3,4-Methylenedioxymethamphetamine (MDMA), commonly known as ecstasy, and molly or mandy, is a potent empathogen–entactogen with stimulant and minor psychedelic properties. Investigational indications include as an adjunct to psychotherapy in the treatment of post-traumatic stress disorder (PTSD) and social anxiety in autism spectrum disorder. The purported pharmacological effects that may be prosocial include altered sensations, increased energy, empathy, and pleasure. When taken by mouth, effects begin in 30 to 45 minutes and last three to six hours.
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that develops from experiencing a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life or well-being. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress, but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.
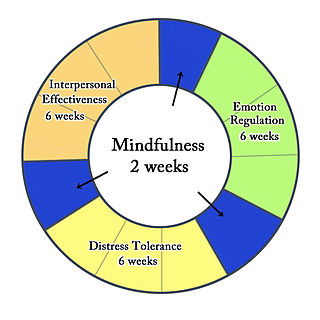
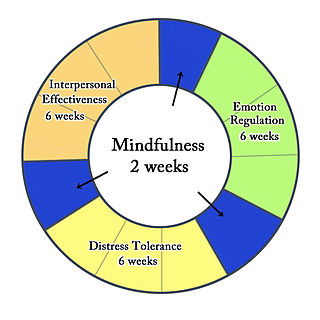
Dialectical behavior therapy (DBT) is an evidence-based psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts. Evidence suggests that DBT can be useful in treating mood disorders and suicidal ideation as well as for changing behavioral patterns such as self-harm and substance use. DBT evolved into a process in which the therapist and client work with acceptance and change-oriented strategies and ultimately balance and synthesize them—comparable to the philosophical dialectical process of thesis and antithesis, followed by synthesis.

Empathogens or entactogens are a class of psychoactive drugs that induce the production of experiences of emotional communion, oneness, relatedness, emotional openness—that is, empathy or sympathy—as particularly observed and reported for experiences with 3,4-methylenedioxymethamphetamine (MDMA). This class of drug is distinguished from the classes of hallucinogen or psychedelic, and amphetamine or stimulants. Major members of this class include MDMA, MDA, MDEA, MDOH, MBDB, 5-APB, 5-MAPB, 6-APB, 6-MAPB, methylone, mephedrone, GHB, αMT, and αET, MDAI among others. Most entactogens are phenethylamines and amphetamines, although several, such as αMT and αET, are tryptamines. When referring to MDMA and its counterparts, the term MDxx is often used. Entactogens are sometimes incorrectly referred to as hallucinogens or stimulants, although many entactogens such as ecstasy exhibit psychedelic or stimulant properties as well.
Psychedelic therapy refers to the proposed use of psychedelic drugs, such as psilocybin, MDMA, LSD, and ayahuasca, to treat mental disorders. As of 2021, psychedelic drugs are controlled substances in most countries and psychedelic therapy is not legally available outside clinical trials, with some exceptions.

Nightmare disorder is a sleep disorder characterized by repeated intense nightmares that most often center on threats to physical safety and security. The nightmares usually occur during the REM stage of sleep, and the person who experiences the nightmares typically remembers them well upon waking. More specifically, nightmare disorder is a type of parasomnia, a subset of sleep disorders categorized by abnormal movement or behavior or verbal actions during sleep or shortly before or after. Other parasomnias include sleepwalking, sleep terrors, bedwetting, and sleep paralysis.
The Multidisciplinary Association for Psychedelic Studies (MAPS) is an American nonprofit organization working to raise awareness and understanding of psychedelic substances. MAPS was founded in 1986 by Rick Doblin and is now based in San Jose, California.
Treatment-resistant depression (TRD) is major depressive disorder in which an affected person does not respond adequately to at least two different antidepressant medications at an adequate dose and for an adequate duration. Inadequate response has most commonly been defined as less than 25% reduction in depressive symptoms following treatment with an antidepressant. Many clinicians and researchers question the construct validity and clinical utility of treatment-resistant depression as currently conceptualized.

In applied psychology, interventions are actions performed to bring about change in people. A wide range of intervention strategies exist and they are directed towards various types of issues. Most generally, it means any activities used to modify behavior, emotional state, or feelings. Psychological interventions have many different applications and the most common use is for the treatment of mental disorders, most commonly using psychotherapy. The ultimate goal behind these interventions is not only to alleviate symptoms but also to target the root cause of mental disorders.
Prolonged exposure therapy (PE) is a form of behavior therapy and cognitive behavioral therapy designed to treat post-traumatic stress disorder. It is characterized by two main treatment procedures – imaginal and in vivo exposures. Imaginal exposure is repeated 'on-purpose' retelling of the trauma memory. In vivo exposure is gradually confronting situations, places, and things that are reminders of the trauma or feel dangerous. Additional procedures include processing of the trauma memory and breathing retraining.
Substituted amphetamines are a class of compounds based upon the amphetamine structure; it includes all derivative compounds which are formed by replacing, or substituting, one or more hydrogen atoms in the amphetamine core structure with substituents. The compounds in this class span a variety of pharmacological subclasses, including stimulants, empathogens, and hallucinogens, among others. Examples of substituted amphetamines are amphetamine (itself), methamphetamine, ephedrine, cathinone, phentermine, mephentermine, tranylcypromine, bupropion, methoxyphenamine, selegiline, amfepramone (diethylpropion), pyrovalerone, MDMA (ecstasy), and DOM (STP).
PTSD or post-traumatic stress disorder, is a psychiatric disorder characterised by intrusive thoughts and memories, dreams or flashbacks of the event; avoidance of people, places and activities that remind the individual of the event; ongoing negative beliefs about oneself or the world, mood changes and persistent feelings of anger, guilt or fear; alterations in arousal such as increased irritability, angry outbursts, being hypervigilant, or having difficulty with concentration and sleep.
The Spring Grove Experiment is a series of lysergic acid diethylamide (LSD) studies performed from 1963 to 1976 on patients with psychotic illnesses at the Spring Grove Clinic in Catonsville, Maryland. These patients were sponsored by the National Institute of Mental Health to be part of the first study conducted on the effects of psychedelic drugs on people with schizophrenia. The Spring Grove Experiments were adapted to study the effect of LSD and psychotherapy on patients including alcoholics, heroin addicts, neurotics, and terminally-ill cancer patients. The research done was largely conducted by the members of the Research Unit of Spring Grove State Hospital. Significant contributors to the experiments included Walter Pahnke, Albert Kurland, Sanford Unger, Richard Yensen, Stanislav Grof, William Richards, Francesco Di Leo, and Oliver Lee McCabe. Later, Spring Grove was rebuilt into the Maryland Psychiatric Research Center where studies continued to be performed for the advancement of psychiatric research. This study on LSD is the largest study on psychedelic drugs to date.

