricles above and below it.

Dandy–Walker malformation (DWM), also known as Dandy–Walker syndrome (DWS), is a rare congenital brain malformation in which the part joining the two hemispheres of the cerebellum does not fully form, and the fourth ventricle and space behind the cerebellum are enlarged with cerebrospinal fluid. Most of those affected develop hydrocephalus within the first year of life, which can present as increasing head size, vomiting, excessive sleepiness, irritability, downward deviation of the eyes and seizures. Other, less common symptoms are generally associated with comorbid genetic conditions and can include congenital heart defects, eye abnormalities, intellectual disability, congenital tumours, other brain defects such as agenesis of the corpus callosum, skeletal abnormalities, an occipital encephalocele or underdeveloped genitalia or kidneys. It is sometimes discovered in adolescents or adults due to mental health problems.

The median portion of the wall of the forebrain consists of a thin lamina, the lamina terminalis, which stretches from the interventricular foramen to the recess at the base of the optic stalk and contains the vascular organ of the lamina terminalis, which regulates the osmotic concentration of the blood. The lamina terminalis is immediately anterior to the tuber cinereum; together they form the pituitary stalk.

Choroid plexus papilloma, also known as papilloma of the choroid plexus, is a rare benign neuroepithelial intraventricular WHO grade I lesion found in the choroid plexus. It leads to increased cerebrospinal fluid production, thus causing increased intracranial pressure and hydrocephalus.

A colloid cyst is a non-malignant tumor in the brain. It consists of a gelatinous material contained within a membrane of epithelial tissue. It is almost always found just posterior to the foramen of Monro in the anterior aspect of the third ventricle, originating from the roof of the ventricle. Because of its location, it can cause obstructive hydrocephalus and increased intracranial pressure. Colloid cysts represent 0.5–1.0% of intracranial tumors.

A cerebral shunt is a device permanently implanted inside the head and body to drain excess fluid away from the brain. They are commonly used to treat hydrocephalus, the swelling of the brain due to excess buildup of cerebrospinal fluid (CSF). If left unchecked, the excess CSF can lead to an increase in intracranial pressure (ICP), which can cause intracranial hematoma, cerebral edema, crushed brain tissue or herniation. The drainage provided by a shunt can alleviate or prevent these problems in patients with hydrocephalus or related diseases.

Intraventricular hemorrhage (IVH), also known as intraventricular bleeding, is a bleeding into the brain's ventricular system, where the cerebrospinal fluid is produced and circulates through towards the subarachnoid space. It can result from physical trauma or from hemorrhagic stroke.
Choroid plexus tumors are a rare type of cancer that occur from the brain tissue called choroid plexus of the brain. Choroid plexus tumors are uncommon tumors of the central nervous system that account for 0.5–0.6% of intracranial neoplasms in people of all ages. Choroid plexus papilloma, atypical choroid plexus papilloma, and choroid plexus carcinoma are the three World Health Organization grades for these cancers, respectively. Children under the age of five account for 10% of cases of choroid plexus tumors. In children and adults, respectively, the lateral ventricle and the fourth ventricle are common locations, About 5% of all choroid plexus tumors are located in the third ventricle. Along with other unusual places such the cerebellopontine angle, the Luschka foramen, or brain parenchyma, the third ventricle is a rare location for choroid plexus tumors. Together, atypical choroid plexus papilloma, and choroid plexus carcinoma make up around 25% of all choroid plexus tumors. Although there have been reports of third ventricle choroid plexus papillomas in people in their fifth decade of life, only 14% of choroid plexus tumors are reported to arise in infants. Most findings indicate that choroid plexus tumors have no sex predilection.
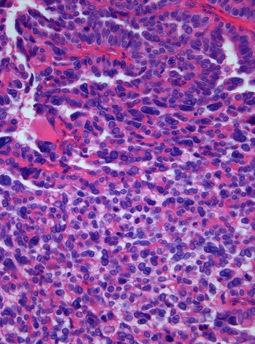
A choroid plexus carcinoma is a type of choroid plexus tumor that affects the choroid plexus of the brain. It is considered the worst of the three grades of chord plexus tumors, having a much poorer prognosis than choroid atypical plexus papilloma and choroid plexus papilloma. The disease creates lesions in the brain and increases cerebrospinal fluid volume, resulting in hydrocephalus.

