Capgras delusion or Capgras syndrome is a psychiatric disorder in which a person holds a delusion that a friend, spouse, parent, another close family member, or pet has been replaced by an identical impostor. It is named after Joseph Capgras (1873–1950), the French psychiatrist who first described the disorder.
The Fregoli delusion is a rare disorder in which a person holds a delusional belief that different people are in fact a single person who changes appearance or is in disguise. The syndrome may be related to a brain lesion and is often of a paranoid nature, with the delusional person believing themselves persecuted by the person they believe is in disguise.

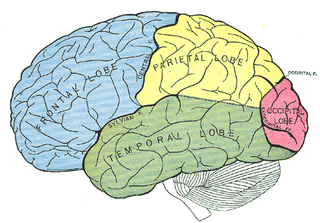
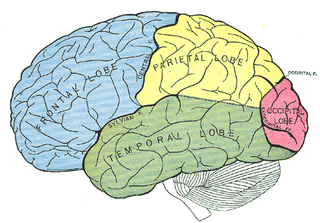
Hypergraphia is a behavioral condition characterized by the intense desire to write or draw. Forms of hypergraphia can vary in writing style and content. It is a symptom associated with temporal lobe changes in epilepsy and in Geschwind syndrome. Structures that may have an effect on hypergraphia when damaged due to temporal lobe epilepsy are the hippocampus and Wernicke's area. Aside from temporal lobe epilepsy, chemical causes may be responsible for inducing hypergraphia.
Bálint's syndrome is an uncommon and incompletely understood triad of severe neuropsychological impairments: inability to perceive the visual field as a whole (simultanagnosia), difficulty in fixating the eyes, and inability to move the hand to a specific object by using vision. It was named in 1909 for the Austro-Hungarian neurologist and psychiatrist Rezső Bálint who first identified it.
Reduplicative paramnesia is the delusional belief that a place or location has been duplicated, existing in two or more places simultaneously, or that it has been 'relocated' to another site. It is one of the delusional misidentification syndromes; although rare, it is most commonly associated with acquired brain injury, particularly simultaneous damage to the right cerebral hemisphere and to both frontal lobes.
Neuropsychiatry is a branch of medicine that deals with psychiatry as it relates to neurology, in an effort to understand and attribute behavior to the interaction of neurobiology and social psychology factors. Within neuropsychiatry, the mind is considered "as an emergent property of the brain", whereas other behavioral and neurological specialties might consider the two as separate entities. Those disciplines are typically practiced separately.

In the field of neurology, temporal lobe epilepsy is an enduring brain disorder that causes unprovoked seizures from the temporal lobe. Temporal lobe epilepsy is the most common type of focal onset epilepsy among adults. Seizure symptoms and behavior distinguish seizures arising from the medial temporal lobe from seizures arising from the lateral (neocortical) temporal lobe. Memory and psychiatric comorbidities may occur. Diagnosis relies on electroencephalographic (EEG) and neuroimaging studies. Anticonvulsant medications, epilepsy surgery and dietary treatments may improve seizure control.
Frontal lobe epilepsy (FLE) is a neurological disorder that is characterized by brief, recurring seizures arising in the frontal lobes of the brain, that often occur during sleep. It is the second most common type of epilepsy after temporal lobe epilepsy (TLE), and is related to the temporal form in that both forms are characterized by partial (focal) seizures.

Frontal lobe disorder, also frontal lobe syndrome, is an impairment of the frontal lobe of the brain due to disease or frontal lobe injury. The frontal lobe plays a key role in executive functions such as motivation, planning, social behaviour, and speech production. Frontal lobe syndrome can be caused by a range of conditions including head trauma, tumours, neurodegenerative diseases, neurodevelopmental disorders, neurosurgery and cerebrovascular disease. Frontal lobe impairment can be detected by recognition of typical signs and symptoms, use of simple screening tests, and specialist neurological testing.
Perseveration, in the fields of psychology, psychiatry, and speech–language pathology, is the repetition of a particular response regardless of the absence or cessation of a stimulus. It is usually caused by a brain injury or other organic disorder. Symptoms include "lacking ability to transition or switch ideas appropriately with the social context, as evidenced by the repetition of words or gestures after they have ceased to be socially relevant or appropriate", or the "act or task of doing so", and are not better described as stereotypy.

