Related Research Articles
Bipolar I disorder is a type of bipolar spectrum disorder characterized by the occurrence of at least one manic episode, with or without mixed or psychotic features. Most people also, at other times, have one or more depressive episodes, and all experience a hypomanic stage before progressing to full mania.
A mental disorder, also referred to as a mental illness or psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. A mental disorder is also characterized by a clinically significant disturbance in an individual's cognition, emotional regulation, or behaviour. It is usually associated with distress or impairment in important areas of functioning. There are many different types of mental disorders. Mental disorders may also be referred to as mental health conditions. Such features may be persistent, relapsing and remitting, or occur as single episodes. Many disorders have been described, with signs and symptoms that vary widely between specific disorders. Such disorders may be diagnosed by a mental health professional, usually a clinical psychologist or psychiatrist.

Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterised by excessive amounts of inattention, hyperactivity, and impulsivity that are pervasive, impairing in multiple contexts, and otherwise age-inappropriate.
Conduct disorder (CD) is a mental disorder diagnosed in childhood or adolescence that presents itself through a repetitive and persistent pattern of behavior that includes theft, lies, physical violence that may lead to destruction, and reckless breaking of rules, in which the basic rights of others or major age-appropriate norms are violated. These behaviors are often referred to as "antisocial behaviors." It is often seen as the precursor to antisocial personality disorder, which by definition cannot be diagnosed until the individual is 18 years old. Conduct disorder may result from parental rejection and neglect and can be treated with family therapy, as well as behavioral modifications and pharmacotherapy. Conduct disorder is estimated to affect 51.1 million people globally as of 2013.
Antisocial personality disorder is a personality disorder characterized by a limited capacity for empathy as well as a difficulty sustaining long-term relationships. A long-term pattern of disregard or violation of the rights of others and a contemptuous or vindictive attitude are often apparent, as well as a history of rule-breaking that can sometimes include law-breaking, manipulation, compulsive lying for amusement or personal gain, a tendency towards chronic boredom and substance abuse, and impulsive and aggressive behavior. Antisocial behaviors often have their onset before the age of 8, and in nearly 80% of ASPD cases, the subject will develop their first symptoms by age 11. The prevalence of ASPD peaks in people age 24 to 44 years old, and often decreases in people age 45 to 64 years. In the United States, the rate of antisocial personality disorder in the general population is estimated between 0.5 and 3.5 percent. In a study, a random sampling of 320 newly incarcerated offenders found ASPD was present in over 35 percent of those surveyed. One out of 17 (6%) of divorces involves a person affected by ASPD.

Obsessive–compulsive personality disorder (OCPD) is a cluster C personality disorder marked by a spectrum of obsessions with rules, lists, schedules, and order, among other things. Symptoms are usually present by the time a person reaches adulthood, and are visible in a variety of situations. The cause of OCPD is thought to involve a combination of genetic and environmental factors, namely problems with attachment.
Avoidant personality disorder (AvPD) or Anxious personality disorder is a Cluster C personality disorder characterized by excessive social anxiety and inhibition, fear of intimacy, severe feelings of inadequacy and inferiority, and an overreliance on avoidance of feared stimuli as a maladaptive coping method. Those affected typically display a pattern of extreme sensitivity to negative evaluation and rejection, a belief that one is socially inept or personally unappealing to others, and avoidance of social interaction despite a strong desire for it. It appears to affect an approximately equal number of men and women.
Child psychopathology refers to the scientific study of mental disorders in children and adolescents. Oppositional defiant disorder, attention-deficit hyperactivity disorder, and autism spectrum disorder are examples of psychopathology that are typically first diagnosed during childhood. Mental health providers who work with children and adolescents are informed by research in developmental psychology, clinical child psychology, and family systems. Lists of child and adult mental disorders can be found in the International Statistical Classification of Diseases and Related Health Problems, 10th Edition (ICD-10), published by the World Health Organization (WHO) and in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association (APA). In addition, the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood is used in assessing mental health and developmental disorders in children up to age five.
