The Diagnostic and Statistical Manual of Mental Disorders is a publication by the American Psychiatric Association (APA) for the classification of mental disorders using a common language and standard criteria. It is the main book for the diagnosis and treatment of mental disorders in the United States and Australia, while in other countries it may be used in conjunction with other documents. The DSM-5 is considered one of the principal guides of psychiatry, along with the International Classification of Diseases (ICD), Chinese Classification of Mental Disorders (CCMD), and the Psychodynamic Diagnostic Manual. However, not all providers rely on the DSM-5 as a guide, since the ICD's mental disorder diagnoses are used around the world and scientific studies often measure changes in symptom scale scores rather than changes in DSM-5 criteria to determine the real-world effects of mental health interventions.
A mental disorder, also referred to as a mental illness, a mental health condition, or a psychiatric disability, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. A mental disorder is also characterized by a clinically significant disturbance in an individual's cognition, emotional regulation, or behavior, often in a social context. Such disturbances may occur as single episodes, may be persistent, or may be relapsing–remitting. There are many different types of mental disorders, with signs and symptoms that vary widely between specific disorders. A mental disorder is one aspect of mental health.

A mood disorder, also known as an affective disorder, is any of a group of conditions of mental and behavioral disorder where a disturbance in the person's mood is the main underlying feature. The classification is in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD).
A delusion is a false fixed belief that is not amenable to change in light of conflicting evidence. As a pathology, it is distinct from a belief based on false or incomplete information, confabulation, dogma, illusion, hallucination, or some other misleading effects of perception, as individuals with those beliefs are able to change or readjust their beliefs upon reviewing the evidence. However:

Borderline personality disorder (BPD), also known as emotionally unstable personality disorder (EUPD), is a personality disorder characterized by a pervasive, long-term pattern of significant interpersonal relationship instability, a distorted sense of self, and intense emotional responses. Individuals diagnosed with BPD frequently exhibit self-harming behaviours and engage in risky activities, primarily due to challenges in regulating emotional states to a healthy, stable baseline. Symptoms such as dissociation, a pervasive sense of emptiness, and an acute fear of abandonment are prevalent among those affected.

Hypochondriasis or hypochondria is a condition in which a person is excessively and unduly worried about having a serious illness. Hypochondria is an old concept whose meaning has repeatedly changed over its lifespan. It has been claimed that this debilitating condition results from an inaccurate perception of the condition of body or mind despite the absence of an actual medical diagnosis. An individual with hypochondriasis is known as a hypochondriac. Hypochondriacs become unduly alarmed about any physical or psychological symptoms they detect, no matter how minor the symptom may be, and are convinced that they have, or are about to be diagnosed with, a serious illness.

Conduct disorder (CD) is a mental disorder diagnosed in childhood or adolescence that presents itself through a repetitive and persistent pattern of behavior that includes theft, lies, physical violence that may lead to destruction, and reckless breaking of rules, in which the basic rights of others or major age-appropriate norms are violated. These behaviors are often referred to as "antisocial behaviors", and is often seen as the precursor to antisocial personality disorder; however, the latter, by definition, cannot be diagnosed until the individual is 18 years old. Conduct disorder may result from parental rejection and neglect and can be treated with family therapy, as well as behavioral modifications and pharmacotherapy. Conduct disorder is estimated to affect 51.1 million people globally as of 2013.
Abnormal psychology is the branch of psychology that studies unusual patterns of behavior, emotion, and thought, which could possibly be understood as a mental disorder. Although many behaviors could be considered as abnormal, this branch of psychology typically deals with behavior in a clinical context. There is a long history of attempts to understand and control behavior deemed to be aberrant or deviant, and there is often cultural variation in the approach taken. The field of abnormal psychology identifies multiple causes for different conditions, employing diverse theories from the general field of psychology and elsewhere, and much still hinges on what exactly is meant by "abnormal". There has traditionally been a divide between psychological and biological explanations, reflecting a philosophical dualism in regard to the mind–body problem. There have also been different approaches in trying to classify mental disorders. Abnormal includes three different categories; they are subnormal, supernormal and paranormal.
Avolition, as a symptom of various forms of psychopathology, is the decrease in the ability to initiate and persist in self-directed purposeful activities. Such activities that appear to be neglected usually include routine activities, including hobbies, going to work or school, and most notably, engaging in social activities. A person experiencing avolition may stay at home for long periods of time, rather than seeking out work or peer relations.
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usual, causing marked distress, preoccupation with the stressor and its consequences, and functional impairment.

The diathesis-stress model, also known as the vulnerability–stress model, is a psychological theory that attempts to explain a disorder, or its trajectory, as the result of an interaction between a predispositional vulnerability, the diathesis, and stress caused by life experiences. The term diathesis derives from the Greek term (διάθεσις) for a predisposition or sensibility. A diathesis can take the form of genetic, psychological, biological, or situational factors. A large range of differences exists among individuals' vulnerabilities to the development of a disorder.
The classification of mental disorders, also known as psychiatric nosology or psychiatric taxonomy, is central to the practice of psychiatry and other mental health professions.

