Related Research Articles

A respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people who have acute critical conditions, cardiac and pulmonary disease. Respiratory therapists graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC is responsible for credentialing as a CRT, or RRT,
Social work is an academic discipline and practice-based profession concerned with meeting the basic needs of individuals, families, groups, communities, and society as a whole to enhance their individual and collective well-being. Social work practice draws from liberal arts and STEM areas such as psychology, sociology, health, political science, community development, law, and economics to engage with systems and policies, conduct assessments, develop interventions, and enhance social functioning and responsibility. The ultimate goals of social work include the improvement of people's lives, alleviation of biopsychosocial concerns, empowerment of individuals and communities, and the achievement of social justice.

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. The term includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.

The healthcare industry is an aggregation and integration of sectors within the economic system that provides goods and services to treat patients with curative, preventive, rehabilitative, and palliative care. It encompasses the creation and commercialization of products and services conducive to the preservation and restoration of well-being. The contemporary healthcare sector comprises three fundamental facets, namely services, products, and finance. It can be further subdivided into numerous sectors and categories and relies on interdisciplinary teams of highly skilled professionals and paraprofessionals to address the healthcare requirements of both individuals and communities.

A clinic is a health facility that is primarily focused on the care of outpatients. Clinics can be privately operated or publicly managed and funded. They typically cover the primary care needs of populations in local communities, in contrast to larger hospitals which offer more specialized treatments and admit inpatients for overnight stays.
Health psychology is the study of psychological and behavioral processes in health, illness, and healthcare. The discipline is concerned with understanding how psychological, behavioral, and cultural factors contribute to physical health and illness. Psychological factors can affect health directly. For example, chronically occurring environmental stressors affecting the hypothalamic–pituitary–adrenal axis, cumulatively, can harm health. Behavioral factors can also affect a person's health. For example, certain behaviors can, over time, harm or enhance health. Health psychologists take a biopsychosocial approach. In other words, health psychologists understand health to be the product not only of biological processes but also of psychological, behavioral, and social processes.
In China, the practice of medicine is a mixture of government, charitable, and private institutions, while many people rely on traditional medicine. Until reforms in the late twentieth and early twenty-first century, physicians were quasi-government employees and with little freedom in the choice of the hospital to work with. In addition, decades of planned economic policy discouraged physicians from opening their own clinics, and the practice of medicine was generally under the control of local units, such as factories, government, offices, or communes. The reforms created a largely private practice, and physicians now are encouraged to open private clinics and for-profit hospitals.
The psychosocial approach looks at individuals in the context of the combined influence that psychological factors and the surrounding social environment have on their physical and mental wellness and their ability to function. This approach is used in a broad range of helping professions in health and social care settings as well as by medical and social science researchers.
Patient safety is a discipline that emphasizes safety in health care through the prevention, reduction, reporting and analysis of error and other types of unnecessary harm that often lead to adverse patient events. The frequency and magnitude of avoidable adverse events, often known as patient safety incidents, experienced by patients was not well known until the 1990s, when multiple countries reported significant numbers of patients harmed and killed by medical errors. Recognizing that healthcare errors impact 1 in every 10 patients around the world, the World Health Organization (WHO) calls patient safety an endemic concern. Indeed, patient safety has emerged as a distinct healthcare discipline supported by an immature yet developing scientific framework. There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety with mobile health apps being a growing area of research.
A mental health professional is a health care practitioner or social and human services provider who offers services for the purpose of improving an individual's mental health or to treat mental disorders. This broad category was developed as a name for community personnel who worked in the new community mental health agencies begun in the 1970s to assist individuals moving from state hospitals, to prevent admissions, and to provide support in homes, jobs, education, and community. These individuals were the forefront brigade to develop the community programs, which today may be referred to by names such as supported housing, psychiatric rehabilitation, supported or transitional employment, sheltered workshops, supported education, daily living skills, affirmative industries, dual diagnosis treatment, individual and family psychoeducation, adult day care, foster care, family services and mental health counseling.
Case management is a managed care technique within the health care coverage system of the United States. It involves an integrated system that manages the delivery of comprehensive healthcare services for enrolled patients. Case managers are employed in almost every aspect of health care and these employ different approaches in the control of clinical actions.
Patient advocacy is a process in health care concerned with advocacy for patients, survivors, and caregivers. The patient advocate may be an individual or an organization, concerned with healthcare standards or with one specific group of disorders. The terms patient advocate and patient advocacy can refer both to individual advocates providing services that organizations also provide, and to organizations whose functions extend to individual patients. Some patient advocates are independent and some work for the organizations that are directly responsible for the patient's care.
Psychiatric rehabilitation, also known as psychosocial rehabilitation, and sometimes simplified to psych rehab by providers, is the process of restoration of community functioning and well-being of an individual diagnosed in mental health or emotional disorder and who may be considered to have a psychiatric disability.
Health administration, healthcare administration, healthcare management or hospital management is the field relating to leadership, management, and administration of public health systems, health care systems, hospitals, and hospital networks in all the primary, secondary, and tertiary sectors.