Sluggish cognitive tempo (SCT) is a syndrome related to attention deficit hyperactivity disorder (ADHD) but distinct from it. Typical symptoms include prominent dreaminess, mental fogginess, hypoactivity, sluggishness, staring frequently, inconsistent alertness and a slow working speed.
Oppositional defiant disorder (ODD) is listed in the DSM-5 under Disruptive, impulse-control, and conduct disorders and defined as "a pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness". This behavior is usually targeted toward peers, parents, teachers, and other authority figures. Unlike conduct disorder (CD), those with ODD do not show patterns of aggression towards people or animals, destruction of property, theft, or deceit. One half of children with ODD also fulfill the diagnostic criteria for ADHD.

Sadistic personality disorder is a personality disorder defined by a pervasive pattern of sadistic and cruel behavior. People with this disorder were thought to have desired to control others. It was believed they accomplish this through the use of physical or emotional violence. This diagnosis appeared in an appendix of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R). The later versions of the DSM do not include it. It was removed as psychiatrists believed it would be used to legally excuse sadistic behavior.
Emotional and behavioral disorders refer to a disability classification used in educational settings that allows educational institutions to provide special education and related services to students who have displayed poor social and/or academic progress.

The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is the 2013 update to the Diagnostic and Statistical Manual of Mental Disorders, the taxonomic and diagnostic tool published by the American Psychiatric Association (APA). In the United States, the DSM serves as the principal authority for psychiatric diagnoses. Treatment recommendations, as well as payment by health care providers, are often determined by DSM classifications, so the appearance of a new version has practical importance. However, not all providers rely on the DSM-5 for planning treatment as the ICD's mental disorder diagnoses are used around the world and scientific studies often measure changes in symptom scale scores rather than changes in DSM-5 criteria to determine the real-world effects of mental health interventions. The DSM-5 is the only DSM to use an Arabic numeral instead of a Roman numeral in its title, as well as the only living document version of a DSM.
Personality disorders (PD) are a class of mental disorders characterized by enduring maladaptive patterns of behavior, cognition, and inner experience, exhibited across many contexts and deviating from those accepted by the individual's culture. These patterns develop early, are inflexible, and are associated with significant distress or disability. The definitions vary by source and remain a matter of controversy. Official criteria for diagnosing personality disorders are listed in the sixth chapter of the International Classification of Diseases (ICD) and in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM).
Childhood schizophrenia is similar in characteristics of schizophrenia that develops at a later age, but has an onset before the age of 13 years, and is more difficult to diagnose. Schizophrenia is characterized by positive symptoms that can include hallucinations, delusions, and disorganized speech; negative symptoms, such as blunted affect and avolition and apathy, and a number of cognitive impairments. Differential diagnosis is problematic since several other neurodevelopmental disorders, including autism spectrum disorder, language disorder, and attention deficit hyperactivity disorder, also have signs and symptoms similar to childhood-onset schizophrenia.
In personality pathology, dimensional models of personality disorders conceptualize personality disorders as quantitatively rather than qualitatively different from normal personality. They consist of extreme, maladaptive levels of certain personality characteristics. Within the context of personality psychology, a "dimension" refers to a continuum on which an individual can have various levels of a characteristic, in contrast to the dichotomous categorical approach in which an individual does or does not possess a characteristic. According to dimensional models personality disorders are classified according to which characteristics are expressed at which levels. This stands in contrast to the traditional categorical models of classification, which are based on the boolean presence or absence of symptoms and do not take into account levels of expression of a characteristic or the presence of any underlying dimension.

Disruptive mood dysregulation disorder (DMDD) is a mental disorder in children and adolescents characterized by a persistently irritable or angry mood and frequent temper outbursts that are disproportionate to the situation and significantly more severe than the typical reaction of same-aged peers. DMDD was added to the DSM-5 as a type of depressive disorder diagnosis for youths. The symptoms of DMDD resemble those of attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), anxiety disorders, and childhood bipolar disorder.

