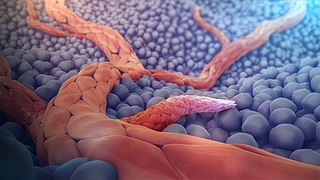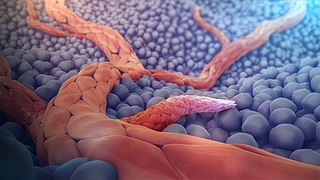
Angiogenesis is the physiological process through which new blood vessels form from pre-existing vessels, formed in the earlier stage of vasculogenesis. Angiogenesis continues the growth of the vasculature mainly by processes of sprouting and splitting, but processes such as coalescent angiogenesis, vessel elongation and vessel cooption also play a role. Vasculogenesis is the embryonic formation of endothelial cells from mesoderm cell precursors, and from neovascularization, although discussions are not always precise. The first vessels in the developing embryo form through vasculogenesis, after which angiogenesis is responsible for most, if not all, blood vessel growth during development and in disease.

A fibroblast is a type of biological cell that synthesizes the extracellular matrix and collagen, produces the structural framework (stroma) for animal tissues, and plays a critical role in wound healing. Fibroblasts are the most common cells of connective tissue in animals.

Fibronectin is a high-molecular weight glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. It is approved for marketing as a topical solution in India by Central Drugs Standard Control organization in 2020 under the brand name FIBREGA for chronic wounds. Fibronectin also binds to other extracellular matrix proteins such as collagen, fibrin, and heparan sulfate proteoglycans.

In biology, the extracellular matrix (ECM), is a network consisting of extracellular macromolecules and minerals, such as collagen, enzymes, glycoproteins and hydroxyapatite that provide structural and biochemical support to surrounding cells. Because multicellularity evolved independently in different multicellular lineages, the composition of ECM varies between multicellular structures; however, cell adhesion, cell-to-cell communication and differentiation are common functions of the ECM.
Connective tissue is one of the four primary types of animal tissue, along with epithelial tissue, muscle tissue, and nervous tissue. It develops mostly from the mesenchyme, derived from the mesoderm, the middle embryonic germ layer. Connective tissue is found in between other tissues everywhere in the body, including the nervous system. The three meninges, membranes that envelop the brain and spinal cord, are composed of connective tissue. Most types of connective tissue consists of three main components: elastic and collagen fibers, ground substance, and cells. Blood, and lymph are classed as specialized fluid connective tissues that do not contain fiber. All are immersed in the body water. The cells of connective tissue include fibroblasts, adipocytes, macrophages, mast cells and leucocytes.

With physical trauma or disease suffered by an organism, healing involves the repairing of damaged tissue(s), organs and the biological system as a whole and resumption of (normal) functioning. Medicine includes the process by which the cells in the body regenerate and repair to reduce the size of a damaged or necrotic area and replace it with new living tissue. The replacement can happen in two ways: by regeneration in which the necrotic cells are replaced by new cells that form "like" tissue as was originally there; or by repair in which injured tissue is replaced with scar tissue. Most organs will heal using a mixture of both mechanisms.

Bone healing, or fracture healing, is a proliferative physiological process in which the body facilitates the repair of a bone fracture.

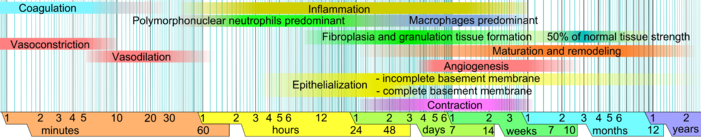
Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.
Haptotaxis is the directional motility or outgrowth of cells, e.g. in the case of axonal outgrowth, usually up a gradient of cellular adhesion sites or substrate-bound chemoattractants. These gradients are naturally present in the extracellular matrix (ECM) of the body during processes such as angiogenesis or artificially present in biomaterials where gradients are established by altering the concentration of adhesion sites on a polymer substrate.

Loose connective tissue, also known as areolar tissue, is a cellular connective tissue with thin and relatively sparse collagen fibers. They have a semi-fluid matrix with lesser proportions of fibers. Its ground substance occupies more volume than the fibers do. It has a viscous to gel-like consistency and plays an important role in the diffusion of oxygen and nutrients from the capillaries that course through this connective tissue as well as in the diffusion of carbon dioxide and metabolic wastes back to the vessels. Moreover, loose connective tissue is primarily located beneath the epithelia that cover the body surfaces and line the internal surfaces of the body. It is also associated with the epithelium of glands and surrounds the smallest blood vessels. This tissue is thus the initial site where pathogenic agents, such as bacteria that have breached an epithelial surface, are challenged and destroyed by cells of the immune system.

