Related Research Articles

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. It includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.
Medical privacy, or health privacy, is the practice of maintaining the security and confidentiality of patient records. It involves both the conversational discretion of health care providers and the security of medical records. The terms can also refer to the physical privacy of patients from other patients and providers while in a medical facility, and to modesty in medical settings. Modern concerns include the degree of disclosure to insurance companies, employers, and other third parties. The advent of electronic medical records (EMR) and patient care management systems (PCMS) have raised new concerns about privacy, balanced with efforts to reduce duplication of services and medical errors.

The Health Insurance Portability and Accountability Act of 1996 is a United States Act of Congress enacted by the 104th United States Congress and signed into law by President Bill Clinton on August 21, 1996. It modernized the flow of healthcare information, stipulates how personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and addressed some limitations on healthcare insurance coverage. It generally prohibits healthcare providers and healthcare businesses, called covered entities, from disclosing protected information to anyone other than a patient and the patient's authorized representatives without their consent. With limited exceptions, it does not restrict patients from receiving information about themselves. It does not prohibit patients from voluntarily sharing their health information however they choose, nor does it require confidentiality where a patient discloses medical information to family members, friends, or other individuals not a part of a covered entity.
Medical billing is a payment practice within the United States healthcare system. The process involves the systematic submission and processing of healthcare claims for reimbursement. Once the services are provided, the healthcare provider creates a detailed record of the patient's visit, including the diagnoses, procedures performed, and any medications prescribed. This information is translated into standardized codes using the appropriate coding system, such as ICD-10-CM or Current Procedural Terminology codes—this part of the process is known as medical coding. These coded records are submitted by medical billing to the health insurance company or the payer, along with the patient's demographic and insurance information. Most insurance companies use a similar process, whether they are private companies or government sponsored programs. The insurance company reviews the claim, verifying the medical necessity and coverage eligibility based on the patient's insurance plan. If the claim is approved, the insurance company processes the payment, either directly to the healthcare provider or as a reimbursement to the patient. The healthcare provider may need to following up on and appealing claims.
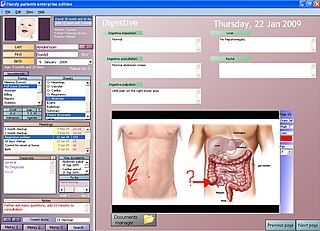
An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.
A personal health record (PHR) is a health record where health data and other information related to the care of a patient is maintained by the patient. This stands in contrast to the more widely used electronic medical record, which is operated by institutions and contains data entered by clinicians to support insurance claims. The intention of a PHR is to provide a complete and accurate summary of an individual's medical history which is accessible online. The health data on a PHR might include patient-reported outcome data, lab results, and data from devices such as wireless electronic weighing scales or from a smartphone.
OSCAR McMaster is a web-based electronic medical record (EMR) system initially developed for academic primary care clinics. It has grown into a comprehensive EMR and billing system used by many doctor's offices and private medical clinics in Canada and other parts of the world. The name is derived from where it was created and an acronym; OSCAR stands for Open Source Clinical Application and Resource and McMaster refers to McMaster University, where it was developed. It enables the delivery of evidence resources at the point of care.

Open Dental, previously known as Free Dental, is an open source dental practice management software licensed under the GNU General Public License. It is written in the C# programming language compatible with Microsoft .NET Framework and was first released in 2003. Current versions of the software require Microsoft Windows, but earlier versions supported other operating systems, including Linux. The full function version is only available under the commercial license because it includes royalty-bearing, licensed materials from the American Dental Association (ADA), the Code on Dental Procedures and Nomenclature (CDT).

