Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. Cognitive behavioral therapy is one of the most effective means of treatment for substance abuse and co-occurring mental health disorders. CBT focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include many issues and the treatment of many mental health conditions, including anxiety, substance use disorders, marital problems, ADHD, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.
Psychotherapy is the use of psychological methods, particularly when based on regular personal interaction, to help a person change behavior, increase happiness, and overcome problems. Psychotherapy aims to improve an individual's well-being and mental health, to resolve or mitigate troublesome behaviors, beliefs, compulsions, thoughts, or emotions, and to improve relationships and social skills. Numerous types of psychotherapy have been designed either for individual adults, families, or children and adolescents. Certain types of psychotherapy are considered evidence-based for treating some diagnosed mental disorders; other types have been criticized as pseudoscience.
Group psychotherapy or group therapy is a form of psychotherapy in which one or more therapists treat a small group of clients together as a group. The term can legitimately refer to any form of psychotherapy when delivered in a group format, including art therapy, cognitive behavioral therapy or interpersonal therapy, but it is usually applied to psychodynamic group therapy where the group context and group process is explicitly utilized as a mechanism of change by developing, exploring and examining interpersonal relationships within the group.
Psychedelic therapy refers to the proposed use of psychedelic drugs, such as psilocybin, MDMA, LSD, and ayahuasca, to treat mental disorders. As of 2021, psychedelic drugs are controlled substances in most countries and psychedelic therapy is not legally available outside clinical trials, with some exceptions.
Eye movement desensitization and reprocessing (EMDR) is a form of psychotherapy that is controversial within the psychological community. It was devised by Francine Shapiro in 1987 and originally designed to alleviate the distress associated with traumatic memories such as post-traumatic stress disorder (PTSD).

Art therapy is a distinct discipline that incorporates creative methods of expression through visual art media. Art therapy, as a creative arts therapy profession, originated in the fields of art and psychotherapy and may vary in definition. Art therapy encourages creative expression through painting, drawing, or modelling. It may work by providing a person with a safe space to express their feelings and allow them to feel more in control over their life.
The Bobath concept is an approach to neurological rehabilitation that is applied in patient assessment and treatment. The goal of applying the Bobath concept is to promote motor learning for efficient motor control in various environments, thereby improving participation and function. This is done through specific patient handling skills to guide patients through the initiation and completing of intended tasks. This approach to neurological rehabilitation is multidisciplinary, primarily involving physiotherapists, occupational therapists, and speech and language therapists. In the United States, the Bobath concept is also known as 'neuro-developmental treatment' (NDT).
Psychodynamic psychotherapy and psychoanalytic psychotherapy are two categories of psychological therapies. Their main purpose is revealing the unconscious content of a client's psyche in an effort to alleviate psychic tension, which is inner conflict within the mind that was created in a situation of extreme stress or emotional hardship, often in the state of distress. The terms "psychoanalytic psychotherapy" and "psychodynamic psychotherapy" are often used interchangeably, but a distinction can be made in practice: though psychodynamic psychotherapy largely relies on psychoanalytical theory, it employs substantially shorter treatment periods than traditional psychoanalytical therapies. Psychodynamic psychotherapy is evidence-based; the effectiveness of psychoanalysis and its relationship to facts is disputed.
Behaviour therapy or behavioural psychotherapy is a broad term referring to clinical psychotherapy that uses techniques derived from behaviourism and/or cognitive psychology. It looks at specific, learned behaviours and how the environment, or other people's mental states, influences those behaviours, and consists of techniques based on behaviorism's theory of learning: respondent or operant conditioning. Behaviourists who practice these techniques are either behaviour analysts or cognitive-behavioural therapists. They tend to look for treatment outcomes that are objectively measurable. Behaviour therapy does not involve one specific method, but it has a wide range of techniques that can be used to treat a person's psychological problems.
Professional Association of Therapeutic Horsemanship International, formerly the North American Riding for the Handicapped Association (NARHA), is a non-profit organization based in Denver, Colorado, that promotes the benefits of therapeutic horseback riding and other equine-assisted activities and therapies for people with physical, emotional and learning disabilities. PATH Intl. serves people of all ages, backgrounds and walks of life. They serve people with both physical challenges as well as those with mental challenges. Some examples of challenges participants face are multiple sclerosis, down syndrome, post traumatic stress disorder, autism and traumatic brain injuries. PATH Intl. is a 501(c)(3) organization.
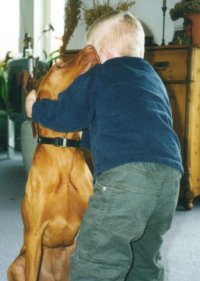
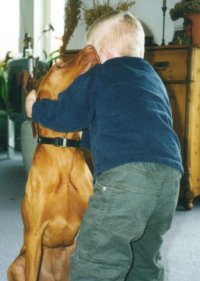
Animal-assisted therapy (AAT) is an alternative or complementary type of therapy that includes the use of animals in a treatment. The goal of this animal-assisted intervention is to improve a patient's social, emotional, or cognitive functioning. Studies have documented some positive effects of the therapy on subjective self-rating scales and on objective physiological measures such as blood pressure and hormone levels.
Child psychotherapy, or mental health interventions for children refers to the psychological treatment of various mental disorders diagnosed in children and adolescents. The therapeutic techniques developed for younger age ranges specialize in prioritizing the relationship between the child and the therapist. The goal of maintaining positive therapist-client relationships is typically achieved using therapeutic conversations and can take place with the client alone, or through engagement with family members.
Aquatic therapy refers to treatments and exercises performed in water for relaxation, fitness, physical rehabilitation, and other therapeutic benefit. Typically a qualified aquatic therapist gives constant attendance to a person receiving treatment in a heated therapy pool. Aquatic therapy techniques include Ai Chi, Aqua Running, Bad Ragaz Ring Method, Burdenko Method, Halliwick, Watsu, and other aquatic bodywork forms. Therapeutic applications include neurological disorders, spine pain, musculoskeletal pain, postoperative orthopedic rehabilitation, pediatric disabilities, pressure ulcers, and disease conditions, such as osteoporosis.
Common factors theory, a theory guiding some research in clinical psychology and counseling psychology, proposes that different approaches and evidence-based practices in psychotherapy and counseling share common factors that account for much of the effectiveness of a psychological treatment. This is in contrast to the view that the effectiveness of psychotherapy and counseling is best explained by specific or unique factors that are suited to treatment of particular problems.
The mainstay of management of borderline personality disorder is various forms of psychotherapy with medications being found to be of little use.