Healthcare in South Korea is universal, although a significant portion of healthcare is privately funded. South Korea's healthcare system is based on the National Health Insurance Service, a public health insurance program run by the Ministry of Health and Welfare to which South Koreans of sufficient income must pay contributions in order to insure themselves and their dependants, and the Medical Aid Program, a social welfare program run by the central government and local governments to insure those unable to pay National Health Insurance contributions. In 2015, South Korea ranked first in the OECD for healthcare access. Satisfaction of healthcare has been consistently among the highest in the world – South Korea was rated as the second most efficient healthcare system by Bloomberg. Health insurance in South Korea is single-payer system. The introduction of health insurance resulted in a significant surge in the utilization of healthcare services. Healthcare providers are overburdened by government taking advantage of them.

Nursing is a health care profession that "integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence". Nurses practice in many specialties with varying levels of certification and responsibility. Nurses comprise the largest component of most healthcare environments. Shortages of qualified nurses are found in many countries.

A hospital is a healthcare institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care.
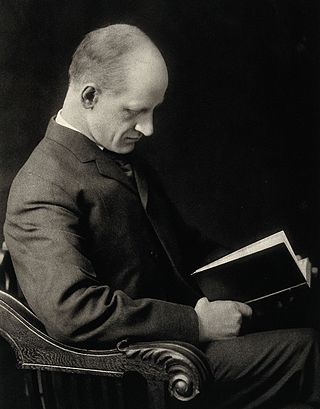
Richard Clarke Cabot was an American physician who advanced clinical hematology, was an innovator in teaching methods, and was a pioneer in social work.

Virginia Margaret Alexander was an American physician, public health researcher, and the founder of the Aspiranto Health Home in Philadelphia, Pennsylvania.

Anne Emily Cummins was an early British medical social worker who was later called the "mother of almoners".
References
- ↑ Jean, Dockhorn (1982). Essentials of social work programs in hospitals. Chicago: American Hospital Association. pp. 1+.
- ↑ A Social Worker's Guide to Professional Practice in Hospitals (PDF). Ordre professionnel des travailleurs sociaux du Québec. 1999. p. 4.
- ↑ "A Complete Guide to Medical Social Work" . Retrieved 2018-09-12.
- ↑ Scesny, Alice M. (1991). Essentials for Directors of Social Work Programs in Health Care. AHA Catalog No. 187104. Chicago, Illinois: American Hospital Association. pp. 30–33. ISBN 0-87258-559-X.
- ↑ Cabot, Richard Clarke (1915). Social Service and the Art of Healing. New York: Moffat, Yard & Co. pp. 32–37.
- ↑ Nottingham, Christ; Dougall, Rona (2007), "A Close and Practical Association with the Medical Profession: Scottish Medical Social Workers and Social Medicine, 1940–1975", Medical History, 51 (3): 309–336, doi:10.1017/S0025727300001460, PMC 1894864 , PMID 17603656
- ↑ Burnham, David (2016), The Social Worker Speaks: A History of Social Workers Through the Twentieth Century, Routledge, pp. 41–43, ISBN 978-1-317-01546-8
- ↑ David Burnham (24 February 2016). The Social Worker Speaks: A History of Social Workers Through the Twentieth Century. Routledge. pp. 43–45. ISBN 978-1-317-01546-8.
- ↑ "Paying for healthcare: Life in Britain before the 'free' NHS".
- 1 2 Lynne M. Healy, International Social Work: Professional Action in an Interdependent World, Oxford University Press, 2001, ISBN 9780195124460, p.24
- ↑ G.R. Madan, Indian Social Problems (Vol-2): Social Disorganization and Reconstruction, Allied Publishers, 1967, ISBN 9788184244601, p.351
- ↑ Kearney, Noreen; Skehill, Caroline (2005), "Chapter 8: An Overview of the Development of Health-Related Social Work in Ireland", Social Work in Ireland: Historical Perspectives, Institute of Public Administration, pp. 165–170, ISBN 978-1-904541-23-3
- ↑ "MOH | Career & Practices".
- ↑ Goh, Soon Noi (2020). "Development of Social Work in Health Care in Singapore". Medical Social Work in Singapore. pp. 3–26. doi:10.1142/9789811227493_0001. ISBN 978-981-12-2748-6. S2CID 225288400.
- ↑ "Home".
- 1 2 Sarah Gehlert, Teri Browne, Handbook of Health Social Work , John Wiley & Sons, 2011, ISBN 9781118115916
- ↑ "Cummins, Anne Emily". Oxford Dictionary of National Biography (online ed.). Oxford University Press. doi:10.1093/ref:odnb/75263.(Subscription or UK public library membership required.)
- ↑ Cannon, Ida M. (1917). Social Work in Hospitals: A Contribution to Progressive Medicine. New York: The Russell Sage Foundation. pp. 6–17.
- ↑ Bracht, Neil F. (1978). Social Work in Health Care: A Guide to Professional Practice. New York: The Haworth Press. pp. 3–18. ISBN 978-0-917724-04-6.