Hungary is a landlocked country in Central Europe. Spanning 93,030 square kilometres (35,920 sq mi) of the Carpathian Basin, it is bordered by Slovakia to the north, Ukraine to the northeast, Romania to the east and southeast, Serbia to the south, Croatia and Slovenia to the southwest, and Austria to the west. Hungary has a population of 9.7 million, mostly ethnic Hungarians and a significant Romani minority. Hungarian, the official language, is the world's most widely spoken Uralic language and among the few non-Indo-European languages widely spoken in Europe. Budapest is the country's capital and largest city; other major urban areas include Debrecen, Szeged, Miskolc, Pécs, and Győr.

Tobacco smoking is the practice of burning tobacco and ingesting the resulting smoke. The smoke may be inhaled, as is done with cigarettes, or simply released from the mouth, as is generally done with pipes and cigars. The practice is believed to have begun as early as 5000–3000 BC in Mesoamerica and South America. Tobacco was introduced to Eurasia in the late 17th century by European colonists, where it followed common trade routes. The practice encountered criticism from its first import into the Western world onwards but embedded itself in certain strata of a number of societies before becoming widespread upon the introduction of automated cigarette-rolling apparatus.
A sin tax is an excise tax specifically levied on certain goods deemed harmful to society and individuals, such as alcohol, tobacco, drugs, candies, soft drinks, fast foods, coffee, sugar, gambling, and pornography. In contrast to Pigovian taxes, which are to pay for the damage to society caused by these goods, sin taxes are used to increase the price in an effort to lower demand, or failing that, to increase and find new sources of revenue. Increasing a sin tax is often more popular than increasing other taxes. However, these taxes have often been criticized for burdening the poor and taxing the physically and mentally dependent.
A fat tax is a tax or surcharge that is placed upon fattening food, beverages or on overweight individuals. It is considered an example of Pigovian taxation. A fat tax aims to discourage unhealthy diets and offset the economic costs of obesity.

A non-communicable disease (NCD) is a disease that is not transmissible directly from one person to another. NCDs include Parkinson's disease, autoimmune diseases, strokes, most heart diseases, most cancers, diabetes, chronic kidney disease, osteoarthritis, osteoporosis, Alzheimer's disease, cataracts, and others. NCDs may be chronic or acute. Most are non-infectious, although there are some non-communicable infectious diseases, such as parasitic diseases in which the parasite's life cycle does not include direct host-to-host transmission.

Prevalence of tobacco use is reported by the World Health Organization (WHO), which focuses on cigarette smoking due to reported data limitations. Smoking has therefore been studied more extensively than any other form of consumption.

Healthcare in Europe is provided through a wide range of different systems run at individual national levels. Most European countries have a system of tightly regulated, competing private health insurance companies, with government subsidies available for citizens who cannot afford coverage. Many European countries offer their citizens a European Health Insurance Card which, on a reciprocal basis, provides insurance for emergency medical treatment insurance when visiting other participating European countries.
Health in the United Kingdom refers to the overall health of the population of the United Kingdom. This includes overall trends such as life expectancy and mortality rates, mental health of the population and the suicide rate, smoking rates, alcohol consumption, prevalence of diseases within the population and obesity in the United Kingdom. Three of these, smoking rates, alcohol consumption and obesity are above the OECD average.

Health in Ethiopia has improved markedly since the early 2000s, with government leadership playing a key role in mobilizing resources and ensuring that they are used effectively. A central feature of the sector is the priority given to the Health Extension Programme, which delivers cost-effective basic services that enhance equity and provide care to millions of women, men and children. The development and delivery of the Health Extension Program, and its lasting success, is an example of how a low-income country can still improve access to health services with creativity and dedication.
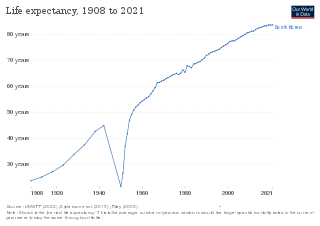
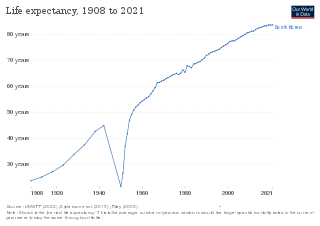
Life expectancy has been rising rapidly and South Korea ranked 3rd in the world for life expectancy. South Korea has among the lowest HIV/AIDS adult prevalence rate in the world, with just 0.1% of the population being infected, significantly lower than the U.S. at 0.6%, France's 0.4%, and the UK's 0.3% prevalence rate. South Korea has a good influenza vaccination rate, with a total of 43.5% of the population being vaccinated in 2019. A new measure of expected human capital calculated for 195 countries from 1920 to 2016 and defined for each birth cohort as the expected years lived from age 20 to 64 years and adjusted for educational attainment, learning or education quality, and functional health status was published by the Lancet in September 2018. South Korea had the sixth highest level of expected human capital with 26 health, education, and learning-adjusted expected years lived between age 20 and 64 years.

