Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. Cognitive behavioral therapy is one of the most effective means of treatment for substance abuse and co-occurring mental health disorders. CBT focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include many issues and the treatment of many mental health conditions, including anxiety, substance use disorders, marital problems, ADHD, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.
Anxiety disorders are a cluster of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal functions are significantly impaired. Anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, easy fatigue, difficulty concentrating, increased heart rate, chest pain, abdominal pain, and a variety of other symptoms that may vary based on the individual.
Eye movement desensitization and reprocessing (EMDR) is a form of psychotherapy that is controversial within the psychological community. It was devised by Francine Shapiro in 1987 and originally designed to alleviate the distress associated with traumatic memories such as post-traumatic stress disorder (PTSD).
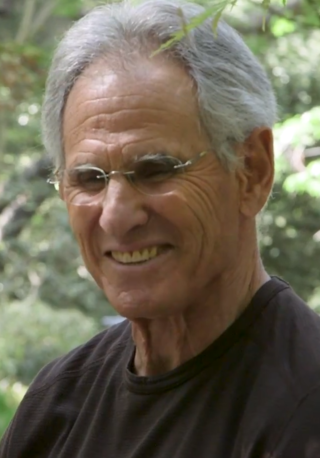
Mindfulness is the cognitive skill, usually developed through meditation, of sustaining meta-attention of the contents of one's own mind in the present moment. Mindfulness derives from sati, a significant element of Hindu and Buddhist traditions, and is based on Zen, Vipassanā, and Tibetan meditation techniques. Though definitions and techniques of mindfulness are wide-ranging, Buddhist traditions describe what constitutes mindfulness such as how past, present and future moments arise and cease as momentary sense impressions and mental phenomena. Individuals who have contributed to the popularity of mindfulness in the modern Western context include Thích Nhất Hạnh, Joseph Goldstein, Herbert Benson, Jon Kabat-Zinn, and Richard J. Davidson.
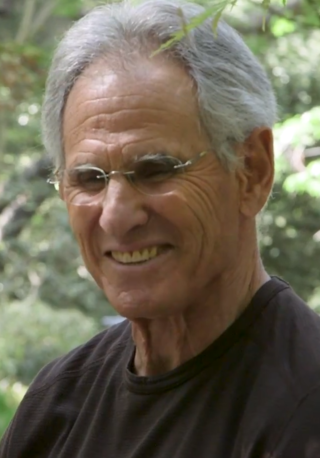
Jon Kabat-Zinn is an American professor emeritus of medicine and the creator of the 'Stress Reduction Clinic' and the 'Center for Mindfulness in Medicine, Health Care, and Society' at the University of Massachusetts Medical School. Kabat-Zinn was a student of Zen Buddhist teachers such as Philip Kapleau, Thich Nhat Hanh, and Seung Sahn, and a founding member of Cambridge Zen Center. His practice of hatha yoga, Vipassanā and appreciation of the teachings of Soto Zen and Advaita Vedanta led him to integrate their teachings with scientific findings. He teaches mindfulness, which he says can help people cope with stress, anxiety, pain, and illness. The stress reduction program created by Kabat-Zinn, mindfulness-based stress reduction (MBSR), is offered by medical centers, hospitals, and health maintenance organizations, and is described in his book Full Catastrophe Living.
Mindfulness-based cognitive therapy (MBCT) is an approach to psychotherapy that uses cognitive behavioral therapy (CBT) methods in conjunction with mindfulness meditative practices and similar psychological strategies. The origins to its conception and creation can be traced back to the traditional approaches from East Asian formative and functional medicine, philosophy and spirituality, birthed from the basic underlying tenets from classical Taoist, Buddhist and Traditional Chinese medical texts, doctrine and teachings.
Psycho-oncology is an interdisciplinary field at the intersection of physical, psychological, social, and behavioral aspects of the cancer experience for both patients and caregivers. Also known as psychiatric oncology or psychosocial oncology, researchers and practitioners in the field are concerned with aspects of individuals' experience with cancer beyond medical treatment, and across the cancer trajectory, including at diagnosis, during treatment, transitioning to and throughout survivorship, and approaching the end-of-life. Founded by Jimmie Holland in 1977 via the incorporation of a psychiatric service within the Memorial Sloan Kettering Cancer Center in New York, the field has expanded drastically since and is now universally recognized as an integral component of quality cancer care. Cancer centers in major academic medical centers across the country now uniformly incorporate a psycho-oncology service into their clinical care, and provide infrastructure to support research efforts to advance knowledge in the field.