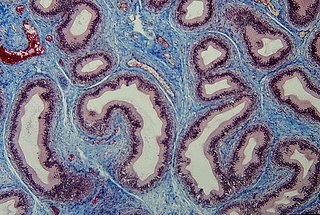
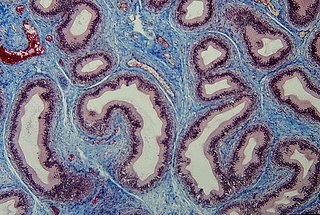
The basement membrane, also known as base membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between epithelial tissues including mesothelium and endothelium, and the underlying connective tissue.
A chronic wound is a wound that does not heal in an orderly set of stages and in a predictable amount of time the way most wounds do; wounds that do not heal within three months are often considered chronic. Chronic wounds seem to be detained in one or more of the phases of wound healing. For example, chronic wounds often remain in the inflammatory stage for too long. To overcome that stage and jump-start the healing process, a number of factors need to be addressed such as bacterial burden, necrotic tissue, and moisture balance of the whole wound. In acute wounds, there is a precise balance between production and degradation of molecules such as collagen; in chronic wounds this balance is lost and degradation plays too large a role.

A myofibroblast is a cell phenotype that was first described as being in a state between a fibroblast and a smooth muscle cell.

Stroma is the part of a tissue or organ with a structural or connective role. It is made up of all the parts without specific functions of the organ - for example, connective tissue, blood vessels, ducts, etc. The other part, the parenchyma, consists of the cells that perform the function of the tissue or organ.

In medicine, desmoplasia is the growth of fibrous connective tissue. It is also called a desmoplastic reaction to emphasize that it is secondary to an insult. Desmoplasia may occur around a neoplasm, causing dense fibrosis around the tumor, or scar tissue (adhesions) within the abdomen after abdominal surgery.
Angiogenesis is the process of forming new blood vessels from existing blood vessels, formed in vasculogenesis. It is a highly complex process involving extensive interplay between cells, soluble factors, and the extracellular matrix (ECM). Angiogenesis is critical during normal physiological development, but it also occurs in adults during inflammation, wound healing, ischemia, and in pathological conditions such as rheumatoid arthritis, hemangioma, and tumor growth. Proteolysis has been indicated as one of the first and most sustained activities involved in the formation of new blood vessels. Numerous proteases including matrix metalloproteinases (MMPs), a disintegrin and metalloproteinase domain (ADAM), a disintegrin and metalloproteinase domain with throbospondin motifs (ADAMTS), and cysteine and serine proteases are involved in angiogenesis. This article focuses on the important and diverse roles that these proteases play in the regulation of angiogenesis.
Acellular dermis is a type of biomaterial derived from processing human or animal tissues to remove cells and retain portions of the extracellular matrix (ECM). These materials are typically cell-free, distinguishing them from classical allografts and xenografts, can be integrated or incorporated into the body, and have been FDA approved for human use for more than 10 years in a wide range of clinical indications.
Dermal fibroblasts are cells within the dermis layer of skin which are responsible for generating connective tissue and allowing the skin to recover from injury. Using organelles, dermal fibroblasts generate and maintain the connective tissue which unites separate cell layers. Furthermore, these dermal fibroblasts produce the protein molecules including laminin and fibronectin which comprise the extracellular matrix. By creating the extracellular matrix between the dermis and epidermis, fibroblasts allow the epithelial cells of the epidermis to affix the matrix, thereby allowing the epidermal cells to effectively join together to form the top layer of the skin.

Diabetic foot ulcer is a breakdown of the skin and sometimes deeper tissues of the foot that leads to sore formation. It may occur due to a variety of mechanisms. It is thought to occur due to abnormal pressure or mechanical stress chronically applied to the foot, usually with concomitant predisposing conditions such as peripheral sensory neuropathy, peripheral motor neuropathy, autonomic neuropathy or peripheral arterial disease. It is a major complication of diabetes mellitus, and it is a type of diabetic foot disease. Secondary complications to the ulcer, such as infection of the skin or subcutaneous tissue, bone infection, gangrene or sepsis are possible, often leading to amputation.
A cancer-associated fibroblast (CAF) is a cell type within the tumor microenvironment that promotes tumorigenic features by initiating the remodelling of the extracellular matrix or by secreting cytokines. CAFs are a complex and abundant cell type within the tumour microenvironment; the number cannot decrease, as they are unable to undergo apoptosis.