Over time, the approach to cerebral palsy management has shifted away from narrow attempts to fix individual physical problems – such as spasticity in a particular limb – to making such treatments part of a larger goal of maximizing the person's independence and community engagement. Much of childhood therapy is aimed at improving gait and walking. Approximately 60% of people with CP are able to walk independently or with aids at adulthood. However, the evidence base for the effectiveness of intervention programs reflecting the philosophy of independence has not yet caught up: effective interventions for body structures and functions have a strong evidence base, but evidence is lacking for effective interventions targeted toward participation, environment, or personal factors. There is also no good evidence to show that an intervention that is effective at the body-specific level will result in an improvement at the activity level, or vice versa. Although such cross-over benefit might happen, not enough high-quality studies have been done to demonstrate it.
PTSD or post-traumatic stress disorder, is a psychiatric disorder characterised by intrusive thoughts and memories, dreams or flashbacks of the event; avoidance of people, places and activities that remind the individual of the event; ongoing negative beliefs about oneself or the world, mood changes and persistent feelings of anger, guilt or fear; alterations in arousal such as increased irritability, angry outbursts, being hypervigilant, or having difficulty with concentration and sleep.
Horseback riding simulators are intended to allow people to gain the benefits of therapeutic horseback riding or to gain skill and conditioning for equestrian activity while diminishing the issues of surrounding cost, availability, and individual comfort level around horses. Horseback therapy has been used by many types of therapists to advance their physical, mental, emotional, and social skills.
Horses Healing Hearts (HHH) is a 501(c)3 charitable organization located in South Florida, United States. This psychoeducational program helps children whose parents suffer from the disease of addiction. While providing a safe and nurturing environment to build self-esteem and confidence by working with horses, HHH equips children with the tools to change their lives and break the generational cycle of addiction. It was founded in 2009 by Lizabeth Olszewski.

Equine-assisted therapy or equine-assisted therapy on autistic people is a therapy using a mediating horse or pony. A session can take place on foot or on horseback. Equine-assisted therapy is one of the few animal-assisted therapies regularly studied for its effectiveness, and the most popular of all autism therapies.