Stephen P. Hinshaw is an American psychologist whose contributions lie in the areas of developmental psychopathology and combating the stigma that surrounds mental illness. He has authored more than 325 scientific articles and chapters as well as 14 authored and edited books. Currently, he is Professor in the Department of Psychology at the University of California, Berkeley, and Professor In Residence and Vice Chair for Child and Adolescent Psychology in the Department of Psychiatry at the University of California, San Francisco. His work focuses on child and adolescent mental disorders, clinical interventions, mechanisms of change in psychopathology, and stigma prevention efforts, with a specialization in ADHD and other externalizing behavioral disorders.
Borderline personality disorder (BPD) is a psychological disorder characterized by chronic instability of relationships, self-image, moods, and affect, which is frequently misdiagnosed. This misdiagnosis can come in the form of providing a BPD diagnosis to a person who does not actually meet criteria or providing an incorrect alternative diagnosis in the place of a BPD diagnosis.
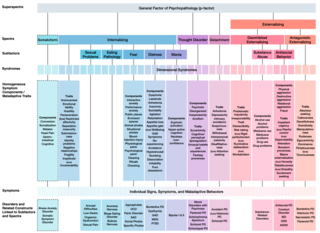
The Hierarchical Taxonomy Of Psychopathology (HiTOP) consortium was formed in 2015 as a grassroots effort to articulate a classification of mental health problems based on recent scientific findings on how the components of mental disorders fit together. The consortium is developing the HiTOP model, a classification system, or taxonomy, of mental disorders, or psychopathology, aiming to prioritize scientific results over convention and clinical opinion. The motives for proposing this classification were to aid clinical practice and mental health research. The consortium was organized by Drs. Roman Kotov, Robert Krueger, and David Watson. At inception it included 40 psychologists and psychiatrists, who had a record of scientific contributions to classification of psychopathology The HiTOP model aims to address limitations of traditional classification systems for mental illness, such as the DSM-5 and ICD-10, by organizing psychopathology according to evidence from research on observable patterns of mental health problems.
References
- 1 2 Krueger, Robert F.; Markon, Kristian E.; Patrick, Christopher J.; Iacono, William G. (2005-11-01). "Externalizing Psychopathology in Adulthood: A Dimensional-Spectrum Conceptualization and Its Implications for DSM–V". Journal of Abnormal Psychology. 114 (4): 537–550. doi:10.1037/0021-843X.114.4.537. ISSN 0021-843X. PMC 2242352 . PMID 16351376.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 "Disruptive, Impulse-Control, and Conduct Disorders". Diagnostic and Statistical Manual of Mental Disorders . DSM Library. American Psychiatric Association. 2013-05-22. doi:10.1176/appi.books.9780890425596.dsm15. ISBN 978-0-89042-555-8.
- 1 2 McMahon, R. J. (1994-10-01). "Diagnosis, assessment, and treatment of externalizing problems in children: the role of longitudinal data". Journal of Consulting and Clinical Psychology. 62 (5): 901–917. doi:10.1037/0022-006x.62.5.901. ISSN 0022-006X. PMID 7806720.
- ↑ "Use of the Manual". Diagnostic and Statistical Manual of Mental Disorders . DSM Library. American Psychiatric Association. 2013-05-22. doi:10.1176/appi.books.9780890425596.useofdsm5. ISBN 978-0-89042-555-8.
- ↑ "Introduction". Diagnostic and Statistical Manual of Mental Disorders . DSM Library. American Psychiatric Association. 2013-05-22. doi:10.1176/appi.books.9780890425596.introduction. ISBN 978-0-89042-555-8.
- ↑ Turygin, Nicole C.; Matson, Johnny L.; Adams, Hilary; Belva, Brian (August 2013). "The effect of DSM-5 criteria on externalizing, internalizing, behavioral and adaptive symptoms in children diagnosed with autism". Developmental Neurorehabilitation. 16 (4): 277–282. doi:10.3109/17518423.2013.769281. PMID 23617257. S2CID 23850413.
- ↑ Lyness, KP; Koehler, AN (2016). "Effect of coping on substance use in adolescent girls: a dyadic analysis of parent and adolescent perceptions." International Journal of Adolescence and Youth. 21. (4): 449-461. http://dx.doi.org/10.1080/02673843.2013.866146
- ↑ Drabick, Deborah, A.G.; Steinberg, Elizabeth; Hampton Shields, Ashley (2015). "Overview of DSM Disruptive Behavior Disorders". In Beauchaine, Theodore P.; Hinshaw, Stephen P. (eds.). The Oxford Handbook of Externalizing Spectrum Disorders. New York, New York: Oxford University Press. p. 9. ISBN 978-0-19-932467-5.