An external ventricular drain (EVD), also known as a ventriculostomy or extraventricular drain, is a device used in neurosurgery to treat hydrocephalus and relieve elevated intracranial pressure when the normal flow of cerebrospinal fluid (CSF) inside the brain is obstructed. An EVD is a flexible plastic catheter placed by a neurosurgeon or neurointensivist and managed by intensive care unit (ICU) physicians and nurses. The purpose of external ventricular drainage is to divert fluid from the ventricles of the brain and allow for monitoring of intracranial pressure. An EVD must be placed in a center with full neurosurgical capabilities, because immediate neurosurgical intervention can be needed if a complication of EVD placement, such as bleeding, is encountered.
Bobble-head doll syndrome is a rare neurological movement disorder in which patients, usually children around age 3, begin to bob their head and shoulders forward and back, or sometimes side-to-side, involuntarily, in a manner reminiscent of a bobblehead doll. The syndrome is related to cystic lesions and swelling of the third ventricle in the brain.
CURE Children's Hospital of Uganda (CCHU) is a specialized children's neurosurgery hospital in Uganda. It is a private hospital, owned and operated by CURE International. The hospital is also a teaching center in pediatric neurosurgery for Sub-Saharan Africa.

Aqueductal stenosis is a narrowing of the aqueduct of Sylvius which blocks the flow of cerebrospinal fluid (CSF) in the ventricular system. Blockage of the aqueduct can lead to hydrocephalus, specifically as a common cause of congenital and/or obstructive hydrocephalus.
Benjamin Warf is an American pediatric neurosurgeon. Warf was awarded a MacArthur Fellowship in 2012.