First Databank (FDB) is a major provider of drug and medical device databases that help inform healthcare professionals to make decisions. FDB partners with information system developers to deliver useful medication- and medical device-related information to clinicians, business associates, and patients. FDB is part of Hearst and the Hearst Health network.
Patient portals are healthcare-related online applications that allow patients to interact and communicate with their healthcare providers, such as physicians and hospitals. Typically, portal services are available on the Internet at all hours of the day and night. Some patient portal applications exist as stand-alone web sites and sell their services to healthcare providers. Other portal applications are integrated into the existing web site of a healthcare provider. Still others are modules added onto an existing electronic medical record (EMR) system. What all of these services share is the ability of patients to interact with their medical information via the Internet. Currently, the lines between an EMR, a personal health record, and a patient portal are blurring. For example, Intuit Health and Microsoft HealthVault describe themselves as personal health records (PHRs), but they can interface with EMRs and communicate through the Continuity of Care Record standard, displaying patient data on the Internet so it can be viewed through a patient portal.
Health information technology (HIT) is health technology, particularly information technology, applied to health and health care. It supports health information management across computerized systems and the secure exchange of health information between consumers, providers, payers, and quality monitors. Based on a 2008 report on a small series of studies conducted at four sites that provide ambulatory care – three U.S. medical centers and one in the Netherlands, the use of electronic health records (EHRs) was viewed as the most promising tool for improving the overall quality, safety and efficiency of the health delivery system.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
Surgical scheduling software is computer software related to scheduling of tasks for a sequence of surgical cases in one surgery theatre and with one surgery staff using an operational model, a computer and a network. Another vital part of the surgery scheduling process is the communication between the Facility and the Vendor.

The adoption of electronic medical records refers to the recent shift from paper-based medical records to electronic health records (EHRs) in hospitals. The move to electronic medical records is becoming increasingly prevalent in health care delivery systems in the United States, with more than 80% of hospitals adopting some form of EHR system by November 2017.

Medical image sharing is the electronic exchange of medical images between hospitals, physicians and patients. Rather than using traditional media, such as a CD or DVD, and either shipping it out or having patients carry it with them, technology now allows for the sharing of these images using the cloud. The primary format for images is DICOM. Typically, non-image data such as reports may be attached in standard formats like PDF during the sending process. Additionally, there are standards in the industry, such as IHE Cross Enterprise Document Sharing for Imaging (XDS-I), for managing the sharing of documents between healthcare enterprises. A typical architecture involved in setup is a locally installed server, which sits behind the firewall, allowing secure transmissions with outside facilities. In 2009, the Radiological Society of North America launched the "Image Share" project, with the goal of giving patients control of their imaging histories by allowing them to manage these records as they would online banking or shopping.

Intrahealth Systems Limited is a privately held company that develops, licences, supports and sells electronic health record software, medical practice management software, and related services. Founded in Auckland, New Zealand by Dr. Mark Matthews and Dr. Andrew Hall in 1997, they have since moved their headquarters to the City of North Vancouver, British Columbia, Canada in 2005. Apart from the head office, Intrahealth maintains offices in Auckland, New Zealand; Sydney; and Toronto, Canada.
Greenway Health, LLC is a privately-owned vendor of health information technology (HIT) including integrated electronic health record (EHR), practice management, and revenue cycle management solutions. Intergy, Greenway’s cloud-based EHR and practice management solution, serves ambulatory healthcare practices. The company has offices in Tampa, Florida; Carrollton, Georgia; and Bangalore, India.
Home health care software sometimes referred to as home care software or home health software falls under the broad category of health care information technology (HIT). HIT is “the application of information processing involving both computer hardware and software that deals with the storage, retrieval, sharing, and use of health care information, data, and knowledge for communication and decision making” Home health software is designed specifically for companies employing home health providers, as well as government entities who track payments to home health care providers.
Revenue cycle management (RCM) is the process used by healthcare systems in the United States and all over the world to track the revenue from patients, from their initial appointment or encounter with the healthcare system to their final payment of balance. It is a normal part of health administration. The revenue cycle can be defined as, "all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue." It is a cycle that describes and explains the life cycle of a patient (and subsequent revenue and payments) through a typical healthcare encounter from admission (registration) to final payment (or adjustment off of accounts receivables).
Federal and state governments, insurance companies and other large medical institutions are heavily promoting the adoption of electronic health records. The US Congress included a formula of both incentives and penalties for EMR/EHR adoption versus continued use of paper records as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the, American Recovery and Reinvestment Act of 2009.
References
- ↑ "How to select a practice management system". American Medical Association.
- ↑ Terry, Ken "Coding Software Upgrades" Physicians Practice journal, volume 19, number 1, the year 2009, access date July 2, 2009,
- 1 2 3 "Veterinary Software Market Size & Share | Industry Report, 2014-2025". www.grandviewresearch.com. Retrieved 2018-04-04.
- ↑ "Best Veterinary Software | 2018 Reviews of the Most Popular Systems". www.capterra.com. Retrieved 2018-04-04.
- ↑ "Practice management software guide".