- ↑ Regier, Darrel A.; Kuhl, Emily A.; Kupfer, David J. (June 2013). "The DSM-5: Classification and criteria changes". World Psychiatry. 12 (2): 92–98. doi:10.1002/wps.20050. PMC 3683251 . PMID 23737408.
- 1 2 3 4 5 Kotsopoulos, S. (2013-05-22). "Neurodevelopmental Disorders". Diagnostic and Statistical Manual of Mental Disorders. DSM Library. Vol. 26. American Psychiatric Association. p. 257. doi:10.1176/appi.books.9780890425596.dsm01. ISBN 978-0-89042-555-8. PMC 1408294 .
- 1 2 "Personality Disorders". Diagnostic and Statistical Manual of Mental Disorders . DSM Library. American Psychiatric Association. 2013-05-22. doi:10.1176/appi.books.9780890425596.dsm18. ISBN 978-0-89042-555-8.
- 1 2 3 "Substance-Related and Addictive Disorders". Diagnostic and Statistical Manual of Mental Disorders . DSM Library. American Psychiatric Association. 2013-05-22. doi:10.1176/appi.books.9780890425596.dsm16. ISBN 978-0-89042-555-8.
- ↑ Levy, Florence; Hawes, David J.; Johns, Adam (2015). "Externalizing and Internalizing Comorbidity". In Beauchaine, Theodore P.; Hinshaw, Stephen P. (eds.). The Oxford Handbook of Externalizing Spectrum Disorders. New York, New York: Oxford University Press. ISBN 978-0-19-932467-5.
- ↑ Nikolas, Molly A. (2015). "Comorbidity Among Externalizing Disorders". In Beauchaine, Theodore P.; Hinshaw, Stephen P. (eds.). Overview of DSM Disruptive Behavior Disorders. New York, New York: Oxford University Press. ISBN 978-0-19-932467-5.
- 1 2 3 Beauchaine, Theodore P.; McNulty, Tiffany (2013-11-01). "Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology". Development and Psychopathology. 25 (25th Anniversary Special Issue 4pt2): 1505–1528. doi:10.1017/S0954579413000746. ISSN 1469-2198. PMC 4008972 . PMID 24342853.
- ↑ Steinberg, Elizabeth A.; Drabick, Deborah A. G. (2015-02-07). "A Developmental Psychopathology Perspective on ADHD and Comorbid Conditions: The Role of Emotion Regulation". Child Psychiatry & Human Development. 46 (6): 951–966. doi:10.1007/s10578-015-0534-2. ISSN 0009-398X. PMID 25662998. S2CID 25617531.
- ↑ Picoito, João; Santos, Constança; Nunes, Carla (2020-06-19). "Heterogeneity and heterotypic continuity of emotional and behavioural profiles across development". Social Psychiatry and Psychiatric Epidemiology. 56 (5): 807–819. doi:10.1007/s00127-020-01903-y. ISSN 0933-7954. PMID 32561937. S2CID 219935864.
- ↑ Picoito, João (2020-07-08). "Commentary on Evans et al . (2020): the complex interplay between adolescent substance use, internalizing and externalizing symptoms". Addiction. 115 (10): 1942–1943. doi: 10.1111/add.15171 . ISSN 0965-2140. PMID 32639070.
- ↑ Hinshaw, Stephen P.; Stier, Andrea (2008-01-01). "Stigma as Related to Mental Disorders". Annual Review of Clinical Psychology. 4 (1): 367–393. doi:10.1146/annurev.clinpsy.4.022007.141245. PMID 17716044.
- ↑ Stier, Andrea; Hinshaw, Stephen P. (2007). "Explicit and implicit stigma against individuals with mental illness". Australian Psychologist. 42 (2): 106–117. doi:10.1080/00050060701280599.