Sandi Lam is a Canadian pediatric neurosurgeon and is known for her research in minimally invasive endoscopic hemispherectomy for patients with epilepsy. Lam is the Vice Chair for Pediatric Neurological Surgery at Northwestern University and the Division Chief of Pediatric Neurosurgery at Lurie Children's Hospital. She has spent her career advancing pediatric brain surgery capabilities globally through her work in Kenya performing surgeries as well as training and mentoring local residents and fellows.
References
- ↑ Kahle, Kristopher T; Kulkarni, Abhaya V; Limbrick, David D; Warf, Benjamin C (2016). "Hydrocephalus in children". The Lancet. 387 (10020): 788–99. doi:10.1016/s0140-6736(15)60694-8. PMID 26256071.
- ↑ Hydrocephalus and Treatment: Shunts and Endoscopic Third Ventriculostomy, AboutKidsHealth.ca
- ↑ Bouras, T.; Sgouros, S. (2013). "Complications of endoscopic third ventriculostomy". Journal of Neurosurgery. 79 (2 Supple): e9–12. doi:10.1016/j.wneu.2012.02.014. PMID 22381818.
- ↑ Vulcu, Sonja; Eickele, Leonie; Cinalli, Giuseppe; Wagner, Wolfgang; Oertel, Joachim (2015-07-31). "Long-term results of endoscopic third ventriculostomy: an outcome analysis". Journal of Neurosurgery. 123 (6): 1456–1462. doi: 10.3171/2014.11.jns14414 . PMID 26230473.
- ↑ Drake, J.; Chumas, P.; Kestle, J.; Pierre-Kahn, A.; Vinchon, M.; Brown, J.; Pollack, I.F.; Arai, H. (2006). "Late rapid deterioration after endoscopic third ventriculostomy: additional cases and review of the literature". Journal of Neurosurgery. 105 (2 Supple): 118–26. doi:10.3171/ped.2006.105.2.118. PMID 16922073. S2CID 41357365.
- ↑ Oertel, Joachim M. K.; Vulcu, Sonja; Schroeder, Henry W. S.; Konerding, Moritz A.; Wagner, Wolfgang; Gaab, Michael R. (2010). "Endoscopic transventricular third ventriculostomy through the lamina terminalis". Journal of Neurosurgery. 113 (6): 1261–9. doi:10.3171/2010.6.JNS09491. PMID 20707616. S2CID 9327180.
- ↑ Komotar, Ricardo J.; Hahn, David K.; Kim, Grace H.; Starke, Robert M.; Garrett, Matthew C.; Merkow, Maxwell B.; Otten, Marc L.; Sciacca, Robert R.; Connolly, E. Sander (2009). "Efficacy of lamina terminalis fenestration in reducing shunt-dependent hydrocephalus following aneurysmal subarachnoid hemorrhage: A systematic review". Journal of Neurosurgery. 111 (1): 147–54. doi:10.3171/2009.1.JNS0821. PMID 19284236. S2CID 28475913.
- ↑ Sgouros, S.; Kulkharni, A. V.; Constantini, S. (2005-10-15). "The international infant hydrocephalus study: concept and rational". Child's Nervous System. 22 (4): 338–345. doi:10.1007/s00381-005-1253-y. ISSN 0256-7040. PMID 16228238.
- ↑ Constantini, S.; Sgouros, S.; Kulkarni, A. (2013). "Neuroendoscopy in the youngest age group". World Neurosurgery. 79 (2 Supple): S23.e1–11. doi:10.1016/j.wneu.2012.02.003. PMID 22381849.
- ↑ "Neurosurgeons challenged to eliminate all infant deaths from hydrocephalus". EurekAlert. Retrieved 14 January 2016.
- ↑ Warf, B.C.; Tracy, S.; Mugamba, J. (2012). "Long-term outcome for endoscopic third ventriculostomy alone or in combination with choroid plexus cauterization for congenital aqueductal stenosis in African infants". Journal of Neurosurgery. Pediatrics. 10 (2): 108–11. doi:10.3171/2012.4.PEDS1253. PMID 22747094.
- ↑ Stone, S.S.; Warf, B.C. (2014). "Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment for infant hydrocephalus: a prospective North American series". Journal of Neurosurgery. Pediatrics. 14 (5): 439–46. doi: 10.3171/2014.7.PEDS14152 . PMID 25171723.
- ↑ Riva-Cambrin, Jay. "ETV+CPC Success and Evolving Indications over Time: A Prospective HCRN Study". Hydrocephalus Clinical Research Network. Retrieved 7 March 2016.
