Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. Cognitive behavioral therapy is one of the most effective means of treatment for substance abuse and co-occurring mental health disorders. CBT focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include many issues and the treatment of many mental health conditions, including anxiety, substance use disorders, marital problems, ADHD, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.

Meditation is a practice in which an individual uses a technique – such as mindfulness, or focusing the mind on a particular object, thought, or activity – to train attention and awareness, and achieve a mentally clear and emotionally calm and stable state.
Mind–body interventions (MBI) or mind-body training (MBT) are health and fitness interventions that are intended to work on a physical and mental level such as yoga, tai chi, and Pilates.
Mindfulness is the cognitive skill, usually developed through meditation, of sustaining meta-attention of the contents of one's own mind in the present moment. Mindfulness derives from sati, a significant element of Hindu and Buddhist traditions, and is based on Zen, Vipassanā, and Tibetan meditation techniques. Though definitions and techniques of mindfulness are wide-ranging, Buddhist traditions describe what constitutes mindfulness, such as how perceptions of the past, present and future arise and cease as momentary sense-impressions and mental phenomena. Individuals who have contributed to the popularity of mindfulness in the modern Western context include Thích Nhất Hạnh, Joseph Goldstein, Herbert Benson, Jon Kabat-Zinn, and Richard J. Davidson.
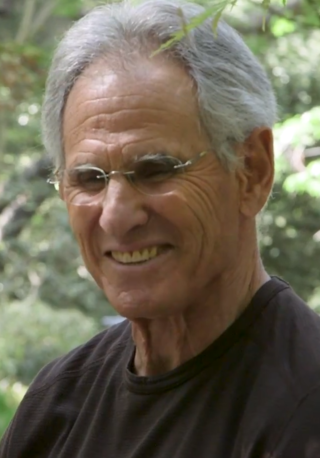
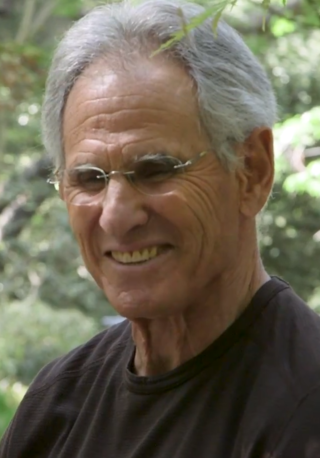
Jon Kabat-Zinn is an American professor emeritus of medicine and the creator of the 'Stress Reduction Clinic' and the 'Center for Mindfulness in Medicine, Health Care, and Society' at the University of Massachusetts Medical School. Kabat-Zinn was a student of Zen Buddhist teachers such as Philip Kapleau, Thich Nhat Hanh, and Seung Sahn, and a founding member of Cambridge Zen Center. His practice of hatha yoga, Vipassanā and appreciation of the teachings of Soto Zen and Advaita Vedanta led him to integrate their teachings with scientific findings. He teaches mindfulness, which he says can help people cope with stress, anxiety, pain, and illness. The stress reduction program created by Kabat-Zinn, mindfulness-based stress reduction (MBSR), is offered by medical centers, hospitals, and health maintenance organizations, and is described in his book Full Catastrophe Living.
Acceptance and commitment therapy is a form of psychotherapy, as well as a branch of clinical behavior analysis. It is an empirically based psychological intervention that uses acceptance and mindfulness strategies along with commitment and behavior-change strategies to increase psychological flexibility.

J. Mark G. Williams, is Emeritus Professor of Clinical Psychology and Honorary Senior Research Fellow at the University of Oxford Department of Psychiatry. He held previous posts at the University of Newcastle upon Tyne, the Medical Research Council Applied Psychology Unit in Cambridge and the University of Wales Bangor, where he founded the Institute for Medical and Social Care Research and the Centre for Mindfulness Research and Practice. He is a Fellow of the British Psychological Society, the Academy of Medical Sciences and the British Academy. He was educated at Stockton Grammar School, Stockton-on-Tees, and at St Peter's College, Oxford. He received an honorary doctorate from the Katholieke Universiteit Leuven on May 8, 2023, in Leuven, Belgium.
John D. Teasdale was a leading researcher at Oxford University, and then in the Cognition and Brain Sciences Unit in Cambridge. He dedicated his focus to understanding the cognition behind depression. Teasdale was a pioneer in the cognitive therapy advancements in the United Kingdom. He was one of the founders of Mindfulness-based Cognitive Therapy, MBCT. He has received many awards to compliment his work and is now retired but still teaching meditation and mindfulness. He has received a Distinguished Scientist Award from the American Psychological Association, and has been elected Fellow of both the British Academy and the Academy of Medical Sciences. He is currently retired, pursuing personal interests in practising and teaching meditation and mindfulness training.

The psychological and physiological effects of meditation have been studied. In recent years, studies of meditation have increasingly involved the use of modern instruments, such as fMRI and EEG, which are able to observe brain physiology and neural activity in living subjects, either during the act of meditation itself or before and after meditation. Correlations can thus be established between meditative practices and brain structure or function.