- 1 2 Hinshaw, Stephen P. (2005-07-01). "The stigmatization of mental illness in children and parents: developmental issues, family concerns, and research needs". Journal of Child Psychology and Psychiatry. 46 (7): 714–734. doi:10.1111/j.1469-7610.2005.01456.x. ISSN 1469-7610. PMID 15972067.
- ↑ Hinshaw, Stephen P.; Cicchetti, Dante (2000). "Stigma and mental disorder: Conceptions of illness, public attitudes, personal disclosure, and social policy". Development and Psychopathology. 12 (4): 555–598. doi:10.1017/s0954579400004028. PMID 11202034. S2CID 11442378.
- 1 2 3 4 5 6 Frick, Paul J.; Ray, James V.; Thornton, Laura C.; Kahn, Rachel E. (2014-06-01). "Annual Research Review: A developmental psychopathology approach to understanding callous-unemotional traits in children and adolescents with serious conduct problems". Journal of Child Psychology and Psychiatry. 55 (6): 532–548. doi:10.1111/jcpp.12152. ISSN 1469-7610. PMID 24117854.
- 1 2 3 4 Waller, Rebecca; Gardner, Frances; Hyde, Luke W. (2013-06-01). "What are the associations between parenting, callous–unemotional traits, and antisocial behavior in youth? A systematic review of evidence". Clinical Psychology Review. 33 (4): 593–608. doi:10.1016/j.cpr.2013.03.001. PMID 23583974.
- 1 2 Hawes, David J.; Price, Matthew J.; Dadds, Mark R. (2014-04-19). "Callous-Unemotional Traits and the Treatment of Conduct Problems in Childhood and Adolescence: A Comprehensive Review". Clinical Child and Family Psychology Review. 17 (3): 248–267. doi:10.1007/s10567-014-0167-1. ISSN 1096-4037. PMID 24748077. S2CID 9188468.
- 1 2 3 Frick, Paul J.; Nigg, Joel T. (2012-01-01). "Current Issues in the Diagnosis of Attention Deficit Hyperactivity Disorder, Oppositional Defiant Disorder, and Conduct Disorder". Annual Review of Clinical Psychology. 8 (1): 77–107. doi:10.1146/annurev-clinpsy-032511-143150. PMC 4318653 . PMID 22035245.
- ↑ Pardini, Dustin A.; Frick, Paul J.; Moffitt, Terrie E. (2010). "Building an evidence base for DSM–5 conceptualizations of oppositional defiant disorder and conduct disorder: Introduction to the special section". Journal of Abnormal Psychology. 119 (4): 683–688. doi:10.1037/a0021441. PMC 3826598 . PMID 21090874.
- ↑ Craske, Michelle G. (2012-04-01). "The R-Doc Initiative: Science and Practice". Depression and Anxiety. 29 (4): 253–256. doi: 10.1002/da.21930 . ISSN 1520-6394. PMID 22511361. S2CID 30025777.
- ↑ McCrady, Barbara S. (2008). "Alcohol Use Disorders". In Barlow, David H. (ed.). Clinical Handbook of Psychological Disorders (4 ed.). New York, New York: The Guilford Press. ISBN 978-1-59385-572-7.
- ↑ Higgins, Stephen T.; Sigmon, Stacey C.; Heil, Sarah H. (2008). "Drug Abuse and Dependence". In Barlow, David H. (ed.). Clinical Handbook of Psychological Disorders (4 ed.). New York, New York: The Guilford Press. ISBN 978-1-59385-572-7.
- ↑ Maliken, Ashley C.; Katz, Lynn Fainsilber (2013-04-18). "Exploring the Impact of Parental Psychopathology and Emotion Regulation on Evidence-Based Parenting Interventions: A Transdiagnostic Approach to Improving Treatment Effectiveness". Clinical Child and Family Psychology Review. 16 (2): 173–186. doi:10.1007/s10567-013-0132-4. ISSN 1096-4037. PMID 23595362. S2CID 45147481.
- ↑ Menting, Ankie T. A.; Orobio de Castro, Bram; Matthys, Walter (2013-12-01). "Effectiveness of the Incredible Years parent training to modify disruptive and prosocial child behavior: A meta-analytic review". Clinical Psychology Review. 33 (8): 901–913. doi:10.1016/j.cpr.2013.07.006. hdl: 1874/379971 . PMID 23994367.