- ↑ Kulkarni, A.V.; Riva-Cambrin, J.; Browd, S.R.; Drake, J.M.; Holubkov, R.; Kestle, J.R.; Limbrick, D.D.; Rozzelle, C.J.; Simon, T.D.; Tamber, M.S.; Wellons, J.C.3rd.; Whitehead, W.E.; Hydrocephalus Clinical Research Network. (2014). "Endoscopic third ventriculostomy and choroid plexus cauterization in infants with hydrocephalus: a retrospective Hydrocephalus Clinical Research Network study". Journal of Neurosurgery. Pediatrics. 14 (3): 224–9. doi: 10.3171/2014.6.PEDS13492 . PMID 24995823.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ↑ Ruparell, Asha. "New neurosurgery saves lives in Calgary by treating hydrocephalus, 'water in the brain'". Global News. Retrieved 25 May 2016.
- 1 2 Kulkarni, A.V.; Drake, J.M.; Mallucci, C.L.; Sgouros, S.; Roth, J.; Constantini, S.; Canadian Pediatric Neurosurgery Study Group (2009). "Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus". Journal of Pediatrics. 155 (2): 254–9. doi:10.1016/j.jpeds.2009.02.048. PMID 19446842.
- ↑ Durnford, Andrew J.; Kirkham, Fenella J.; Mathad, Nijaguna; Sparrow, Owen C. E. (2011-11-01). "Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus: validation of a success score that predicts long-term outcome". Journal of Neurosurgery: Pediatrics. 8 (5): 489–493. doi:10.3171/2011.8.PEDS1166. ISSN 1933-0707. PMID 22044375.
- ↑ Breimer, G. E.; Sival, D. A.; Brusse-Keizer, M. G. J.; Hoving, E. W. (2013-05-05). "An external validation of the ETVSS for both short-term and long-term predictive adequacy in 104 pediatric patients". Child's Nervous System. 29 (8): 1305–1311. doi:10.1007/s00381-013-2122-8. ISSN 0256-7040. PMID 23644629.
- ↑ Labidi, M.; Lavoie, P.; Lapointe, G.; Obaid, D.; Weil, A.G.; Bojanowski, M.W.; Turmel, A. (2015-07-24). "Predicting success of endoscopic third ventriculostomy: validation of the ETV Success Score in a mixed population of adult and pediatric patients". Journal of Neurosurgery. 123 (6): 1447–1455. doi: 10.3171/2014.12.JNS141240 . PMID 26207604.
- ↑ Peretta, P.; Cinalli, G.; Spennato, P.; Ragazzi, P.; Rugierro, C.; Aliberti, F.; Carlino, C.; Cianciulli, E. (2009). "Long-term results of a second endoscopic third ventriculostomy in children: retrospective analysis of 40 cases". Neurosurgery. 65 (3): 539–47. doi:10.1227/01.NEU.0000350228.08523.D1. PMID 19687699.
- ↑ Marano, Paul J.; Stone, Scellig S. D.; Mugamba, John; Ssenyonga, Peter; Warf, Ezra B.; Warf, Benjamin C. (2015-02-06). "Reopening of an obstructed third ventriculostomy: long-term success and factors affecting outcome in 215 infants". Journal of Neurosurgery: Pediatrics. 15 (4): 399–405. doi: 10.3171/2014.10.peds14250 . PMID 25658247.
- ↑ Choudhury, N.; Gelinas-Phaneuf, F.; Delorme, S.; Del Maestro, R. (2013). "Fundamentals of neurosurgery: virtual reality tasks for training and evaluation of technical skills". World Neurosurgery. 80 (5): e9–19. doi:10.1016/j.wneu.2012.08.022. PMID 23178917.
- ↑ Breimer, G.E.; Bodani, V.; Looi, T.; Drake, J.M. (2015). "Design and evaluation of a new synthetic brain simulator for endoscopic third ventriculostomy". Journal of Neurosurgery. Pediatrics. 15 (1): 82–8. doi: 10.3171/2014.9.PEDS1447 . PMID 25360853. S2CID 10586172.
- ↑ Zymberg, S.; Vaz-Guimaraes Filho, F.; Lyra, M. (2010). "Neuroendoscopic training: presentation of a new real simulator". Minimally Invasive Neurosurgery. 53 (1): 44–6. doi:10.1055/s-0029-1246169. PMID 20376746.
- ↑ Breimer, Gerben E.; Haji, Faizal A.; Bodani, Vivek; Cunningham, Melissa S.; Lopez-Rios, Adriana-Lucia; Okrainec, Allan; Drake, James M. (June 2016). "Simulation-based Education for Endoscopic Third Ventriculostomy". Operative Neurosurgery. 13 (1): 89–95. doi:10.1227/NEU.0000000000001317. PMID 28931258.
- ↑ Breimer, Gerben E.; Haji, Faizal A.; Hoving, Eelco W.; Drake, James M. (2015-05-01). "Development and content validation of performance assessments for endoscopic third ventriculostomy". Child's Nervous System. 31 (8): 1247–1259. doi:10.1007/s00381-015-2716-4. ISSN 0256-7040. PMID 25930722.