Foix–Chavany–Marie syndrome (FCMS), also known as bilateral opercular syndrome, is a neuropathological disorder characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles of the mouth that aid in chewing. The disorder is primarily caused by thrombotic and embolic strokes, which cause a deficiency of oxygen in the brain. As a result, bilateral lesions may form in the junctions between the frontal lobe and temporal lobe, the parietal lobe and cortical lobe, or the subcortical region of the brain. FCMS may also arise from defects existing at birth that may be inherited or nonhereditary. Symptoms of FCMS can be present in a person of any age and it is diagnosed using automatic-voluntary dissociation assessment, psycholinguistic testing, neuropsychological testing, and brain scanning. Treatment for FCMS depends on the onset, as well as on the severity of symptoms, and it involves a multidisciplinary approach.
Geschwind syndrome, also known as Gastaut-Geschwind, is a group of behavioral phenomena evident in some people with temporal lobe epilepsy. It is named for one of the first individuals to categorize the symptoms, Norman Geschwind, who published prolifically on the topic from 1973 to 1984. There is controversy surrounding whether it is a true neuropsychiatric disorder. Temporal lobe epilepsy causes chronic, mild, interictal changes in personality, which slowly intensify over time. Geschwind syndrome includes five primary changes; hypergraphia, hyperreligiosity, atypical sexuality, circumstantiality, and intensified mental life. Not all symptoms must be present for a diagnosis. Only some people with epilepsy or temporal lobe epilepsy show features of Geschwind syndrome.
A horizontal gaze palsy is a subtype of gaze palsy in which conjugate, horizontal eye movements are limited by neurologic deficits. Horizontal gaze palsies typically result from an ipsilateral pontine lesion or a contralateral frontal lobe lesion.
The palmomental reflex (PMR) or Marinesco-Radovici Sign or Kinn reflex or Marinesco Reflex is a primitive reflex consisting of a twitch of the chin muscle elicited by stroking a specific part of the palm. It is present in infancy and disappears as the brain matures during childhood but may reappear due to processes that disrupt the normal cortical inhibitory pathways. Therefore, it is an example of a frontal release sign.
Sleep-related hypermotor epilepsy (SHE), previously known as nocturnal frontal lobe epilepsy, is a form of focal epilepsy characterized by seizures which arise during sleep. The seizures are most typically characterized by complex motor behaviors. It is a relatively uncommon form of epilepsy that constitutes approximately 9-13% of cases. This disorder is associated with cognitive impairment in at least half of patients as well as excessive daytime sleepiness due to poor sleep quality. This disorder is sometimes misdiagnosed as a non-epileptic sleep disorder. There are many potential causes of SHE including genetic, acquired injuries and structural abnormalities.
Musical hallucinations describes a neurological disorder in which the patient will hallucinate songs, tunes, instruments and melodies. The source of these hallucinations are derived from underlying psychotic illness or hearing impairment. These hallucinations are often rare and are followed by mental decline. A majority of patients who have symptoms of musical hallucinations are older and have onset conditions predisposing them to the disease. While there is no set form of treatment, research has discovered medications and alternative therapies to be successful in alleviating the hallucinations.
The McGill Picture Anomaly Test (MPAT) is a scientific test that was created by Donald O. Hebb of McGill University and N.W. Morton that assists in testing visual intelligence as well as understanding human behavior. The test includes a series of pictures that each show a typical situation but have something out of place in the photo and provides evidence that supports the idea that the right temporal lobe is involved in visual recognition. When patients with lesions to the right temporal lobe were given the MPAT, they were unable to point to the absurdity in the photo and perceived that nothing was out of place. The test is used to measure a cultural comprehension which allows for a basis to then estimate an individual's intelligence. However, this test alone is not enough to accurately give a single score or representation of a person's overall intelligence. The MPAT is not meant to be used across a variety of populations due to the fact that the social norms of varied populations can be tremendously different, causing the results of the test to be indeterminate.
The anti-saccade (AS) task is a way of measuring how well the frontal lobe of the brain can control the reflexive saccade, or eye movement. Saccadic eye movement is primarily controlled by the frontal cortex.

Occipital epilepsy is a neurological disorder that arises from excessive neural activity in the occipital lobe of the brain that may or may not be symptomatic. Occipital lobe epilepsy is fairly rare, and may sometimes be misdiagnosed as migraine when symptomatic. Epileptic seizures are the result of synchronized neural activity that is excessive, and may stem from a failure of inhibitory neurons to regulate properly.
Hyperreligiosity is a psychiatric disturbance in which a person experiences intense religious beliefs or episodes that interfere with normal functioning. Hyperreligiosity generally includes abnormal beliefs and a focus on religious content or even atheistic content, which interferes with work and social functioning. Hyperreligiosity may occur in a variety of disorders including epilepsy, psychotic disorders and frontotemporal lobar degeneration. Hyperreligiosity is a symptom of Geschwind syndrome, which is associated with temporal lobe epilepsy.