- ↑ Michelson, Daniel; Davenport, Clare; Dretzke, Janine; Barlow, Jane; Day, Crispin (2013-02-19). "Do Evidence-Based Interventions Work When Tested in the "Real World?" A Systematic Review and Meta-analysis of Parent Management Training for the Treatment of Child Disruptive Behavior". Clinical Child and Family Psychology Review. 16 (1): 18–34. doi:10.1007/s10567-013-0128-0. ISSN 1096-4037. PMID 23420407. S2CID 207101543.
- ↑ Furlong, Mairead; McGilloway, Sinead; Bywater, Tracey; Hutchings, Judy; Smith, Susan M; Donnelly, Michael (2013-03-07). "Cochrane Review: Behavioural and cognitive-behavioural group-based parenting programmes for early-onset conduct problems in children aged 3 to 12 years (Review)". Evidence-Based Child Health: A Cochrane Review Journal. 8 (2): 318–692. doi:10.1002/ebch.1905. ISSN 1557-6272. PMID 23877886.
- ↑ Zwi, Morris; Jones, Hannah; Thorgaard, Camilla; York, Ann; Dennis, Jane A (2011-12-07). "Parent training interventions for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years". Cochrane Database of Systematic Reviews. 2011 (12): CD003018. doi:10.1002/14651858.cd003018.pub3. PMC 6544776 . PMID 22161373.
- ↑ Storebø, Ole Jakob; Storm, Maja Rosenberg Overby; Pereira Ribeiro, Johanne; Skoog, Maria; Groth, Camilla; Callesen, Henriette E.; Schaug, Julie Perrine; Darling Rasmussen, Pernille; Huus, Christel-Mie L.; Zwi, Morris; Kirubakaran, Richard; Simonsen, Erik; Gluud, Christian (2023-03-27). "Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD)". The Cochrane Database of Systematic Reviews. 3 (3): CD009885. doi:10.1002/14651858.CD009885.pub3. ISSN 1469-493X. PMC 10042435 . PMID 36971690.
- ↑ Hinshaw, Stephen P. (2002-12-01). "Intervention research, theoretical mechanisms, and causal processes related to externalizing behavior patterns". Development and Psychopathology. 14 (4): 789–818. doi:10.1017/S0954579402004078. ISSN 1469-2198. PMID 12549704. S2CID 10985589.
- ↑ Safren, Steven A.; Otto, Michael W.; Sprich, Susan; Winett, Carol L.; Wilens, Timothy E.; Biederman, Joseph (2005-07-01). "Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms". Behaviour Research and Therapy. 43 (7): 831–842. doi:10.1016/j.brat.2004.07.001. PMID 15896281.
- ↑ Gibbon, Simon; Khalifa, Najat R.; Cheung, Natalie H.-Y.; Völlm, Birgit A.; McCarthy, Lucy (3 September 2020). "Psychological interventions for antisocial personality disorder". The Cochrane Database of Systematic Reviews. 2020 (9): CD007668. doi:10.1002/14651858.CD007668.pub3. ISSN 1469-493X. PMC 8094166 . PMID 32880104.
- ↑ Khalifa, Najat R.; Gibbon, Simon; Völlm, Birgit A.; Cheung, Natalie H.-Y.; McCarthy, Lucy (3 September 2020). "Pharmacological interventions for antisocial personality disorder". The Cochrane Database of Systematic Reviews. 2020 (9): CD007667. doi:10.1002/14651858.CD007667.pub3. ISSN 1469-493X. PMC 8094881 . PMID 32880105.
- ↑ "DSM-5 | psychiatry.org". www.psychiatry.org. Retrieved 2015-11-23.
- ↑ "DSM-5 Overview: The Future Manual".
- ↑ Biller, Peter; Hudson, Anne (6 June 1996). Heresy and Literacy, 1000-1530 (Volume 23 of Cambridge Studies in Medieval Literature). Cambridge University Press. ISBN 0521575761 . Retrieved 24 May 2021.