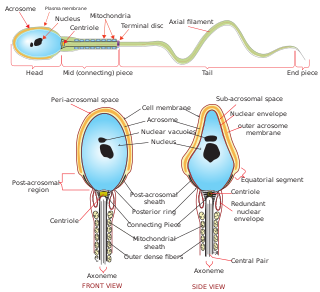
A spermatozoon is a motile sperm cell, or moving form of the haploid cell that is the male gamete. A spermatozoon joins an ovum to form a zygote.

Intracytoplasmic sperm injection is an in vitro fertilization (IVF) procedure in which a single sperm cell is injected directly into the cytoplasm of an egg. This technique is used in order to prepare the gametes for the obtention of embryos that may be transferred to a maternal uterus. With this method, the acrosome reaction is skipped.
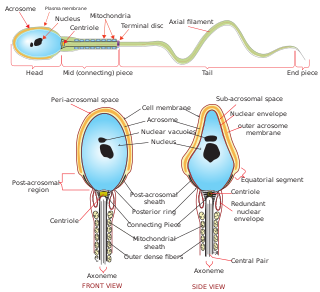
The acrosome is an organelle that develops over the anterior (front) half of the head in the spermatozoa of many animals including humans. It is a cap-like structure derived from the Golgi apparatus. In placental mammals the acrosome contains degradative enzymes. These enzymes break down the outer membrane of the ovum, called the zona pellucida, allowing the haploid nucleus in the sperm cell to join with the haploid nucleus in the ovum.

During fertilization, a sperm must first fuse with the plasma membrane and then penetrate the female egg cell to fertilize it. Fusing to the egg cell usually causes little problem, whereas penetrating through the egg's hard shell or extracellular matrix can be more difficult. Therefore, sperm cells go through a process known as the acrosome reaction, which is the reaction that occurs in the acrosome of the sperm as it approaches the egg.
Capacitation is the penultimate step in the maturation of mammalian spermatozoa and is required to render them competent to fertilize an oocyte. This step is a biochemical event; the sperm move normally and look mature prior to capacitation. In vivo, capacitation occurs after ejaculation, when the spermatozoa leave the vagina and enter the superior female reproductive tract. The uterus aids in the steps of capacitation by secreting sterol-binding albumin, lipoproteins, and proteolytic and glycosidasic enzymes such as heparin.
Hyperactivation is a type of sperm motility. Hyperactivated sperm motility is characterised by a high amplitude, asymmetrical beating pattern of the sperm tail (flagellum). This type of motility may aid in sperm penetration of the zona pellucida, which encloses the ovum.

A23187 is a mobile ion-carrier that forms stable complexes with divalent cations. A23187 is also known as Calcimycin, Calcium Ionophore, Antibiotic A23187 and Calcium Ionophore A23187. It is produced at fermentation of Streptomyceschartreusensis.
The hamster zona-free ovum test, or hamster egg-penetration test, or sometimes just hamster test, is an in-vitro test used to study physiological profile of spermatozoa. The primary application of the test is to diagnose male infertility caused by sperm unable to penetrate the ova. The test has limited value, due to expense and a high false negative rate.
The cation channels of sperm also known as Catsper channels or CatSper, are ion channels that are related to the two-pore channels and distantly related to TRP channels. The four members of this family form voltage-gated Ca2+ channels that seem to be specific to sperm. As sperm encounter the more alkaline environment of the female reproductive tract, CatSper channels become activated by the altered ion concentration. These channels are required for proper fertilization. The study of these channels has been slow because they do not traffic to the cell membrane in many heterologous systems.

In vitro maturation (IVM) is the technique of letting the contents of ovarian follicles and the oocytes inside mature in vitro. It can be offered to women with infertility problems, combined with In Vitro Fertilization (IVF), offering women pregnancy without ovarian stimulation.
The Genetics & IVF Institute (GIVF) is an international provider of infertility and genetics services and products, and also engages in biomedical research in these fields. The Institute was founded in 1984 by Dr. Joseph D. Schulman and associates. GIVF headquarters are in Fairfax, VA, US, and its facilities include locations in Pennsylvania, Minnesota, California, and Texas in the United States, as well as in China, Mexico, and several other countries.
Teratospermia or teratozoospermia is a condition characterized by the presence of sperm with abnormal morphology that affects fertility in males.
Oocyteactivation is a series of processes that occur in the oocyte during fertilization.
Jacques Cohen is a Dutch embryologist based in New York, U.S. He is currently Director at Reprogenetics LLC, Laboratory Director at ART Institute of Washington at Walter Reed National Military Medical Center, and Scientific Director of R & D at IVF-online.
The history of in vitro fertilisation (IVF) goes back more than half a century. In 1959 the first birth in a nonhuman mammal resulting from IVF occurred, and in 1978 the world's first baby conceived by IVF was born. As medicine advanced, IVF was transformed from natural research to a stimulated clinical treatment. There have been many refinements in the IVF process, and today millions of births have occurred with the help of IVF all over the world.
Antisperm antibodies (ASA) are antibodies produced against sperm antigens.
The intracytoplasmic morphologically selected sperm injection (IMSI) is a laboratory technique used for In vitro fertilisation treatments. High-quality sperms are injected into the egg for fertilization, it is an advanced version of ICSI. A high powered microscope is used to pick out and the best sperm cells which are then used in a traditional ICSI protocol. In ICSI a magnification of x400 is used, while in IMSI an amplification of x6000 to x10,000 is used, increasing the magnification by a factor of 15. This allows the sperm to be examined in greater detail, including the nucleus which contains the sperm's genetic material. The use of this method has resulted in higher pregnancy and delivery rates and lower abortion rates. IMSI is a method that can be chosen by for anyone who has failed IVF cycles in the past, and for couples who have a component of male infertility.
Spermatogenesis-associated protein 16 is a mammalian protein encoded by the SPATA16 gene. SPATA16, also known as NYD-SP12, is a developmental protein that aids in differentiation of germ cells for spermatogenesis and participates in acrosome formation for appropriate sperm-egg fusion. SPATA16 is located on chromosome 3 at position 26.31 and is a member of the tetratricopeptide repeat-like superfamily, which facilitate interactions and assemblies between proteins and protein complexes.
Sarah Martins Da SilvaMRCOG is a British gynaecologist and researcher specialising in male infertility. Da Silva is a senior lecturer in reproductive medicine at the University of Dundee. She also works as an honorary consultant gynaecologist at the Ninewells Hospital in Dundee, specialising in fertility problems and assisted conception. She was named one of the BBC's "100 Women of 2019" for her contribution to fertility science.
Dmitri Dozortsev is a Russian-American physician scientist, inventor and researcher. Dozortsev's contributions in research and publications are mostly in the areas of human reproductive medicine and biology. In particular, he is best known for his studies of in vitro fertilisation and embryo transfer. Dozortsev currently serves as President of the American College of Embryology and as Director of Omni-Med laboratories.