The psychological and physiological effects of meditation have been studied. In recent years, studies of meditation have increasingly involved the use of modern instruments, such as fMRI and EEG, which are able to observe brain physiology and neural activity in living subjects, either during the act of meditation itself or before and after meditation. Correlations can thus be established between meditative practices and brain structure or function.

Buddhism includes an analysis of human psychology, emotion, cognition, behavior and motivation along with therapeutic practices. Buddhist psychology is embedded within the greater Buddhist ethical and philosophical system, and its psychological terminology is colored by ethical overtones. Buddhist psychology has two therapeutic goals: the healthy and virtuous life of a householder and the ultimate goal of nirvana, the total cessation of dissatisfaction and suffering (dukkha).
Exposure therapy is a technique in behavior therapy to treat anxiety disorders.
Eastern philosophy in clinical psychology refers to the influence of Eastern philosophies on the practice of clinical psychology.
In psychology, self-compassion is extending compassion to one's self in instances of perceived inadequacy, failure, or general suffering. American psychologist Kristin Neff has defined self-compassion as being composed of three main elements – self-kindness, common humanity, and mindfulness.

In psychology, relaxation is the emotional state of low tension, in which there is an absence of arousal, particularly from negative sources such as anger, anxiety, or fear.
PTSD or post-traumatic stress disorder, is a psychiatric disorder characterised by intrusive thoughts and memories, dreams or flashbacks of the event; avoidance of people, places and activities that remind the individual of the event; ongoing negative beliefs about oneself or the world, mood changes and persistent feelings of anger, guilt or fear; alterations in arousal such as increased irritability, angry outbursts, being hypervigilant, or having difficulty with concentration and sleep.

Meditation and its effect on brain activity and the central nervous system became a focus of collaborative research in neuroscience, psychology and neurobiology during the latter half of the 20th century. Research on meditation sought to define and characterize various practices. The effects of meditation on the brain can be broken up into two categories: state changes and trait changes, respectively alterations in brain activities during the act of meditating and changes that are the outcome of long-term practice.
Metacognitive therapy (MCT) is a psychotherapy focused on modifying metacognitive beliefs that perpetuate states of worry, rumination and attention fixation. It was created by Adrian Wells based on an information processing model by Wells and Gerald Matthews. It is supported by scientific evidence from a large number of studies.
Trauma-sensitive yoga is yoga as exercise, adapted from 2002 onwards for work with individuals affected by psychological trauma. Its goal is to help trauma survivors to develop a greater sense of mind-body connection, to ease their physiological experiences of trauma, to gain a greater sense of ownership over their bodies, and to augment their overall well-being. However, a 2019 systematic review found that the studies to date were not sufficiently robustly designed to provide strong evidence of yoga's effectiveness as a therapy; it called for further research.
Mindfulness-based pain management (MBPM) is a mindfulness-based intervention (MBI) providing specific applications for people living with chronic pain and illness. Adapting the core concepts and practices of mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT), MBPM includes a distinctive emphasis on the practice of 'loving-kindness', and has been seen as sensitive to concerns about removing mindfulness teaching from its original ethical framework. It was developed by Vidyamala Burch and is delivered through the programs of Breathworks. It has been subject to a range of clinical studies demonstrating its effectiveness.

Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness is a book by Jon Kabat-Zinn, first published in 1990, revised in 2013, which describes the mindfulness-based stress reduction (MBSR) program developed at the University of Massachusetts Medical Center's Stress Reduction Clinic. In addition to describing the content and background of MBSR, Kabat-Zinn describes scientific research showing the medical benefits of mindfulness-based interventions (MBIs), and lays out an approach to mind-body medicine emphasizing the depth of the interconnections between physical and mental health. The book has been called "one of the great classics of mind/body medicine", and has been seen as a landmark in the development of the secular mindfulness movement in the United States and internationally.

Mindfulness-Oriented Recovery Enhancement (MORE) is an evidence-based mind-body therapy program developed by Eric Garland. It is a therapeutic approach grounded in affective neuroscience that combines mindfulness training with reappraisal and savoring skills. Garland developed this approach by combining the key features of mindfulness training, "Third Wave" cognitive-behavioral therapy, and principles from positive psychology.