The major causes of deaths in Finland are cardiovascular diseases, malignant tumors, dementia and Alzheimer's disease, respiratory diseases, alcohol related diseases and accidental poisoning by alcohol. In 2010 the leading causes of death among men aged 15 to 64 were alcohol related deaths, ischaemic heart disease, accident, suicides, lung cancer and cerbrovascular diseases. Among women the leading causes were breast cancer, alcohol related deaths, accidents, suicides, ischaemic heart disease and lung cancer.

Hungary has a tax-funded universal healthcare system, organized by the state-owned National Health Insurance Fund. While healthcare is considered universal, several reasons persist preventing Hungarian nationals to access healthcare services. For instance, a Hungarian citizen who lived abroad but is unable to show contributions to another country's healthcare system will not be able to access the Hungarian healthcare system free of charge. However, to the OECD, 100% of the total population is covered by universal health insurance, which is absolutely free for children, mothers or fathers with babies, students, pensioners, people with low income, handicapped people, priests and other church employees. In 2022 the cost of public health insurance is 8,400 HUF per month which is the equivalent of $23.69. The healthcare system underwent significant changes which also resulted in improving life expectancy and a very low infant mortality rate. According to the OECD Hungary spent 7.8% of its GDP on health care in 2012. Total health expenditure was $US1,688.7 per capita in 2011, US$1,098.3governmental-fund (65%) and US$590.4 private-fund (35%).

In Finland, the smoking figures are among the lowest in Europe. There are several factors that have influenced the decrease in the smoking prevalence, such as legislative actions, health promotion and national monitoring systems, policies aimed at reducing tobacco consumption through public awareness campaigns, advertising bans and increased taxation. Ministry of Social Affairs and Health has the leading role in tobacco control in Finland, and one of their main aims is have a more effective ban on sale of tobacco products to children and young people and to prevent sale of illegal tobacco products. Among the key elements in the successful tobacco policy is the traditional collaboration between the health authorities and non-governmental organisations, and intensive health promotion.

Crime in Hungary is combated by the Hungarian police and other agencies.
Health in Malta has seen improvements in recent years, with one of the highest life expectancies in Europe. Malta has a good overall quality of health and has seen rapid growth and improvement in key health indicators. Malta has seen significant development in the practice of mental health which has been supported by new infrastructure and increased government health spending. The introduction of health-focused government initiatives, particularly around nutrition, alcohol, smoking, and health will likely contribute to the further improvement of overall health nationwide.
Lebanon is a small middle-income country on the Eastern Mediterranean shore with a population of around 4 million Lebanese citizens, 1.2 million Syrian refugees, and half a million Palestinian refugees. It is at the third stage of its demographic transition characterized by a decline in both fertility and mortality rates. Moreover, Lebanon, like many countries in the Middle East is experiencing an epidemiological transition with an increasingly ageing population suffering from chronic and non-communicable diseases. Mortality related to non-communicable diseases is 404.4 deaths per 100,000 individuals, with an estimate of 45% due to cardiovascular diseases, making them the leading cause of death in Lebanon. Lebanon has health indices that are close to those of more developed countries, with a reported life expectancy at birth of 80.1 years and an under-five mortality rate of 9.5 per 1,000 live births in 2016. Since the end of the 15-year Lebanese Civil War in 1990, Lebanon’s health indicators have significantly improved.

Health in Norway, with its early history of poverty and infectious diseases along with famines and epidemics, was poor for most of the population at least into the 1800s. The country eventually changed from a peasant society to an industrial one and established a public health system in 1860. Due to the high life expectancy at birth, the low under five mortality rate and the fertility rate in Norway, it is fair to say that the overall health status in the country is generally good.
Montenegro is a country with an area of 13,812 square kilometres and a population of 620,029, according to the 2011 census. The country is bordered by Croatia, the Adriatic Sea, Bosnia, Herzegovina, Serbia, Kosovo and Albania. The most common health issues faced are non-communicable diseases accounting for 95% of all deaths. This is followed by 4% of mortality due to injury, and 1% due to communicable, maternal, perinatal and nutritional conditions. Other health areas of interest are alcohol consumption, which is the most prevalent disease of addiction within Montenegro and smoking. Montenegro has one of the highest tobacco usage rates across Europe. Life expectancy for men is 74 years, and life expectancy for women is 79.