Psilocybin therapy is the use of psilocybin in treating a range of mental health conditions, such as depression, anxiety, addictions, obsessive compulsive disorder, and psychosis. It is one of several forms of psychedelic therapy under study. Psilocybin was popularized as a psychedelic recreational drug in the 1970s and was classified as a Schedule I drug by the DEA. Research on psilocybin as a medical treatment was restricted until the 1990s because of the sociocultural fear of dependence on this drug. As of 2022, psilocybin is the most commonly researched psychedelic due to its safety and low potential for abuse and dependence. Clinical trials are being conducted at universities and there is evidence confirming the use of psilocybin in the treatment of depression, PTSD and end of life anxiety.
Post-traumatic stress disorder (PTSD) can affect about 3.6% of the U.S. population each year, and 6.8% of the U.S. population over a lifetime. 8.4% of people in the U.S. are diagnosed with substance use disorders (SUD). Of those with a diagnosis of PTSD, a co-occurring, or comorbid diagnosis of a SUD is present in 20–35% of that clinical population.
Una D. McCann is a board certified psychiatrist and researcher at Johns Hopkins School of Medicine in the Department of Psychiatry. She is also the Director of the Anxiety Disorders Program, and Co-Director of the Center for Interdisciplinary Sleep Medicine and Research, and Associate Program Director at the Johns Hopkins Bayview Medical Center. McCann is considered to be an expert in anxiety and stress disorders and her primary areas research revolves around amphetamine-induced monoamine neurotoxicity and neurobiology of anxiety disorders.
Psychoplastogens are a group of small molecule drugs that produce rapid and sustained effects on neuronal structure and function, intended to manifest therapeutic benefit after a single administration. Several existing psychoplastogens have been identified and their therapeutic effects demonstrated; several are presently at various stages of development as medications including ketamine, MDMA, scopolamine, and the serotonergic psychedelics, including LSD, psilocin, DMT, and 5-MeO-DMT. Compounds of this sort are being explored as therapeutics for a variety of brain disorders including depression, addiction, and PTSD. The ability to rapidly promote neuronal changes via mechanisms of neuroplasticity was recently discovered as the common therapeutic activity and mechanism of action.
Psychedelic treatments for trauma-related disorders are the use of psychedelic substances, either alone or used in conjunction with psychotherapy, to treat trauma-related disorders. Trauma-related disorders, such as post-traumatic stress disorder (PTSD), have a lifetime prevalence of around 8% in the US population. However, even though trauma-related disorders can hinder the everyday life of individuals with them, less than 50% of patients who meet criteria for PTSD diagnosis receive proper treatment. Psychotherapy is an effective treatment for trauma-related disorders. A meta-analysis of treatment outcomes has shown that 67% of patients who completed treatment for PTSD no longer met diagnostic criteria for PTSD. For those seeking evidence-based psychotherapy treatment, it is estimated that 22-24% will drop out of their treatment. In addition to psychotherapy, pharmacotherapy (medication) is an option for treating PTSD; however, research has found that pharmacotherapy is only effective for about 59% of patients. Although both forms of treatment are effective for many patients, high dropout rates of psychotherapy and treatment-resistant forms of PTSD have led to increased research in other possible forms of treatment. One such form is the use of psychedelics.
Ketamine-assisted psychotherapy(KAP) is the use of prescribed doses of ketamine, the drug, as an adjunct to psychotherapy sessions. KAP shows significant potential in treating mental disorders such as treatment-resistant depression (TRD), anxiety, obsessive–compulsive disorders (OCD), post-traumatic stress disorders (PTSD), and other conditions. It can also be used for those experiencing substance abuse and physical pain. While it is primarily used as a veterinary anaesthetic, ketamine has also been found to have rapid analgesic and hallucinogenic effects, which has sparked interest in its use as an antidepressant. Despite initial trials of its use in the treatment of mental disorders focussing primarily on its antidepressant effects, newer studies are attempting to harness its psychedelic effects to bring about altered states of consciousness, which will augment the adjunct psychotherapy. Ketamine's neuroplasticity-promoting effects strengthen the cognitive restructuring that takes place through traditional psychotherapy, thereby leading to long-lasting behavioural change. KAP offers promising directions for research on new antidepressant alternatives, but is still not sufficiently defined or evaluated as a treatment combination.