Buddhism includes an analysis of human psychology, emotion, cognition, behavior and motivation along with therapeutic practices. Buddhist psychology is embedded within the greater Buddhist ethical and philosophical system, and its psychological terminology is colored by ethical overtones. Buddhist psychology has two therapeutic goals: the healthy and virtuous life of a householder and the ultimate goal of nirvana, the total cessation of dissatisfaction and suffering (dukkha).
In psychology, self-compassion is extending compassion to one's self in instances of perceived inadequacy, failure, or general suffering. American psychologist Kristin Neff has defined self-compassion as being composed of three main elements – self-kindness, common humanity, and mindfulness.
Mindfulness-based stress reduction (MBSR) is an eight-week evidence-based program that offers secular, intensive mindfulness training to assist people with stress, anxiety, depression and pain. Developed at the University of Massachusetts Medical Center in the 1970s by Professor Jon Kabat-Zinn, MBSR uses a combination of mindfulness meditation, body awareness, yoga and exploration of patterns of behavior, thinking, feeling and action. Mindfulness can be understood as the non-judgmental acceptance and investigation of present experience, including body sensations, internal mental states, thoughts, emotions, impulses and memories, in order to reduce suffering or distress and to increase well-being. Mindfulness meditation is a method by which attention skills are cultivated, emotional regulation is developed, and rumination and worry are significantly reduced. During the past decades, mindfulness meditation has been the subject of more controlled clinical research, which suggests its potential beneficial effects for mental health, athletic performance, as well as physical health. While MBSR has its roots in wisdom teachings of Zen Buddhism, Hatha Yoga, Vipassana and Advaita Vedanta, the program itself is secular. The MBSR program is described in detail in Kabat-Zinn's 1990 book Full Catastrophe Living.
Occupational therapy is used to manage the issues caused by seasonal affective disorder (SAD). Occupational therapists assist with the management of SAD through the incorporation of a variety of healthcare disciplines into therapeutic practice. Potential patients with SAD are assessed, treated, and evaluated primarily using treatments such as drug therapies, light therapies, and psychological therapies. Therapists are often involved in designing an individualised treatment plan that most effectively meets the client's goals and needs around their responsiveness to a variety of treatments.
Euphoric recall is a cognitive bias that describes the tendency of people to remember past experiences in a positive light, while overlooking negative experiences associated with some event(s). Euphoric recall has primarily been cited as a factor in substance dependence. Individuals may become obsessed with recreating the remembered pleasures of the past, where positive expectancy of outcomes results in the belief that substance use can provide immediate relief.
Relapse prevention (RP) is a cognitive-behavioral approach to relapse with the goal of identifying and preventing high-risk situations such as unhealthy substance use, obsessive-compulsive behavior, sexual offending, obesity, and depression. It is an important component in the treatment process for alcohol use disorder, or alcohol dependence. This model founding is attributed to Terence Gorski's 1986 book Staying Sober.
Metacognitive therapy (MCT) is a psychotherapy focused on modifying metacognitive beliefs that perpetuate states of worry, rumination and attention fixation. It was created by Adrian Wells based on an information processing model by Wells and Gerald Matthews. It is supported by scientific evidence from a large number of studies.
Embodied writing practices are used by academics and artists to highlight the connection between writing and the body, bring consciousness to the cultural implications of academic writing, and inform an understanding of art forms as first person narrative. Embodied writing practices serve as a means to transcend the traditional boundaries of language and communication, inviting individuals to explore the intricate relationship between their physical experiences and the act of writing itself.
Mindfulness-based pain management (MBPM) is a mindfulness-based intervention (MBI) providing specific applications for people living with chronic pain and illness. Adapting the core concepts and practices of mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT), MBPM includes a distinctive emphasis on the practice of 'loving-kindness', and has been seen as sensitive to concerns about removing mindfulness teaching from its original ethical framework. It was developed by Vidyamala Burch and is delivered through the programs of Breathworks. It has been subject to a range of clinical studies demonstrating its effectiveness.

Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness is a book by Jon Kabat-Zinn, first published in 1990, revised in 2013, which describes the mindfulness-based stress reduction (MBSR) program developed at the University of Massachusetts Medical Center's Stress Reduction Clinic. In addition to describing the content and background of MBSR, Kabat-Zinn describes scientific research showing the medical benefits of mindfulness-based interventions (MBIs), and lays out an approach to mind-body medicine emphasizing the depth of the interconnections between physical and mental health. The book has been called "one of the great classics of mind/body medicine", and has been seen as a landmark in the development of the secular mindfulness movement in the United States and internationally.
Willem Kuyken is a British/Dutch scientist, teacher and author. He is the Ritblat Professor of Mindfulness and Psychological Science at the University of Oxford, United Kingdom, and Director of the University of Oxford Mindfulness Centre.