The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is the 2013 update to the Diagnostic and Statistical Manual of Mental Disorders, the taxonomic and diagnostic tool published by the American Psychiatric Association (APA). In 2022, a revised version (DSM-5-TR) was published. In the United States, the DSM serves as the principal authority for psychiatric diagnoses. Treatment recommendations, as well as payment by health care providers, are often determined by DSM classifications, so the appearance of a new version has practical importance. However, not all providers rely on the DSM-5 for planning treatment as the ICD's mental disorder diagnoses are used around the world and scientific studies often measure changes in symptom scale scores rather than changes in DSM-5 criteria to determine the real-world effects of mental health interventions. The DSM-5 is the only DSM to use an Arabic numeral instead of a Roman numeral in its title, as well as the only living document version of a DSM.
Personality disorders (PD) are a class of mental disorders characterized by enduring maladaptive patterns of behavior, cognition, and inner experience, exhibited across many contexts and deviating from those accepted by the individual's culture. These patterns develop early, are inflexible, and are associated with significant distress or disability. The definitions vary by source and remain a matter of controversy. Official criteria for diagnosing personality disorders are listed in the sixth chapter of the International Classification of Diseases (ICD) and in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM).
The diagnosis of schizophrenia, a psychotic disorder, is based on criteria in either the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, or the World Health Organization's International Classification of Diseases (ICD). Clinical assessment of schizophrenia is carried out by a mental health professional based on observed behavior, reported experiences, and reports of others familiar with the person. Diagnosis is usually made by a psychiatrist. Associated symptoms occur along a continuum in the population and must reach a certain severity and level of impairment before a diagnosis is made. Schizophrenia has a prevalence rate of 0.3-0.7% in the United States.
In personality pathology, dimensional models of personality disorders conceptualize personality disorders as qualitatively rather than quantitatively different from normal personality. They consist of extreme, maladaptive levels of certain personality characteristics. Within the context of personality psychology, a "dimension" refers to a continuum on which an individual can have various levels of a characteristic, in contrast to the dichotomous categorical approach in which an individual does or does not possess a characteristic. According to dimensional models personality disorders are classified according to which characteristics are expressed at which levels. This stands in contrast to the traditional categorical models of classification, which are based on the boolean presence or absence of symptoms and do not take into account levels of expression of a characteristic or the presence of any underlying dimension.

The Research Domain Criteria (RDoC) project is an initiative of personalized medicine in psychiatry developed by US National Institute of Mental Health (NIMH). In contrast to the Diagnostic and Statistical Manual of Mental Disorders (DSM) maintained by the American Psychiatric Association (APA), RDoC aims to address the heterogeneity in the current nosology by providing a biologically-based, rather than symptom-based, framework for understanding mental disorders. "RDoC is an attempt to create a new kind of taxonomy for mental disorders by bringing the power of modern research approaches in genetics, neuroscience, and behavioral science to the problem of mental illness."
Externalizing disorders are mental disorders characterized by externalizing behaviors, maladaptive behaviors directed toward an individual's environment, which cause impairment or interference in life functioning. In contrast to individuals with internalizing disorders who internalize their maladaptive emotions and cognitions, such feelings and thoughts are externalized in behavior in individuals with externalizing disorders. Externalizing disorders are often specifically referred to as disruptive behavior disorders or conduct problems which occur in childhood. Externalizing disorders, however, are also manifested in adulthood. For example, alcohol- and substance-related disorders and antisocial personality disorder are adult externalizing disorders. Externalizing psychopathology is associated with antisocial behavior, which is different from and often confused for asociality.
Maladaptive daydreaming, also called excessive daydreaming, is when an individual experiences excessive daydreaming that interferes with daily life. It is a proposed diagnosis of a disordered form of dissociative absorption, associated with excessive fantasy that is not recognized by any major medical or psychological criteria. Maladaptive daydreaming can result in distress, can replace human interaction and may interfere with normal functioning such as social life or work. Maladaptive daydreaming is not a widely recognized diagnosis and is not found in any major diagnostic manual of psychiatry or medicine. The term was coined in 2002 by Eli Somer of the University of Haifa. Somer's definition of the proposed condition is "extensive fantasy activity that replaces human interaction and/or interferes with academic, interpersonal, or vocational functioning." There has been limited research outside of Somer's.
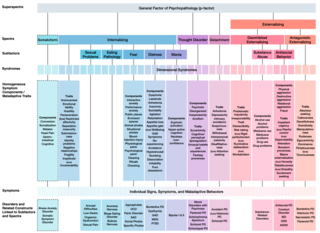
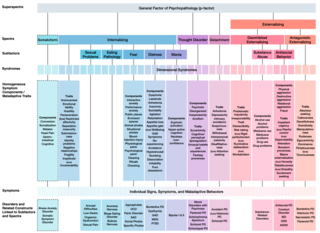
The Hierarchical Taxonomy Of Psychopathology (HiTOP) consortium was formed in 2015 as a grassroots effort to articulate a classification of mental health problems based on recent scientific findings on how the components of mental disorders fit together. The consortium is developing the HiTOP model, a classification system, or taxonomy, of mental disorders, or psychopathology, aiming to prioritize scientific results over convention and clinical opinion. The motives for proposing this classification were to aid clinical practice and mental health research. The consortium was organized by Drs. Roman Kotov, Robert Krueger, and David Watson. At inception it included 40 psychologists and psychiatrists, who had a record of scientific contributions to classification of psychopathology The HiTOP model aims to address limitations of traditional classification systems for mental illness, such as the DSM-5 and ICD-10, by organizing psychopathology according to evidence from research on observable patterns of mental health problems.